Impact statement
Depression is highly prevalent in people living with HIV (PLWH) and has negative consequences for patient daily life and healthcare. Yet, depression remains mostly underdiagnosed and undertreated in sub-Saharan Africa. In resource-limited settings, such as Senegal, the World Health Organization recommends task-shifting and psychotherapeutic interventions to treat depression. The present study is a first evaluation of the acceptability and feasibility of group interpersonal therapy (IPT) to treat depression in PLWH in Senegal. Groups were facilitated by trained social workers and community health workers. Our results showed that group IPT was well accepted and feasible in this country as treatment for depression in PLWH and that it drastically decreased depression severity and associated disability. As group IPT was administered by non mental health specialists, its success can narrow the gap in mental health treatment. In implementation, some treatment barriers to group IPT’s success and sustainability were identified (e.g., refining identification procedures and bringing services closer to patients). We concluded that group IPT was a promising intervention that could close the mental health treatment gap in Senegal, and we discussed how some measures might transform group IPT into a standard of care for depressed PLWH in the country and, possibly, beyond.
Background
Depression is highly prevalent in sub-Saharan Africa (SSA) and is the most prevalent psychiatric disorder in people living with HIV (PLWH) (Bernard et al., Reference Bernard, Dabis and de Rekeneire2017). It is associated with negative consequences for the quality of life (Abas et al., Reference Abas, Ali, Nakimuli-Mpungu and Chibanda2014) and HIV outcomes (i.e., decreased adherence to antiretroviral therapy (ART), slower increase in CD4 count and rapid progression to AIDS stage) (Berhe and Bayray, Reference Berhe and Bayray2013; Memiah et al., Reference Memiah, Shumba, Etienne-Mesubi, Agbor, Hossain, Komba, Niyang and Biadgilign2014; Wroe et al., Reference Wroe, Hedt-Gauthier, Franke, Nsanzimana, Turinimana and Drobac2015). Despite its negative impact on the continuum of care, depression remains often underdiagnosed and undertreated in SSA (Berhe and Bayray, Reference Berhe and Bayray2013; Abas et al., Reference Abas, Ali, Nakimuli-Mpungu and Chibanda2014).
Evaluating promising models of integrated mental health and HIV care was reported as a research priority in the “treat all” area (Parcesepe et al., Reference Parcesepe, Bernard, Agler, Ross, Yotebieng, Bass, Kwobah, Adedimeji, Goulet and Althoff2018a, Reference Parcesepe, Mugglin, Nalugoda, Bernard, Yunihastuti, Althoff, Jaquet, Haas, Duda, Wester and Nash2018b). Indeed, significant gaps exist in the management of mental disorders in HIV care settings in low- and middle-income countries (LMICs) (i.e., limited screening availability, non systematic screening, limited treatment availability), limiting access to care and treatment (Parcesepe et al., Reference Parcesepe, Bernard, Agler, Ross, Yotebieng, Bass, Kwobah, Adedimeji, Goulet and Althoff2018a, Reference Parcesepe, Mugglin, Nalugoda, Bernard, Yunihastuti, Althoff, Jaquet, Haas, Duda, Wester and Nash2018b). The World Health Organization (WHO) recommends the use of psychological interventions as first-line treatment in LMIC. However, there are many challenges to implementing evidence-based psychotherapeutic treatments, such as lack of mental health specialists, limited resources dedicated to mental health care and poor integration of mental health services (Lancet Global Mental Health Group et al., Reference Chisholm, Flisher, Lund, Patel, Saxena, Thornicroft and Tomlinson2007; WHO, 2010; Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011). In this context, the WHO also encourages task-shifting, an approach that involves the training of non mental health specialists to provide mental health care under the guidance of specialists (Lancet Global Mental Health Group et al., Reference Chisholm, Flisher, Lund, Patel, Saxena, Thornicroft and Tomlinson2007; WHO, 2008). Task-shifting is widely acknowledged as an optimal method to sustain the implementation of psychological interventions (Patel and Thornicroft, Reference Patel and Thornicroft2009; Patel et al., Reference Patel, Maj, Flisher, De Silva, Koschorke, Prince, Zonal and Representatives2010).
The WHO also specifically recommends group interpersonal therapy (group IPT) as a first-line intervention to treat depression in LMICs (WHO, 2016). Developed in the 1970s by Klerman and Weissman (Klerman et al., Reference Klerman, Dimascio, Weissman, Prusoff and Paykel1974) as individual treatment for depression, Interpersonal psychotherapy (IPT) has been successfully adapted to different psychiatric conditions, intervention modalities, age groups, and settings around the world. IPT is based on the idea that depressive symptoms are triggered by interpersonal problems in one or more of the following areas: disagreement or conflict; life changes (negative or positive); grief; loneliness or social isolation (Markowitz and Weissman, Reference Markowitz and Weissman2004; Weissman, Reference Weissman2006; Weissman et al., Reference Weissman, Markowitz and Klerman2018). Patients come to see their depression as a treatable condition within an interpersonal context that can be changed or managed effectively with interpersonal competencies and strategies they learn and apply during the course of treatment; ultimately, they come to resolve the problem area and avert a future relapse. IPT’s effectiveness in treating depression has been reported in two systematic reviews (Cuijpers et al., Reference Cuijpers, Donker, Weissman, Ravitz and Cristea2016, Reference Cuijpers, Geraedts, van Oppen, Andersson, Markowitz and van Straten2011) and with various patient populations, including PLWH (Markowitz et al., Reference Markowitz, Kocsis, Fishman, Spielman, Jacobsberg, Frances, Klerman and Perry1998). IPT was first applied as a group intervention to treat adult depression in Uganda, with encouraging outcomes (Bolton et al., Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman, Ndogoni and Weissman2003; Verdeli et al., Reference Verdeli, Clougherty, Bolton, Speelman, Lincoln, Bass, Neugebauer and Weissman2003a; Bass et al., Reference Bass, Neugebauer, Clougherty, Verdeli, Wickramaratne, Ndogoni, Speelman, Weissman and Bolton2006). Authors reported the benefits of using a group modality (e.g., wider patient coverage and lower implementation costs) (Verdeli et al., Reference Verdeli, Clougherty, Bolton, Speelman, Lincoln, Bass, Neugebauer and Weissman2003a). In a US study with PLWH population, IPT appeared to be the most effective method to treat depression compared to cognitive behavioral and supportive psychotherapy, and equally effective to antidepressants combined with supportive psychotherapy (Markowitz et al., Reference Markowitz, Kocsis, Fishman, Spielman, Jacobsberg, Frances, Klerman and Perry1998). In South Africa, receiving an HIV diagnosis, bereavement (particularly multiple losses due to HIV/AIDS), conflict with family members, and financial stress emerged as triggers for depression (Bana et al., 2009 cited in Petersen et al., Reference Petersen, Bhana and Baillie2012). These triggers are consistent with the problem areas associated with depression in IPT, arguably enhancing its suitability for PLWH. The study also reported a significant improvement in depressive symptoms in PLWH treated with a modified form of group IPT, compared to a control group (Petersen et al., Reference Petersen, Hanass Hancock, Bhana and Govender2014).
Implementation of psychological treatments, however, could be different from one population (or country) to another and might need some cultural adaptation. It also requires specialized training and can increase the workload on staff (Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011; Padmanathan and De Silva, Reference Padmanathan and De Silva2013; Bach-Mortensen et al., Reference Bach-Mortensen, Lange and Montgomery2018). Therefore, examining the acceptability and feasibility of such treatments is crucial, especially in the context of its dissemination through the healthcare system of an entire country. Such evaluation is particularly pertinent in the context of HIV/AIDS, where the “HIV and depression” double burden and high related stigma could reduce adherence to care. A recent study in Ethiopia concluded that group IPT was feasible and acceptable in PLWH (Asrat et al., Reference Asrat, Schneider, Ambaw and Lund2020, Reference Asrat, Lund, Ambaw and Schneider2021). Nonetheless, to our knowledge, there are no data available in West Africa or, more specifically, Senegal.
The Senegalese health system has an extensive experience in psychiatry, but suffers from the scarcity of mental health specialists and inequalities in access to mental health care (Petit, Reference Petit and Charbit2022). In this context, we aimed to assess the acceptability and feasibility of group IPT combined with a task-shifting approach (i.e., group IPT was delivered by trained social or community health workers) to treat PLWH with depression in Senegal. A second aim was to evaluate whether after group IPT, disability and HIV-related stigma decreased compared to baseline scores.
Methodology
Study design
The present study is a part of an ancillary study project within the West Africa network of the International epidemiological Databases to Evaluate AIDS (IeDEA) of the US National Institutes of Health (https://www.iedea.org/regions/west-africa/) (Egger et al., Reference Egger, Ekouevi, Williams, Lyamuya, Mukumbi, Braitstein, Hartwell, Graber, Chi, Boulle, Dabis and Wools-Kaloustian2012). The study took place between October 2019 to March 2022 (end of 3-month follow-ups), with an interruption of 4 months due to the COVID-19 pandemic. In this cross-sectional descriptive study, we compared pre- and post-intervention data (depressive symptoms, functioning and HIV-related stigma) in PLWH treated for depression with group IPT. Assessments were conducted pre-intervention, post-intervention, and at 3-month follow-up.
Setting
The present study was conducted at the Fann National University Hospital Center (FNUHC) in Dakar, the capital and largest city in Senegal (population ~ 4,000,000). The FNUHC is at the top of the healthcare pyramid and is a pioneer in the field of psychiatry in West Africa. The study involved two service units that provide treatment and follow-up for PLWH (~ 2,500 patients): (1) Infectious and Tropical Diseases unit; (2) Outpatient Treatment Center. The psychiatry department contributed two Senegalese psychiatrists to confirm the diagnosis of depression in study participants, and to assist with the management of severe study cases if necessary.
Study population
The source population of our study was PLWH followed in HIV care centers. PLWH were voluntarily screened for depression by a designated clinician at the time of their regular HIV clinical visit to the hospital. To be included, PLWH had to be adults aged ≥20 years, on ART, and identified as “depressed” after being screened with the Patient Health Questionnaire (PHQ-9) (Kroenke et al., Reference Kroenke, Spitzer and Williams2001) by one clinician who works in one of the participating sites on the project. In a second step, patients with a PHQ-9 score ≥ 5 saw a study psychiatrist to confirm during a clinical interview whether they had met the diagnostic criteria for depression. The exclusion criteria were: hospitalization and/or medical emergency; diagnosis with a psychiatric illness other than depression; vision or hearing impairment that would seriously hinder group interactions; and imminent suicide risk. Patients with active suicidal risk were referred to a psychiatrist for further evaluation and intervention.
Ethical approval
The research was conducted in accordance with the Helsinki Declaration. Ethical approval was obtained from Senegal’s ethics committee: Conseil National d’Ethique de la Recherche en Santé (CNERS). All participants gave their written consent prior to participation. Informed consent was obtained in a private room typically reserved for medical visits. All collected data were anonymized.
Group IPT
The intervention was implemented following the WHO manual guidelines, which had been translated to French by our team (https://www.who.int/publications/i/item/WHO-MSD-MER-16.4). Group IPT was delivered over the course of eight weekly group sessions, preceded by one pre-group individual meeting. The eight sessions covered the three phases of treatment: initial, middle, and termination. Groups were gender-specific (facilitator included) and consisted of six patients and one group-facilitator each. Therapy was provided in French and/or in Wolof, Senegal’s national language. The expression “naxaru xol” (literally, “loss of appetite for doing things” in Wolof) was chosen to refer to depression. The term “depression” is less acceptable culturally, as it has connotations with madness.
Group facilitators (i.e., trained staff who lead group IPT groups) were Senegalese social workers (N = 3) or community health workers (N = 1). They had no specialized training on depression or its treatment with psychotherapy. Group facilitators were trained in IPT in two cycles. First, at the end of October 2018, a 3-day training in individual IPT was conducted by two French psychiatrists (T.B., L.J.) from the Cercle de Recherche et d’Etudes Appliquées à la Thérapie InterPersonnelle (CREATIP) association. Following this training, trainees had to conduct IPT with two patients to establish competence. Second, in March 2019, a 5-day training in group IPT was conducted by a master trainer (S.Z.), who is a clinical psychologist. To establish clinical proficiency, the training was followed by two rounds of supervised practice, led by the master trainer, from March to October 2019, where trainees first worked in pairs (cofacilitators) then alone (single facilitator) to provide group IPT to PLWH. Following this training, the study’s implementation phase began in October 2019 in the sites described above. In the course of the study, one of the trained facilitators – a social worker – moved to another service and stopped group facilitation. Group facilitators were supervised by the master trainer (S.Z.) throughout the study phase.
Implementation outcomes
Acceptability
Acceptability is defined as how the patient perceives or reacts to treatment (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth, Petticrew and Guidance2008; Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011; Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011). In the present study, acceptability was assessed by the refusal rate (number of patients with depression who refused to participate in group IPT/number of patients with depression who were invited to participate), and the drop-out rate (number of patients who were included but did not continue to attend group IPT sessions/number of patients who agreed to participate) (Purcell et al., Reference Purcell, Garfein, Latka, Thiede, Hudson, Bonner, Golub and Ouellet2007). Patient satisfaction with this therapy was evaluated using four questions adapted from the Consumer Satisfaction Questionnaire (CSQ-8) (Kapp et al., Reference Kapp, Perlini, Baggio, Stephan, Urrego, Rengade, Macias, Hainard and Halfon2014). Specifically, patients were asked to rate (on a 4-point Likert scale) the quality of the service they received, to see whether it was in line with their expectation and the extent to which the treatment met their needs. They also indicated their general level of satisfaction.
Feasibility
Feasibility is defined as the extent to which an intervention can be provided successfully for a specific population (Bowen et al., Reference Bowen, Kreuter, Spring, Cofta-Woerpel, Linnan, Weiner, Bakken, Kaplan, Squiers, Fabrizio and Fernandez2009; Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011). The feasibility was assessed according to different indicators: attendance of therapy sessions, risk of suicide during group IPT delivery, duration of treatment in practice (i.e., 8 weeks or more) and the time between confirmation of diagnosis and starting group IPT. We also asked facilitators and patients whether they would recommend this therapy to others patients. Finally, facilitators were asked to evaluate the feasibility of group IPT, with a self-administered questionnaire that tapped their satisfaction with group IPT, the ease of its implementation in their daily practice and challenges they might have encountered.
Depressive symptoms, functioning and HIV-related stigma
Depressive symptoms, functioning and HIV-related stigma were assessed by clinicians during follow-up visits (i.e., at the end of group IPT and 3 months later).
The PHQ-9 was used to evaluate the severity of depressive symptoms. Each item was rated on a 4-point Likert scale ranging from 0 to 3. A total score on the PHQ-9 was obtained by summing up the scores on the individual items and could range from 0 to 27. The total score indicated the severity of depressive symptoms: mild (5–9), moderate (10–14), moderately severe (15–19), or severe (≥20). The PHQ-9 is widely used in studies conducted with PLWH in SSA (Wagner et al., Reference Wagner, Holloway, Ghosh-Dastidar, Kityo and Mugyenyi2011; Belenky et al., Reference Belenky, Cole, Pence, Itemba, Maro and Whetten2014; Endeshaw et al., Reference Endeshaw, Walson, Rawlins, Dessie, Alemu, Andrews and Rao2014; Musisi et al., Reference Musisi, Wagner, Ghosh-Dastidar, Nakasujja, Dickens and Okello2014; Asangbeh et al., Reference Asangbeh, Sobngwi, Ekali, Eyoum and Msellati2016) and is recommended for use by the mental health work group of the IeDEA Cohort collaboration (NIMH).
The World Health Organization Disability Assessment Schedule (WHODAS-12) was used to measure general health and disability (Ustün et al., Reference Ustün, Chatterji, Kostanjsek, Rehm, Kennedy, Epping-Jordan, Saxena, von Korff and Pull2010). This 12-item measure uses a 5-point Likert scale (i.e., no difficulty, mild difficulty, moderate difficulty, severe difficulty, extreme difficulty/“cannot do”) to assess functioning across six domains (i.e., cognition, mobility, self-care, getting along, life activities, and participation in community activities). A total score is obtained by summing up item scores and could range from 12 to 60, with higher scores denoting more loss of function. The WHODAS has shown good psychometric properties and was used in several countries (Federici et al., Reference Federici, Bracalenti, Meloni and Luciano2017), particularly with people living with mental illness or chronic disease in Ethiopia (Habtamu et al., Reference Habtamu, Alem, Medhin, Fekadu, Prince and Hanlon2016), Nigeria (Igwesi-Chidobe et al., Reference Igwesi-Chidobe, Kitchen, Sorinola and Godfrey2020), and Ghana (Badu et al., Reference Badu, Mitchell, O’Brien, Osei and Rubin2021).
The 12-item short version of the HIV Stigma Scale was also used to assess HIV-related stigma (Reinius et al., Reference Reinius, Wettergren, Wiklander, Svedhem, Ekström and Eriksson2017). The measure includes 4 stigma subscales (i.e., personalized stigma, disclosure concerns, concerns with public attitudes and negative self-image) of three items and uses a 4-point Likert scale ranging from “strongly agree” to “strongly disagree” to generate a total score. Subscale scores have a possible range of 3–12, with higher scores reflecting more stigma. This short version was created from the Berger Scale (40-item version). It was often used with PLWH in sub-Saharan Africa, including Nigeria (Onyebuchi-Iwudibia and Brown, Reference Onyebuchi-Iwudibia and Brown2014; Secor et al., Reference Secor, Wahome, Micheni, Rao, Simoni, Sanders and Graham2015), Kenya (Kaai et al., Reference Kaai, Bullock, Sarna, Chersich, Luchters, Geibel, Munyao, Mandaliya, Temmerman and Rutenberg2010) and Cameroon (Ajong et al., Reference Ajong, Njotang, Nghoniji, Essi, Yakum, Agbor and Kenfack2018). Shorter versions were validated in Ethiopia (Feyissa et al., Reference Feyissa, Abebe, Girma and Woldie2012) and Tanzania (Ramos et al., Reference Ramos, Mmbaga, Turner, Rugalabamu, Luhanga, Cunningham and Dow2018).
Statistical analysis
The characteristics of the sample were described using median and interquartile range (IQR) for continuous variables and counts and proportion for categorical variables. A comparison of baseline characteristics according to follow-up status (i.e., group IPT completed or not) was performed using the Wilcoxon rank test for continuous variables, and Chi-2 or Exact Fisher Test for categorical variables depending on the tests’ conditions of applications.
Significant improvement of depressive symptoms, disability and HIV-related stigma scores were assessed between (1) inclusion and the end of group IPT and (2) between the end of group IPT and 3 months’ post-treatment, using a general linear mixed model (Tukey–Kramer adjustment) (p < 0.05). Description of the different scores is presented with mean and standard deviation for each visit. The evolution of the PHQ-9 symptoms is presented in an alluvial plot (Rosanbalm, Reference Rosanbalm2015), according to symptom severity. Patient Satisfaction Questionnaire responses and the opinions of the facilitators on feasibility are shown using stacked bars.
Results
Flow chart
In total, 559 PLWH were screened for depression using PHQ-9 and 165 had a PHQ-9 score ≥ 5 (Supplementary Figure S1). Of these 165 patients, 79 had a diagnosis of depression subsequently confirmed by the study’s psychiatrist. Three patients had to be excluded from the study: one had received individual IPT and the other two lived too far away from the clinic and required several hours to commute. Participation in group IPT was offered to 76 patients.
Of the patients invited to participate in the study, two refused to participate in group IPT and three accepted but did not participate in any session, thus limiting the number of participants to 71. Subsequently, the data of two patients were excluded from analysis due to incorrect completion in their consent to participate. Therefore, a total of 69 patients were included in the present study.
In total, 12 IPT groups were formed to treat the study participants. In the course of treatment, nine patients dropped out. One patient completed the initial pre-group meeting, but did not participate in any group sessions (she was subsequently invited to join another group, which she accepted but did not attend). In contrast, 60 patients completed their group IPT treatment. No significant baseline differences were observed between patients who dropped out and those who completed their treatment (Supplementary Table S1). The 69 PLWH attributed their depression to one or more interpersonal problem areas, with primary problems (i.e., those that ranked first) distributed as follows: life changes (52.2%), conflict (36.2%), grief (10.2%) and social isolation (1.4%).
Among the patients who completed group IPT (N = 60), 93.3% attended their follow-up visit at the end of group IPT and 73.3% came to their 3-month post-treatment follow-up. Two patients did not attend their initial follow-up visit at the end of group IPT, but came to their 3-month post-treatment follow-up.
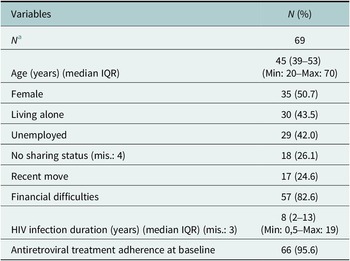
Characteristics of the sample
Sixty-nine PLWH with depression were included in the study. The median age was 45 (interquartile range (IQR): 39–53) (Table 1); 50.7% were female; 43.5% lived alone and 42.0% were unemployed. About a quarter reported that they had not shared their HIV status with anyone (26.1%). A majority reported financial difficulties in the 6 months prior to starting group IPT (82.6%). No patient reported hazardous drinking or drug use. The median duration of HIV infection was 8 years (IQR 2–13), and 95.6% of participants reported 100% ART adherence. None of the participants were prescribed antidepressants at the time of diagnosis with depression, during, or following group IPT implementation.
Table 1. Characteristics of the sample

Note: 71 PLWH agreed to participate in group IPT but 2 patients were subsequently excluded from data analysis due to incorrect completion in their consent to participate.
Abbreviations: IQR, interval interquartile; mis., missing data.
a Including patients who dropped out group IPT.
Acceptability
The refusal rate was 6.6% (2.6% refused to sign the consent form and 3.9% accepted to sign the consent form but did not attend any therapy sessions). The drop-out rate was 12.7%. Dropout occurred after attending the pre-group individual session (one patient) or at least three group sessions (8). The dropout was often justified by a specific reason (e.g., nonpsychiatric hospitalization [1]; leaving the country [1]; flooded home [1]; child custody issue [1]).
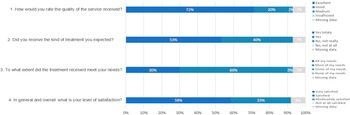
The quality of rendered service was rated as “excellent” or “good” by 92% of participants (Figure 1). The majority reported they received the kind of treatment they had expected (93%) and that group IPT met “all” or “most” of their needs (30 and 60%, respectively). Patient satisfaction with group IPT was high in 91% of participants, with 58% reporting they were “very satisfied” and 33% saying they were “satisfied.”

Figure 1. Patient satisfaction with their participation in group IPT (N = 60).
Feasibility
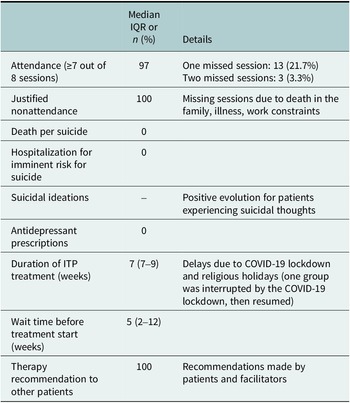
Main feasibility indicators are presented in Table 2. The majority of patients who completed group IPT (97%) had attended at least seven out of eight sessions. Three patients missed two sessions (3.3%), and 13 missed one session (21.7%). Missed sessions were justified (i.e., death in the family, illness, work constraints). At baseline, a number of PLWH who subsequently completed group IPT had reported suicidal ideation; specifically, 4 patients (6.7%) reported suicidal thoughts “more than half of the time” or “almost every day” whereas 19 patients (31.7%) reported suicidal thoughts “several days.” In contrast, upon completion of group IPT, none reported suicidal thoughts “more than half of the time” or “almost every day”; and only 2 patients (3.6%) reported suicidal thoughts “several days.” At their 3-month follow-up, only 5 patients (11.4%) reported suicidal thoughts “several days.”
Table 2. Main feasibility indicators of group IPT in Senegal

Abbreviations: IPT, interpersonal therapy; IQR, interquartile rate.
In the course of group IPT implementation, there were some delays due to COVID-19 lockdown and religious holidays (one group was interrupted by the COVID-19 lockdown, then resumed).
All group facilitators were “very satisfied” with the implementation of group IPT (Supplementary Figure S2) and were either “very satisfied” or “rather satisfied” with the length and frequency of sessions. They all reported that implementing group IPT in their health care routine was not complicated (67% “no, not really” and 33% “no, not at all”). A major difficulty, however, was compliance with group IPT session times; the workload remained nonetheless acceptable. The facilitators’ feedback was mixed on confidentiality management (particularly concerning HIV status) and on patient weekly attendance (i.e., the treatment burden of coming weekly for 8 weeks and associated transportation costs). All the facilitators (100% “yes totally”) and patients (85% “yes totally,” 15% “yes”) said they would recommend group IPT to other patients.
Evolution of PHQ-9, WHODAS and HIV-related scores
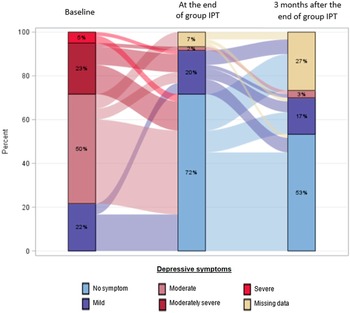
At baseline, 22% of patients had mild depressive symptoms; 50% had moderate symptoms and 28% had moderately severe to severe symptoms (Figure 2). By the end of treatment, only 22% had depressive symptoms (20% mild and 2% moderate, respectively). Three months’ post-treatment, 20% had depressive symptoms (17% mild and 3% moderate, respectively).

Figure 2. Description of the prevalence and the evolution of depressive symptoms according to severity, at baseline, end of group IPT and 3 months after the end of group IPT.
At baseline, the mean PHQ-9 score was 13 (SD = 4) (Table 3). At the end of group IPT, the mean score was 2 (SD = 3). Three months following group IPT, the mean score was 3 (SD = 3). Symptomatic improvement was statistically significant between baseline and completion of group IPT (p < 0.001) (Table 3). The evolution of scores was stable between group IPT completion and subsequent 3-month follow-up. However, 4 patients (7%) with no or mild depressive symptoms at the end of group IPT had moderate symptoms 3 months later, and 1 patient with moderate depressive symptoms at the end of group IPT did not show improvement 3 months later.
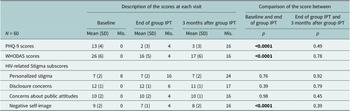
Table 3. Description of the PHQ-9, WHODAS and HIV-related stigma scores at each visit and comparisons of scores across visits

Abbreviation: mis., missing data. p-values in bold indicate significant results (p<0.05).
A significant improvement in WHODAS scores was observed between baseline and the end of group IPT (p < 0.001). However, there was no change in scores between the end of group IPT and 3-month follow-up. Concerning HIV-related stigma, a significant improvement was observed only in negative self-image scores in the time period extending from baseline to group IPT completion (p < 0.001).
Discussion
To our knowledge, the present study constituted the first group IPT implementation in West Africa. The implementation appeared successful and promising in Senegal. Acceptability was high with low refusal rate, moderate drop-out rate and high patient satisfaction. Feasibility appeared good with high session attendance, satisfactory treatment duration and workload for group facilitators. All patients and all facilitators endorsed group IPT, with willingness to recommend it. On the other hand, identification of patients with depression (i.e., delay in group formation) proved challenging and treatment burden of coming weekly for 8 weeks could have been a barrier for some patients. In terms of outcome, patients who completed group IPT had a drastic decrease in depression severity and disability, but no significant reduction of HIV-related stigma except with regard to negative self-image.
Compared to other studies using group IPT, the present study produced comparable or better results in terms of session attendance and patient retention (Bolton et al., Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman, Ndogoni and Weissman2003; Petersen et al., Reference Petersen, Bhana and Baillie2012, Reference Petersen, Hanass Hancock, Bhana and Govender2014; Meffert et al., Reference Meffert, Neylan, McCulloch, Blum, Cohen, Bukusi, Verdeli, Markowitz, Kahn, Bukusi, Thirumurthy, Rota, Rota, Oketch, Opiyo and Ongeri2021). Data on the implementation of other interventions for treating depression among PLWH in sub-Saharan Africa are scarce. One study in Uganda reported promising results from a 8-week group support psychotherapy to treat depression in PLWH. Attrition was also minimal and the majority of the participant attended all the sessions (Nakimuli-Mpungu et al., Reference Nakimuli-Mpungu, Wamala, Okello, Alderman, Odokonyero, Musisi and Mojtabai2014, Reference Nakimuli-Mpungu, Musisi, Wamala, Okello, Ndyanabangi, Birungi, Nanfuka, Etukoit, Mayora, Ssengooba, Mojtabai, Nachega, Harari and Mills2020). However, direct comparisons remain difficult due to different study design. Good acceptability and feasibility may be attributed to various aspects of the study, including cultural adaptation (detailed elsewhere: Ziadeh et al., Reference Ziadeh, Bernard, Ndiaye and Seydiin press). First, the group modality seemed to resonate well with the collectivistic nature of many African cultures (Verdeli et al., Reference Verdeli, Clougherty, Bolton, Speelman, Ndogoni, Bass, Neugebauer and Weissman2003b; Nakimuli-Mpungu et al., Reference Nakimuli-Mpungu, Wamala, Okello, Alderman, Odokonyero, Musisi and Mojtabai2014; Petersen et al., Reference Petersen, Hanass Hancock, Bhana and Govender2014), including Senegal’s. In the context of HIV/AIDS and associated stigma, this is especially pertinent as groups can be powerful means to break social isolation and garner peer support. For PLWH, a group may be more effective than individual counseling (UNAIDS/WHO, 2004) and more helpful than friends and family support (Balmer, Reference Balmer1994). Second, the intervention was implemented within a task-shifting paradigm centered on clinical training and skill building (e.g., drawing on a clear and detailed manual, ongoing supervision), which was critical given that group facilitators had no prior mental health clinical experience. Task-shifting had proved successful in other studies (Dua et al., Reference Dua, Barbui, Clark, Fleischmann, Poznyak, van Ommeren, Yasamy, Ayuso-Mateos, Birbeck, Drummond, Freeman, Giannakopoulos, Levav, Obot, Omigbodun, Patel, Phillips, Prince, Rahimi-Movaghar, Rahman, Sander, Saunders, Servili, Rangaswamy, Unützer, Ventevogel, Vijayakumar, Thornicroft and Saxena2011; Patel et al., Reference Patel, Chowdhary, Rahman and Verdeli2011; Du Zeying et al., Reference Du Zeying, Ashcroft, Kulkarni, Sawrikar and Jackson2022), and could increase treatment accessibility across a country, particularly in rural areas (Nakimuli‐Mpungu et al., Reference Nakimuli‐Mpungu, Musisi, Smith, Von Isenburg, Akimana, Shakarishvili, Nachega, Mills, Chibanda, Ribeiro, Williams and Joska2021). By the same token, it requires more trained staff and a self-sustaining training model (e.g., where facilitators-in-training become supervisors and trainers for future providers).
The present study showed that group IPT was associated with significant and sustainable reduction in depressive symptoms as well as improvement in functioning 3 months post-treatment, in line with other studies but conducted over a longer time period (Bolton et al., Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman, Ndogoni and Weissman2003; Meffert et al., Reference Meffert, Neylan, McCulloch, Blum, Cohen, Bukusi, Verdeli, Markowitz, Kahn, Bukusi, Thirumurthy, Rota, Rota, Oketch, Opiyo and Ongeri2021). Even if those findings need to be viewed with caution given the lack of a control group, they highlight that group IPT had positive impact on the lives of PLWH suffering with depression.
However, PLWH did not experience a positive impact on HIV-related stigma after group IPT (except for self-image). Active ingredients, such as coping skills, social support and behavioral activation, are important for effective mental health (Nakimuli‐Mpungu et al., Reference Nakimuli‐Mpungu, Musisi, Smith, Von Isenburg, Akimana, Shakarishvili, Nachega, Mills, Chibanda, Ribeiro, Williams and Joska2021) and are included in group IPT. In the context of high HIV-related stigma and as stigma impacts depressive symptoms (Nakimuli-Mpungu et al., Reference Nakimuli-Mpungu, Wamala, Okello, Alderman, Odokonyero, Musisi and Mojtabai2014), resilience against stigma should also be considered an active ingredient and included as a component of mental health interventions.
We identified two main barriers to sustainability of group IPT in routine care: (1) difficulties in identifying patients with depression, which led to longer wait times for patients to join their group and, therefore, access treatment; and (2) treatment burden, especially for those living far away from Dakar, particularly due to transportation costs. The COVID-19 pandemic presented additional challenges. The study (conducted during the first 2 years of the pandemic) had to be paused for 4 months following a confinement order issued by the Senegalese government. This had a negative impact on the process of case identification. A number of PLWH balked at the idea of coming to their consultation appointments for fear of being infected with COVID-19 (The Global Fund, 2021). The frail ones might have stayed home, especially when depressed.
One implication for case identification – beyond the effects of a pandemic – is the necessity to systematize and optimize the process, especially that depression screening is not performed routinely in Senegalese HIV care centers. Previous studies conducted in Africa may offer some guidance. In Uganda, the community was involved in identifying patients and spreading information about group support therapy (i.e., they did not use group IPT) (Nakimuli-Mpungu et al., Reference Nakimuli-Mpungu, Wamala, Okello, Alderman, Odokonyero, Mojtabai, Mills, Kanters, Nachega and Musisi2015). In Kenya, patients were recruited through referral or self-referral following informational talks in clinics’ check-in and waiting areas (Meffert et al., Reference Meffert, Neylan, McCulloch, Blum, Cohen, Bukusi, Verdeli, Markowitz, Kahn, Bukusi, Thirumurthy, Rota, Rota, Oketch, Opiyo and Ongeri2021). These strategies may reduce stigma and increase voluntary screening.
Treatment burden is the requirement to attend group sessions over 8 weeks, once a week, which facilitators deemed a bit excessive in terms of time and money commitment, particularly for patients who were employed or who lived far away from the health center. Transportation cost has already been identified as a factor affecting access to treatment in LMICs (Petersen et al., Reference Petersen, Hanass Hancock, Bhana and Govender2014; Meffert et al., Reference Meffert, Neylan, McCulloch, Blum, Cohen, Bukusi, Verdeli, Markowitz, Kahn, Bukusi, Thirumurthy, Rota, Rota, Oketch, Opiyo and Ongeri2021). The dissemination of group IPT to different HIV care centers may help bring treatment closer to patients and reduce transportation costs.
In the context of implementation barriers, there is also the challenge of integrating group IPT into an already operational system, with preexisting tasks and procedures. In the present study, group IPT providers appeared to manage well in the context of task-shifting, as evidenced by their reported satisfaction with the workload and the intervention. Nevertheless, long-term adverse consequences (e.g., worker dissatisfaction, burnout, attrition) cannot be ruled out without a dedicated study.
The present study showed a significant reduction in depressive symptoms and some stability in depression scores post-treatment, suggesting that an 8-week intervention might be sufficient to produce long-term results. On the other hand, for patients who no longer improved or whose condition worsened at the 3-month follow-up, the 8-week intervention might have been too short. We hypothesized that a brief protocol would not permit all patients to develop the necessary skills to get to remission and, in the case of some patients, treatment should be extended. Previous studies with good treatment outcomes (e.g., Uganda study) have typically used a 16-week treatment protocol (Bolton et al., Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman, Ndogoni and Weissman2003). And, in treatment planning, longer interventions may be favored. In this vein, counselors in an Ethiopian study wished to increase the number of sessions (Asrat et al., Reference Asrat, Lund, Ambaw and Schneider2021). On the other hand, increasing the number of sessions can pose a different set of challenges, such as more workload and higher demands on resources, and thus undermine treatment acceptability. In effect, lower treatment attendance can be observed in studies using longer treatment protocols. For example, a 12-week intervention implemented in South Africa (Petersen et al., Reference Petersen, Bhana and Baillie2012) had initially high attendance, but only 50% of patients completed 11–12 treatment sessions.
Apparently, group IPT continues to be helpful beyond the termination session, in that group members go on helping and supporting one another. In Uganda, informal group meetings were reported beyond the 16 weeks of group IPT (Bass et al., Reference Bass, Neugebauer, Clougherty, Verdeli, Wickramaratne, Ndogoni, Speelman, Weissman and Bolton2006). Seemingly, patients used this time for informal counseling, discussing how to tackle their problems and they felt socially and emotionally (Bass et al., Reference Bass, Neugebauer, Clougherty, Verdeli, Wickramaratne, Ndogoni, Speelman, Weissman and Bolton2006). For this reason, perhaps, treatment duration may be less important than cultivating a group culture that is supportive and self-sustaining.
As structural realities in LMICs encourage the use of adapted, brief, structured psychological interventions (Patel et al., Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, McGuire, Rojas and van Ommeren2007), one needs to keep in mind the individual needs of patients. And though group IPT has proved generally helpful to PLWH suffering with depression, the therapeutic scheme and modality still need to be adapted to the patient’s specific needs. For example, individual IPT could be used following group IPT, if a patient expresses the need for it.
Limitations
The present study had a number of limitations. First, the specificity and particularities of the setting – that is, a hospital at the top of the health pyramid, with a dedicated psychiatry department – could have limited the generalizability of these findings. For this reason, the results need to be confirmed in other contexts. Second, some aspects of the acceptability and feasibility were assessed with quantitative measures. In this context, social-desirability bias cannot be ruled out. Third, the feasibility of the intervention from the facilitators’ point of view was only described but not statistically assessed given the limited number of participating staff. Fourth, some aspects of the feasibility (i.e., patients’ experience with group IPT; facilitators’ perception of task-shifting; treatment setting; possible difficulties encountered during the sessions) could not be evaluated in the present study but will be assessed with qualitative interviews in a future study.
Conclusion
Group IPT, conducted in line with the WHO manual and within a task-shifting paradigm, to treat depression in PLWH, showed good acceptability and feasibility and emerged as a promising intervention that could close the mental health treatment gap in Senegal. The intervention’s group modality appeared suitable for Senegal’s culture (i.e., breaking patient isolation and enabling peer-to-peer exchanges). Identified barriers to treatment may be overcome with specific measures, including (1) bringing services closer to patients and making group IPT available beyond Dakar; (2) improving current patient identification procedures and (3) adapting the therapeutic scheme to the specific needs of patients. Such measures may transform group IPT into a standard of care for PLWH with depression across Senegal and beyond.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2023.31.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2023.31.
Data availability statement
The data that support the findings of our study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank the IeDEA West Africa region: Site investigators and cohorts: Adult cohorts: Marcel Djimon Zannou, CNHU, Cotonou, Benin; Armel Poda, CHU Souro Sanou, Bobo Dioulasso, Burkina Faso; Fred Stephen Sarfo, Komfo Anokeye Teaching Hospital, Kumasi, Ghana; Eugene Messou, ACONDA CePReF, Abidjan, Cote d’Ivoire; Henri Chenal, CIRBA, Abidjan, Cote d’Ivoire; Kla Albert Minga, CNTS, Abidjan, Cote d’Ivoire; Emmanuel Bissagnene and Aristophane Tanon, CHU Treichville, Cote d’Ivoire; Moussa Seydi, CHU de Fann, Dakar, Senegal; Akessiwe Akouda Patassi, CHU Sylvanus Olympio, Lomé, Togo. Pediatric cohorts: Sikiratou Adouni Koumakpai-Adeothy, CNHU, Cotonou, Benin; Lorna Awo Renner, Korle Bu Hospital, Accra, Ghana; Sylvie Marie N’Gbeche, ACONDA CePReF, Abidjan, Ivory Coast; Clarisse Amani Bosse, ACONDA_MTCT+, Abidjan, Ivory Coast; Kouadio Kouakou, CIRBA, Abidjan, Cote d’Ivoire; Madeleine Amorissani Folquet, CHU de Cocody, Abidjan, Cote d’Ivoire; François Tanoh Eboua, CHU de Yopougon, Abidjan, Cote d’Ivoire; Fatoumata Dicko Traore, Hopital Gabriel Toure, Bamako, Mali; Elom Takassi, CHU Sylvanus Olympio, Lomé, Togo; Coordinators and data centers: François Dabis, Renaud Becquet, Charlotte Bernard, Shino Chassagne Arikawa, Antoine Jaquet, Karen Malateste, Elodie Rabourdin and Thierry Tiendrebeogo, ADERA, Isped & INSERM U1219, Bordeaux, France. Sophie Desmonde, Julie Jesson and Valeriane Leroy, Inserm 1027, Toulouse, France. Didier Koumavi Ekouevi, Jean-Claude Azani, Patrick Coffie, Abdoulaye Cissé, Guy Gnepa, Apollinaire Horo, Christian Kouadio and Boris Tchounga, PACCI, CHU Treichville, Abidjan, Côte d’Ivoire.
Author contribution
C.B., N.R., F.D., M.S. and N.F.N. designed the study and wrote the protocol. C.B. and H.F. managed and analyzed the data. C.B. wrote the first draft of the manuscript. J.M.T. and A.D. realized the inclusion of the patients and collected the data under the supervision of M.S. and N.F.N. I.N. and O.S. made the diagnosis of depression and supervised the team, as referring psychiatrist. S.Z., H.V., T.B. and L.J. as experts in IPT, trained the team and S.Z. supervised group IPT throughout the project. They helped in the analyses of the data. H.F., N.R. and S.Z. critically reviewed the early draft of the manuscript. All authors critically reviewed and have approved the final manuscript.
Financial support
This work was supported by the National Institute of Mental Health (NIMH), National Cancer Institute (NCI), the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) and the National Institute of Allergy and Infectious Diseases (NIAID) of the U.S. National Institutes of Health (NIH), as part of the International Epidemiologic Databases to Evaluate AIDS (IeDEA) under Award Number U01AI069919. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Competing interest
The authors declare that they have no conflicts of interest.
Ethics statement
This work complies with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.






Comments
Bordeaux
01/06/2023
Dear Editor,
Please find the attached manuscript entitled “Management of depression in people living with HIV in Senegal: acceptability and feasibility of group interpersonal therapy” that we submit to Cambridge Prisms: Global Mental Health for consideration as a Research Article.
Depression is highly prevalent in people living with HIV (PLHIV), and has negative consequences for daily life and care. But in Sub-saharan Africa, depression remains often underdiagnosed and undertreated. In this context, in resource-limited settings, the World Health Organization (WHO) recommends task-shifting and psychotherapeutic treatments to treat depression. We evaluated for the first time the acceptability and feasibility of group interpersonal therapy (group IPT), combined with a task-shifting approach, to treat depression in PLHIV in Senegal. Sixty patients completed group IPT. Groups were facilitated by trained social workers and lay workers and following the WHO manual. With pre and post-treatment evaluations, including a 3-month follow-up, we also evaluated the evolution of depressive symptoms severity, related disability and stigma. Our results showed that group IPT showed good acceptability and feasibility to treat depression in PLHIV in Senegal. group IPT also drastically decreased depression severity and associated disability. We also identified barriers to treatment that are essential to ensure sustainability of this therapy in Senegal. We highlighted that group IPT emerged as a promising intervention that could help to reduce the mental health treatment gap in Senegal. We also discussed how some measures might transform group IPT into a standard of care for depressed PLHIV across Senegal and beyond.
As a Research Article, the content of this submission includes one abstract, one full-text document, three figures, two tables, and a supplementary data file. We certify that all co-authors have seen and approved this manuscript’s content and that it is not under review at any other journal. The authors have no financial interest to declare.
We hope this manuscript will be of interest to your readers and respond to the criteria for publication in Cambridge Prisms: Global Mental Health.
Sincerely yours,
Bernard Charlotte, PhD
Team Global Health in the Global South,
University of Bordeaux, INSERM UMR 1219, IRD EMR 271, BPH,
146 rue Léo Saignat, 33076 BORDEAUX Cedex (FRANCE)
Tél: 05 57 57 56 65, Fax: 05 56 24 00 81
Mail: charlotte.bernard@u-bordeaux.fr