Article contents
Impact of Anti-hypertensive Medication On Psychological Status and Quality of Life in Essential Hypertension
Published online by Cambridge University Press: 15 April 2020
Abstract
Previous findings regarding a possible association among anti-hypertensive medication and dimensions of depressive symptoms, psychopathology and quality of life are mixed.
This study examined whether anti-hypertensive medication impacts on depressive symptoms, psychopathology and quality of life in a sample of hypertensive patients.
Using a prospective design we aimed to explore the psychological status of hypertensive patients both at baseline and one year later.
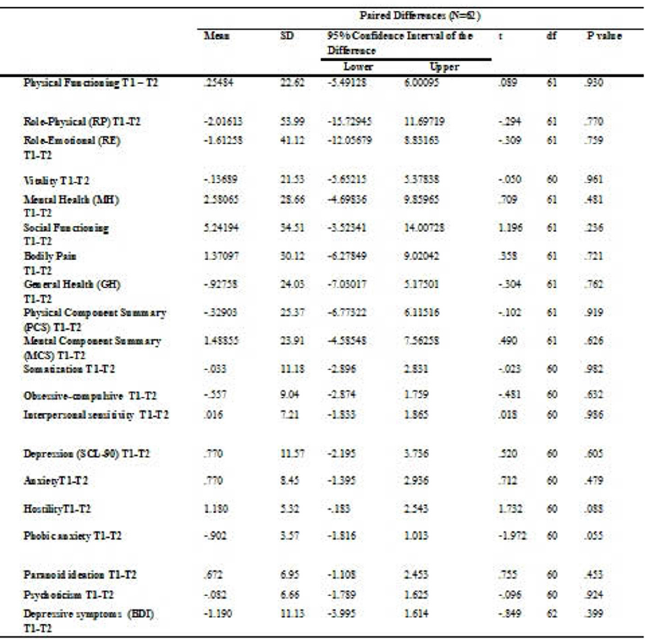
A sample of 198 patients (89 men – 108 women, mean age 52, 9 years, SD = 11, 81 ranged 25-78) with a newly diagnosis of essential hypertension was recruited from a general hospital. The questionnaires included at baseline (T1): a) question for the recording of social-demographic characteristics and clinical features, b) The Short Form 36 (SF-36) General Health Survey questionnaire, c) the Beck Depression Inventory –II (BDI-II), and d) The Symptom Checklist-90-Revised (SCL-90-R). Sixty-two participants completed the SF-36, BDI-II and SCL-90-R again one year later (T2).
Paired t tests showed that there were not significant differences on the psychological measures from baseline to one-year follow-up (Table 1).
Our findings do not support that anti-hypertensive medication has any impact on depression, general psychopathology and quality of life scores than those who use only a dietary program.
- Type
- Article: 0615
- Information
- European Psychiatry , Volume 30 , Issue S1: Abstracts of the 23rd European Congress of Psychiatry , March 2015 , pp. 1
- Copyright
- Copyright © European Psychiatric Association 2015
- 1
- Cited by





Comments
No Comments have been published for this article.