A 48-year-old woman known for Marfan syndrome, with a mechanical valve on anticoagulation, and chronic back pain last treated with lumbar epidural injections 2 years ago presented to a community hospital complaining of severe, non-positional, headaches. She could not recall when she had her last injection. Within hours, her level of consciousness declined precipitously and urgent transfer to our centre was arranged. When she arrived, she was febrile, unable to open her eyes and localised to pain bilaterally (GCS E1V1TM5). CT demonstrated tonsillar herniation, diffuse cerebral sulcal effacement and pseudo-subarachnoid sign. Contrast-enhanced MRI of the brain and spine was ordered to assess for primary differentials of meningitis, venous thromboembolism and spontaneous intracranial hypotension (SIH). This revealed multiple features consistent with SIH (Figure 1A). Imaging also demonstrated known sacral dural ectasia with evidence of newly enlarging meningocele and spinal longitudinal epidural CSF collections (SLECs) (Figure 1B-D). Trendelenburg positioning leads to immediate improvement of her GCS, but gradual elevation of head of bed was not tolerated.

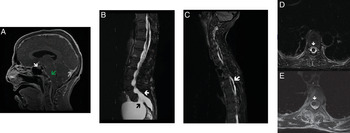
Figure 1: Findings of Intracranial Hypotension with SLECs. (A) Contrast-enhanced MRI of the brain demonstrating multiple features of SIH: enlarged pituitary (white arrow), sagging brainstem (green arrow) and rounding of torcular (grey arrow). (B) Sagittal lumbosacral T2-weighted MRI demonstrating known dural ectasia (white arrow) and enlarging S1 meningocele (black arrow). (C) Sagittal T2 MRI demonstrating thoracic SLECs (white arrow). (D) Axial T2-weighted MRI at T8 level demonstrates a SLEC (white arrow). (E) Following EBP, clinical improvement and resolution of the SLEC were seen (white arrow) with unrelated flow artefact lateral to cord.
In the context of active anticoagulation, we relied on the presence of SLECs to hypothesise that the dural defect lays at, or medial to, the neural foramen and would therefore likely be responsive to epidural blood patch (EBP). Anticoagulation was briefly paused to facilitate this procedure, which lead to sustained clinical improvement and resolution of SLECs (Figure 1E). The patient was discharged home headache-free 10 days after initial presentation.
Approximately 15% of patients with SIH suffer from underlying connective tissue disorders such as Marfan syndrome, and up to 94% are initially misdiagnosed. Reference Mokri, Maher and Sencakova1,Reference Schievink2 CSF leaks contributing to SIH have been classified into four subtypes: I. Ventral dural tear, II. Proximal nerve root sleeve dehiscence, III. CSF-venous fistula or IV. Extravasation from distal root sleeve (e.g. into enlarging meningocele). Reference Schievink, Maya and Jean-Pierre3 In our patient, it was unclear whether the cause was a ventral tear that could respond to EBP (type I/II) or tear within her meningocele sleeve (type IV), which would require surgical repair (Figure 1B). Although invasive myelography is often pursued, the presence of SLECs strongly favours a type I/II tear responsive to EBP. Reference Farb, Nicholson and Peng4 In order to minimise pauses in anticoagulation, we elected to pursue upfront EBP based on non-invasive imaging. Symptom resolution following this procedure strongly supports our pre-intervention hypothesis.
Treatment options for intracranial hypotension include hydration, flat or Trendelenburg positioning, EBP and more rarely a variety of options for surgical repair. Reference Schievink2 In our case, misinterpretation of clinical exam and CT findings of tonsillar herniation, diffuse cerebral sulcal effacement and pseudo-subarachnoid sign may have led to diagnosis of, and intervention for, raised intracranial pressure which can be harmful in SIH. Although two potential aetiologies could have explained SIH in our patient, SLECs strongly supported a dural defect amenable to EBP (type I/II) rather than collection into her enlarging meningocele (type IV), avoiding the need for invasive myelography, potential surgical repair and protracted periods without anticoagulation. Clinicians and trainees should be aware of the diagnostic value of SLECs, novel MR biomarkers for SIH that may predict responsiveness to EBP.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
SKK planned and conceived the manuscript. NMW wrote the paper, performed literature review and developed the figure. RIF and SKK provided critical review of the manuscript and figure and approved the final version of this work.