Introduction
Pituitary adenomas (PAs) are a common heterogeneous group of tumors arising in the pituitary gland with a reported incidence as high as 16.7%. They are often asymptomatic and are detected incidentally on imaging. Some PAs can secrete hormones that lead to a clinical syndrome, while others, even if not biochemically functional, can manifest via hormone hypo-secretion or compressive effects due to their anatomic proximity to critical neural and vascular structures. Reference Ezzat, Asa and Couldwell1
Management of PA often requires a multidisciplinary approach that can include surgical, medical, and radiation therapies. Long-term coordination of care between specialists such as endocrinologists, neurosurgeons, otolaryngologists, radiation oncologists, and ophthalmologists is often necessary. While a multidisciplinary team approach to healthcare delivery has been associated with improved patient outcomes, increased patient satisfaction, Reference Alexander, Lichtenstein, Jinnett, Wells, Zazzali and Liu2 improved resource utilization, Reference Hanson, Deutschman and Anderson3 and decreased mortality, Reference Kim, Barnato, Angus, Fleisher and Kahn4 this type of complex care pathway can be challenging for patients to navigate and has the potential for inefficiencies, and increased morbidity due to a lack of proper communication and increased risk for human error. Reference Bracco, Favre and Bissonnette5,Reference Frandsen, Joynt, Rebitzer and Jha6
“Multidisciplinary” care has been said to utilize the skills and experiences of individuals from different disciplines, with each discipline approaching the patient from their own perspective, Reference Jessup7 but the contribution of the patients in directing their care pathway is often overlooked. In a 2001 report, the Institute of Medicine included patient-centeredness as one of the six core aims for healthcare. Reference Leape, Berwick and Clancy8 Recently, the province of Ontario launched the Minister’s Patient and Family Advisory Council, a formal advisory body that provides advice and recommendations to the Minister of Health and Long-Term Care on matters relating to patients, families, caregivers, and health system priorities. This group released a “Patient Declaration of Values for Ontario”, which issues several statements regarding patient involvement including the expectation that patients will be recognized as part of the care team and that patients “expect a health care culture that values the experiences of patients, families and caregivers and incorporates this knowledge into policy, planning and decision making”. 9
Patient-centered care is a goal that is widely adopted but is often only realized on an individual patient level as shared decision-making during medical encounters. Integrating a patient-directed approach in the development of quality initiatives may be a means of ensuring the goals and outcomes that are meaningful for patients are incorporated into programs. There is increasing recognition of the benefits of patients co-designing healthcare such as identifying care gaps, areas for improvement, defining how services should be provided and educational information development and dissemination. Reference Groene and Sunol10
A review of the care of PA care management at our institution revealed some inconsistencies in the care process and opportunities for improvement. We describe a patient-led quality improvement initiative to improve and streamline care of patients with PA undergoing surgery at our center via the implementation of a multidisciplinary PA care pathway.
Study Design and Methods
Study Setting and Participants
The Ottawa Hospital (TOH) is multi-campus academic teaching hospital located in Ottawa, Ontario and serves a catchment area of 1.3 million people. Over 100 patients are seen annually in the multidisciplinary pituitary clinic and over 30 pituitary surgeries are performed.
We conducted a retrospective chart review on patients with PA before and after quality improvement intervention. Patients were identified based on billing codes of consultations performed by Endocrinologists and by review of the database of new referrals gathered by administrative staff at the multidisciplinary pituitary clinic.
This study was conducted in accordance with The Ottawa Health Science Network Research Ethics Board’s regulations for quality improvement projects. Funding for this project was provided by the University of Ottawa, Department of Medicine Patient Quality and Safety Grant.
Intervention Development and Implementation
A multidisciplinary committee consisting of key stakeholders in Endocrinology and Metabolism, Neurosurgery, and Nursing was convened to review the current state of pituitary care and review literature for best practices. A patient advisory committee was established to understand the patient experience and patient-identified areas in need of improvement. Eleven advisors participated: 9 patients and 2 spouses, 6 of whom were male. The ages ranged from 36 to 65 years and the patients were a median of 14.1 months (range 4–30) out from surgery. Five of the patients had required multiple surgeries and seven of them were receiving hormone replacement post-operatively. Participants in the advisory committee were identified via purposeful sampling. Inclusion criteria for the advisory committee were adult patients with PA who underwent surgery, PA surgery within the past 2 years, clinically well enough, and cognitively able to participate. Consent and confidentiality forms were signed by the participants. Experience-based design, originally developed by the National Institute of Health, was used to guide the process. The approach captures the experiences of those involved in healthcare services looking at the care and emotional journey people experience. Reference Bate and Robert11 The session consisted of open-ended questions to gain patient perspectives on key areas of the patient journey.
The members of the patient advisory committee identified “touchpoints” – experiences that resulted in very strong positive or negative feelings along with the following themes: clinic flow, treatment journey, and partnerships/level of patient/family involvement in planning and decision-making. Despite the heterogeneous patient journey, the advisory committee identified five improvement themes:
-
1) Integration of care: Enhancement of system navigation and communication between team members in the peri-operative period.
-
2) Timely access to information: Improvement of access to information to prepare patients and family members better.
-
3) Support strategies: Development of strategies to meet emotional and supportive care needs such as group learning and peer support activities.
-
4) Individualized plan: Establishment of a process for undertaking comprehensive needs assessment and developing a patient-specific plan of care.
-
5) Minimize follow-ups: Identify opportunities to use technology and enhance visit coordination to minimize the number of follow-ups.
In response to the five areas of need identified by the patient advisory committee, several changes were implemented. A central triage process to streamline access to the appropriate care for patients was developed (Figure 1). It included criteria for urgency and referral to the joint Endocrinology and Neurosurgery pituitary clinic (Multidisciplinary Clinic). Our center already had a Multidisciplinary Clinic, but access was limited as it was held only once per month. The frequency of the clinic was increased to every second week to address themes 1, 4, and 5.
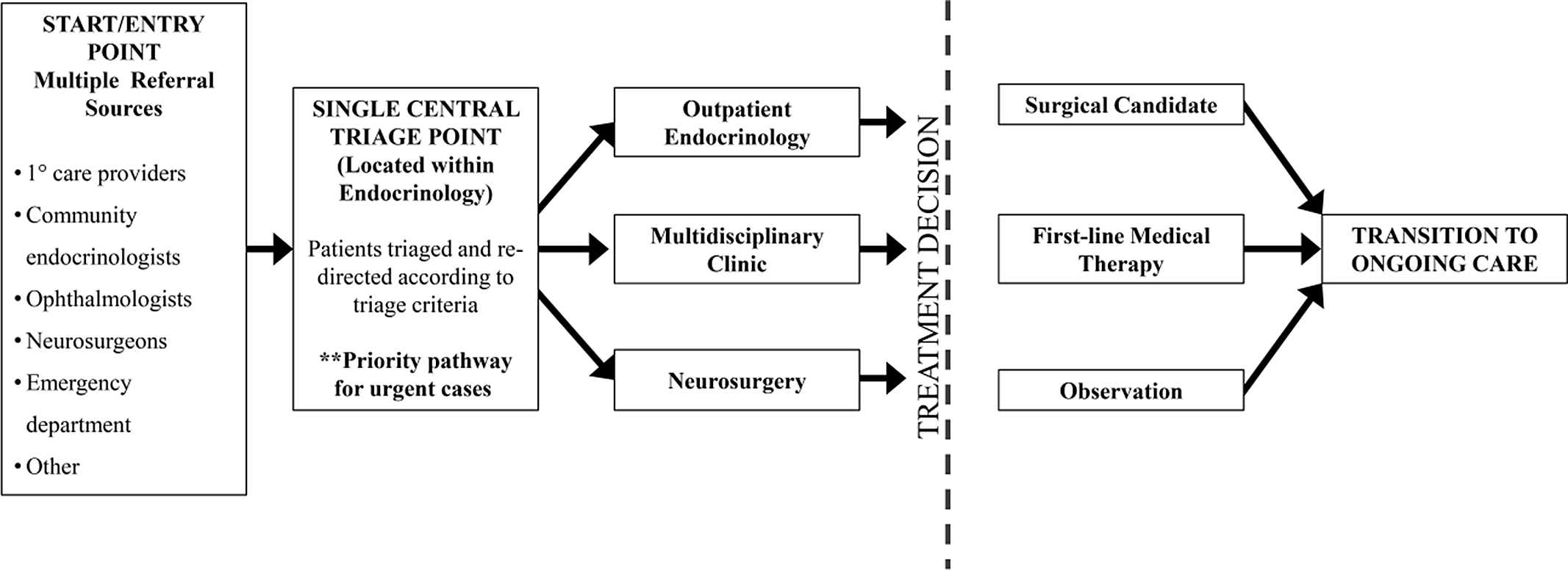
Figure 1: High-level desired end-stage process map for triage. 1° = Primary; ** = does not denote significance but indicates that cases deemed as urgent are not triaged according to this process.
To address the needs for timely access to information and peer support (themes 2 and 3) the following strategies were undertaken: development of a patient-information booklet, creation of semi-annual patient information night, and vetted and endorsed web-based patient educational material. Reference Druce, Williams, Baggoo, Keely and Malcolm12 The patient information night included presentations from healthcare professionals describing the anticipated patient journey, videos of surgical processes, and patients sharing their experience.
These particular changes were chosen mainly due to their low cost, feasibility, and potential impact. The centralized triage criteria were implemented as it is low-cost and had the potential to limit duplicate referrals (i.e. referral from Neurosurgery to Endocrinology and vice versa), thus being cost-saving. Additional clinic time was possible as the model and funding for the clinic were already in place, all that was required was the securing of additional personnel. This intervention was felt to have the greatest potential impact on patient care as it doubled the available clinic time allowing for a greater number of patients to be assessed, potentially decreasing the wait time for assessment. The creation of a patient booklet and review of existing web-based information was chosen as it also required a one-time low-cost intervention which could have long-term benefits for patients through access to reliable healthcare information. The education night was the most labor and cost-intensive intervention it was pursued due to its potential patient impact, allowing patients, and their families, access to the clinicians outside of the exam room and also introduced future patients to those who had already experienced the journey of care. This allowed for the potential creation of support networks and data exchange.
Study Populations
All adult patients, >18 years of age, with newly diagnosed PA during two time periods [March 1, 2012 to February 28, 2013 (pre-intervention) and July 1, 2016 to June 30, 2017 (post-intervention)] were included in this study. The interventions were implemented in May 2015. Cases involving other pituitary lesions (e.g. Rathke’s cleft cyst) and repeat treatment for previously diagnosed lesions were excluded.
Outcome Measures
This was a pre- and post-intervention analysis. In each cohort, data collected included patient demographics, the location of initial assessment, the type and size of adenoma, imaging and biochemical testing, wait times from diagnosis and referral to assessment and surgical treatment (if indicated), surgical outcomes for patients treated with surgery, time to follow-up assessment, imaging, and biochemical testing and finally, communication with other care providers.
Statistical Analysis
The normalcy of distribution of continuous data was assessed with the Shapiro–Wilk test. Normally distributed variables were expressed as a mean and compared with Student’s T-test. Non-normally distributed data were expressed as a median and compared with the Mann–Whitney U-test. Categorical data were compared with Fisher’s exact test. A p-value of <0.05 was considered statistically significant. All statistical analysis was performed with the SPSS Statistics software.
Results
Sixty-eight patients were identified in each of the pre-specified time period. After exclusion, 34 patients were identified in the pre-cohort and 35 in the post-cohort (Figure 2).
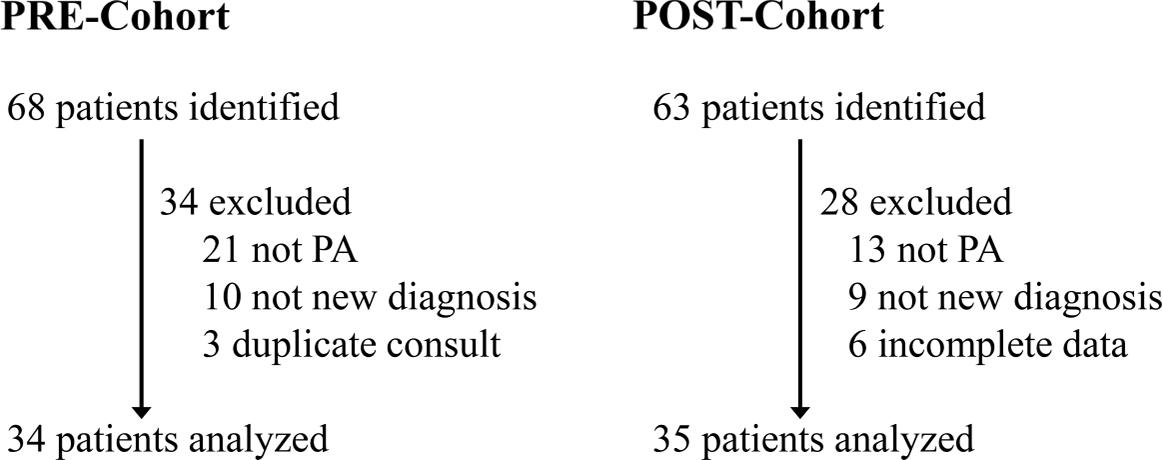
Figure 2: Flow diagram of patient identification.
The patient demographics of the two populations were similar (Table 1). There was no statistical difference between the type (functioning vs. non-functioning) and size of the lesion. There were no adrenocorticotropic hormone-secreting adenomas identified in either cohort. More patients were treated surgically in the post-cohort, but the difference was not statistically significant (p = 0.140). No patients were treated with radiation.
Table 1: Demographics of study population

GH=growth hormone; TSH=thyrotropin secreting hormone.
Microadenoma <10 mm, macroadenoma 10–40 mm, giant adenoma >40 mm.
Process Outcomes
Our intervention resulted in a shift in the location of the first assessment and a change in referral patterns. Post-intervention, patients were primarily being assessed in the Multidisciplinary Clinic vs. other clinics (community or academic center Endocrinology clinics, Neurosurgery clinics; 26% vs. 63%; p = 0.036). In the Multidisciplinary Clinic, patients were assessed by Endocrinology and Neurosurgery simultaneously, and as a result, the number of referrals from Neurosurgery to Endocrinology decreased from 38% to 6% (p = 0.001). We concomitantly saw an increase in the number of referrals from primary care providers from 18% to 46% (p = 0.02). These data reflect the effectiveness of the triaging process.
There was also improved communication with other care providers, identified as the frequency with which consultation letters were being copied to other physicians. Copies to primary care providers increased from 70.6% to 100% (p < 0.001) and copies to Neurosurgery went from 29.4% to 91.4% (p < 0.001).
Clinical Outcomes
There was a trend toward a decrease in wait times for the first assessment following the intervention. None of the decreases were statistically significant (Figure 3).
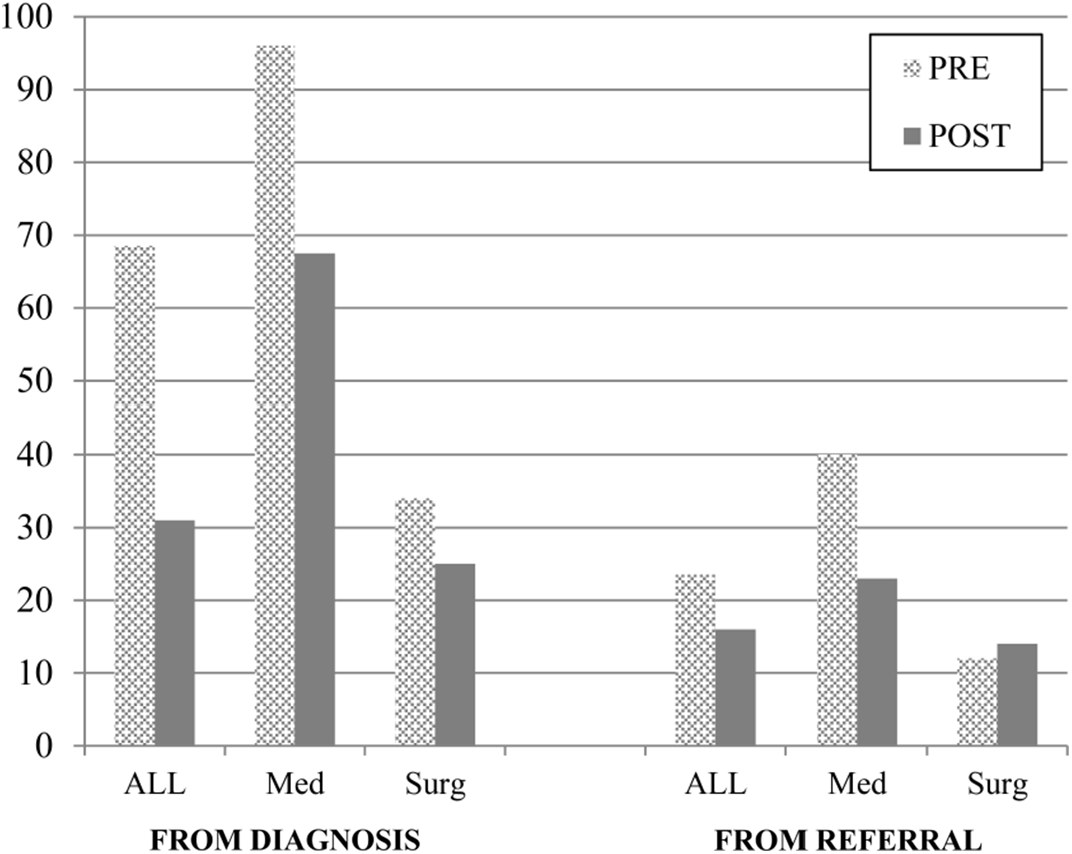
Figure 3: Median wait time, in days, from diagnosis and from referral to the first assessment before and after intervention. ALL=total cohort; Med=patients treated medically or with observation; Surg=patients treated surgically. None of the changes were statistically significant therefore
p-values not shown.
For the surgical cohort, there was also a trend toward a decrease in wait time from diagnosis and referral to surgery (median 90.5 vs. 76 days from diagnosis, 81 vs. 63 days from referral); however, these changes were not statistically significant.
There was no difference between cohorts with respect to the type of imaging modality used or biochemical work-up performed. The number of post-treatment imaging scans increased post-intervention (a median of 2 vs. 3, p = 0.003). The time to follow-up imaging increased post-intervention for the medical group (a median of 110.5 vs. 214.5 days, p = 0.061) and the surgical group (a median of 105.5 vs. 124 days, p = 0.726). However, this may have been a reflection of challenges accessing imaging at our center at the time of the study.
Balancing Outcomes
The time to first follow-up increased post-intervention. In the group who had undergone surgical treatment for PA, the median number of days after surgery to reassessment by Endocrinology went from 28 to 39 days (p = 0.263) and the first follow-up imaging scan post-surgery lengthened from a median of 105.5 to 124 days (p = 0.726). In the medically treated group, the interval to first follow-up was not quantified, but the time to first follow-up scan increased from 110.5 to 214.5 days (p = 0.061).
Patient Satisfaction with Patient Educational Materials
Formal evaluations were completed after the patient information nights. Out of 70 patients surveyed, 63 patients (90%) rated the evening as excellent or very good and 61/70 (87%) would recommend the session to a friend. The education booklet was not formally evaluated, but informal feedback was positive.
Discussion
Our study was a pre- and post-analysis of a quality improvement initiative in the care of PA in a Canadian tertiary care center. To our knowledge, it is the first study to outline the success of a patient-inspired quality improvement initiative to integrate care for PA. The intervention involved expanding and streamlining care delivered at a multidisciplinary pituitary clinic in response to the patient-identified need for efficient and personalized care and resulted in decreased wait times for the first assessment for patients and better communication amongst treating services and care providers. Based on our experience and preliminary data, we would recommend this approach, but understand that there may be limitations with regards to specialist availability, funding and time.
The primary barriers to implementation were funding for additional clinic time and physician availability. Our center is sufficiently large that there are multiple neurosurgeons and endocrinologists who were able to staff the clinic. In smaller centers, where the number of available specialists is limited, this approach may not be feasible. Although a cost analysis has not been undertaken, it is anticipated that the implementation of a Multidisciplinary Clinic may be in fact cost-saving for an institution as it eliminates the need for multiple visits to separate specialists. It is postulated that multidisciplinary care should be cost-effective, but it has to be offset by the cost of organizing, administering, and attending it and research into this area has shown mixed results with regards to cost-effectiveness. Reference Ke, Blazeby, Strong, Carroll, Ness and Hollingworth13 One study used modeling to try and predict the cost-effectiveness of multidisciplinary care in chronic kidney disease – they found that multidisciplinary care was generally more cost-effective in patients with more advanced disease, but those who had milder disease stood to benefit more with regards to improvement in their health with the intervention. Reference Lin, Chertow, Yan, Malcolm and Goldhaber-Fiebert14
While it is recognized that patient and public involvement in quality improvement can be beneficial, documentation of involvement is low. Reference Groene and Sunol10 All the changes we implemented as part of our quality improvement initiative were driven by our patient advisory committee, comprised of patients and family members who had undergone treatment for PA at our center. This is directly in line with the Patient Declaration of Values for Ontario. 9
A study by Armstrong et al. Reference Armstrong, Herbert, Aveling, Dixon-Woods and Martin15 evaluated patient and public involvement in quality improvement for lung-cancer care at three different levels: input from two relevant public charities, a patient representative involved in regional meetings, and a patient advisory group, like in our study. The authors note that all three modes of patient involvement were beneficial and there may not be a single best method for patient involvement. For example, as their study involved lung-cancer care where most patients had a terminal diagnosis, long-term patient involvement was not possible. They contrast this with an initiative in the chronic renal disease where long-term and flexible patient-involvement was successful. They stress that there is no “one-size fits all” model for patient involvement in quality improvement and go on to identify elements for successful patient involvement in any model. These include clarity in the rationale for patient involvement, identifying the right model for patient participation, having clear roles for patients and meaningful contribution, achieved via having patients present at the planning stage, and having clear communication channels.
In our study, we chose a patient advisory group model for patient involvement. This seemed a reasonable approach as our goal was to have patient input in identifying gaps in care delivery at the outset of our intervention. As explained by Armstrong et al., in this case, the patients served as knowledge brokers, bringing the patient experience to the clinicians, highlighting the need for change, and identifying an area with the greatest need for improvement, such as coordination of care and access to educational materials. Reference Armstrong, Herbert, Aveling, Dixon-Woods and Martin15 In presenting our findings, our aim was not to provide a recipe for patient involvement in quality improvement but to highlight the feasibility of such a process and the potential for a positive impact.
In response to demands for greater care efficiency, many countries, and on a smaller-scale, centers, have opted for the division of roles and tasks in healthcare delivery. This has been achieved with decentralization and increased specialization. The unforeseen consequence has been increased fragmentation of care with the risk of patients not receiving holistic care and a lack of coordination of various healthcare provider endeavors. Reference Ahbren16 Literature has repeatedly shown that multidisciplinary care can improve clinical outcomes with reduced hospitalization, decreased mortality, more consistent prescribing practices, and cost-savings to the healthcare system, in both the outpatient and inpatient care setting. Reference Kim, Barnato, Angus, Fleisher and Kahn4,Reference McAlister, Lawson, Teo and Armstrong17–Reference Ajarmeh, Er, Brin, Djurdjev and Dionne21
In the care of PA, the first step in a patient’s journey is their referral being sent and triaged. Our intervention included the establishment of a centralized triaging process that directed all referrals for a pituitary lesion for review and classification based on whether patients would benefit from surgical assessment vs. medical therapy. Potentially surgical cases were directed to the Multidisciplinary Clinic, whereas medical cases (i.e. prolactinomas) were first assessed in the outpatient Endocrinology clinic. This process, combined with increased access to the Multidisciplinary Clinic, possibly led to the observed decreases in wait times, although it has to be noted that the observed decrease could also be due to changes in practice over time. Furthermore, the improvement in wait times was not statistically significant, likely due to the small sample size. However, this trend was consistent across all treatment groups. The greatest decrease in wait time was observed for those patients being directed to medical care.
While healthcare practitioners understand that a longer wait time is usually associated with lesser urgency, and thus severity, of disease, Reference Liddy, Nawar and Moroz22 patients do share this perception. Decreased wait times are consistently associated with higher patient satisfaction. Reference Bleustein, Rothschild, Valen, Valatis, Schweitzer and Jones23 Patients identified that receiving a diagnosis of PA was associated with significant anxiety. The patients were told they had “something growing in their brain” and often the diagnosis was not explained. They had to wait until their consultation to receive answers to their questions and reassurance. Any shortening of wait times is likely to improve outcomes and patient satisfaction as it shortens the duration spent in doubt about the diagnosis and prognosis.
The wait time from diagnosis to the first assessment is subject to the length of time the primary care provider took to send the referral and were out of our control. The wait time from referral to the first assessment was directly impacted by the effectiveness of the triage process and access to the Multidisciplinary Clinic. Prior to intervention, this median wait time for the whole cohort was 23.5 days, and it decreased to 16 days after the intervention. These wait times are comparable, or even shorter than might be expected. A report by Jaakkimainen et al. Reference Jaakkimainen, Glazier, Barnsley, Salkeld, Lu and Tu24 demonstrated that in 2013 in Canada, the median wait time from referral by a primary care provider to consultation with a specialist was 33 days for General Surgery, 43 days for Urology, 60 days for ENT, 39 days for Cardiology and 57 days for Rheumatology, for example. We also surveyed other major Canadian centers that treat PA and received responses from six of them, indicating that their wait times are in general in the order of “weeks to months” (unpublished).
Another change that we observed post-intervention was the location of the first assessment for PA care. There was a shift toward patients being primarily assessed in the Multidisciplinary Clinic. Although we did not quantify the number of visits, this likely represents fewer visits to the hospital as there is no longer a need for separate assessments and cross-referral between Endocrinology and Neurosurgery. This was also observed in the referral pattern with fewer referrals coming from Neurosurgery. This change is the result of the change in triage, but more importantly by the increased availability of the Multidisciplinary Clinic.
In diseases such as PA, where multiple treatment modalities supported by different specialists must work in concert, facilitating access to multiple specialties at once streamlines care. Having Neurosurgeons and Endocrinologists present at the same appointment allows the medical team and patient to create and efficiently implement a personalized treatment plan. This saves the patient time and hospital visits, promotes consistent messaging, faster treatment decisions, decreases in duplicate testing, and most importantly, increased confidence of the patient in their care. Reference Ruhstaller, Roe, Thürlimann and Nicoll25,Reference Naidu26
Patients also desire a reputable and reliable source of information outside of consultation with their healthcare provider to help them understand and cope with their disease. This was clearly identified by the advisory committee as a need for timely access to information and support and addressed through increased access to patient information and educational materials. The feedback that has been received on these educational initiatives developed (patient information evenings, web resources, and information booklets) has been overwhelmingly positive.
While there many positive outcomes, there were also some unanticipated outcomes. Post-intervention, more imaging scans were completed. This is likely a reflection of a higher proportion of patients undergoing surgery in the second cohort, which would require pre-operative imaging for surgical planning, as opposed to an actual change in the practice patterns of our center.
We also observed a longer wait for follow-up imaging in the post-intervention cohort, especially in the medically managed patients. This, however, may reflect challenges with obtaining imaging in our center that was occurring at the time of the study. Also, there was a trend toward increased wait time for the first follow-up after surgery. Our intervention appears to have had a more profound impact on pre-operative assessment and care.
The goal in sharing our experience, thus far, is to demonstrate the success we have had with the Multidisciplinary Clinic approach to PA care, specifically, but more generally to provide a template for other practitioners on how patient involvement could be increased in quality improvement initiatives.
We have reached out to other Canadian centers with PA programs to assess their approach and whether they employ a multidisciplinary model. Our next goals are to streamline and standardize the biochemical work-up for PA and to standardize post-operative glucocorticoids use and we hope to draw on the success of other centers. As previously noted, our center is sufficiently large and we have multiple clinicians in the Endocrinology and Neurosurgery divisions that we foresee being having sufficient staff to maintain our current approach for the foreseeable future. Furthermore, even though the number of clinics was doubled, the number of clinic visits for each patient has been halved, effectively keeping the cost to the hospital neutral. Thus far, our experience has been positive, and we would recommend it to other centers, where possible.
Limitations
This is a single-center retrospective analysis. The small sample size may have limited the statistical significance of our observations. Pre- and post-intervention analysis is a weaker design for quality improvement research and the observed changes (e.g. in wait times) may be due to changes in practice patterns and not attributed to our intervention. The selection of the patient advisory committee depended on purposeful sampling and the patients who participated may not be representative of the full patient population.
Six patients were excluded in the post-intervention analysis as at the time when the data were collected, they had not yet received their surgical treatment and thus data on follow-up were unavailable. Even with their exclusion, the size of the pre- and post-intervention cohorts was similar.
Conclusions
We demonstrated that a patient-inspired quality improvement initiative in PA care with improved access to a Multidisciplinary Clinic led to more streamlined assessments and may have decreased wait times to treatment decisions. We also implemented several education and support projects, which have been positively received by our patient population. In a time where the concept of “patient-centered care” is moving beyond the individual patient–physician interaction, we demonstrated that patients can be involved on a larger scale, impacting not just their own health, but healthcare delivery overall.
Acknowledgements
The authors thank Emily Sharples for support with the patient advisory board and Kathy Styles for assistance with data retrieval.
Disclosures
None of the authors have any conflicts of interest to disclose other than funding for portions of this project was provided by the University of Ottawa, Department of Medicine Patient Quality and Safety Grant.
Statement of Authorship
ID identified eligible patients, collected, and analyzed data, created, and edited tables and figures, wrote, and edited the manuscript. MAD designed intervention, analyzed data, wrote, and edited the manuscript. AA collected data and edited the manuscript. DL collected data and edited the manuscript. FA identified eligible patients, analyzed data, and edited the manuscript. CA identified eligible patients, analyzed data, and edited the manuscript. EK designed intervention, ran patient advisory committee, and edited the manuscript. JM designed intervention, ran patient advisory committee, analyzed data, edited figures, wrote, and edited the manuscript.








