No CrossRef data available.
Article contents
Early hepatic proteomic signatures reveal metabolic changes in high-fat-induced obesity in rats
Published online by Cambridge University Press: 27 October 2023
Abstract
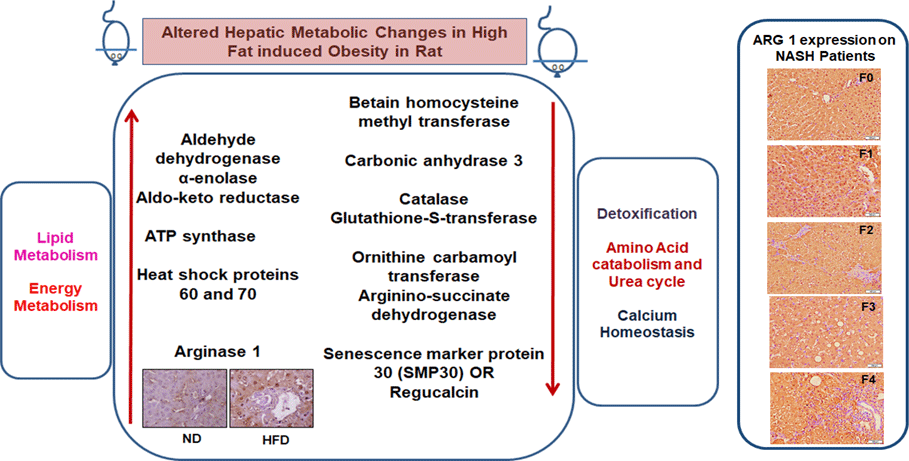
The prevalence of diet-related obesity is increasing dramatically worldwide, making it important to understand the associated metabolic alterations in the liver. It is well known that obesity is a multifactorial condition that is the result of complex integration between many gene expressions and dietary factors. Obesity alone or in conjunction with other chronic diseases such as diabetes and insulin resistance causes many health problems and is considered a major risk factor for developing non-alcoholic steatohepatitis (NASH) and cirrhosis. In this study, we aimed to understand the molecular mechanisms underlying early hepatic changes in the pathophysiology of high-fat diet (HFD)-induced abdominal obesity in rats. Hepatic protein profiles of normal diet and HFD-induced obesity for 24 weeks were analysed using two-dimensional differential gel electrophoresis (DIGE) and protein identification by MS. Fifty-two proteins were identified by matrix-assisted laser desorption ionization-time of flight (MALDI-TOF), and computer-assisted DIGE image software analysis showed that eighteen major proteins were significantly differentially expressed between comparable groups, with 2·0–4·0-fold change/more (P < 0·01). These proteins are regulated in response to a HFD, and differentially expressed proteins are involved in key metabolic pathways such as lipid metabolism, energy metabolism, detoxification, urea cycle and hepatic Ca homoeostasis. In addition, Western blot and immunohistochemistry of liver-specific arginase-1 (Arg-1) showed significant increased expression in the liver of high-fat-fed rats (P < 0·01). Further, Arg-1 expression was correlated with NASH patients with obesity-related fibrosis (F0–F4). It is concluded that high-fat content may affect changes in liver pathways and may be a therapeutic target for obesity-related liver disease. Arg-1 expressions may be a potential pathological marker for assessing the progression of the disease.
Keywords
- Type
- Research Article
- Information
- Copyright
- © Artemis Education and Ressearch Foundation (AERF), 2023. Published by Cambridge University Press on behalf of The Nutrition Society





