Lutein is a unique member of the xanthophyll family of carotenoids. Man does not have the capacity for de novo biosynthesis of carotenoids and an adequate supply of dietary lutein depends on regular intakes of fruits and vegetables(Reference Bone, Landrum and Dixon1). Unlike other carotenoids, lutein and its structural isomer, zeaxanthin, are specifically highly concentrated in the macula(Reference Landrum and Bone2), and are believed to play a major role in protecting retinal constituents from free radicals(Reference Wooten and Hammond3). Over the past few years, there has been increased interest in evaluating the effect of lutein for optimizing eye health. Epidemiological studies support the notion that high dietary intake of lutein is strongly associated with a decreased relative risk of ocular diseases(Reference Bernstein, Zhao and Wintch4, Reference Gale, Hall and Phillips5). Findings from placebo-controlled intervention trials show that dietary supplementation with lutein may help to improve visual function in patients suffering from age-related macular degeneration and other ocular diseases(Reference Schalch, Cohn and Barker6, Reference Dagnelie, Zorge and McDonald7). Furthermore, numerous structures of the eye do not undergo processes of biological renewal and thus, once lost, cannot be restored(Reference Sujak, Gabrielska and Grudziński8). Damage to these structures accumulates with age and eventually results in permanent visual loss. For the aforementioned reasons, dietary intervention in healthy populations is often seen as an important means of maintaining the health of the macula and preventing age-related eye disease. In particular, long-term computer display light exposure may lead to visual function damage, and duration of daily computer display light exposure is linearly related to the physical symptoms, including visual disorders(Reference Nakazawa, Okubo and Suwazono9). However, little is known about the potential benefits of lutein on visual function in healthy populations, especially in persons with long-term computer display light exposure. Therefore, the objective of the present study was to examine the effect of consuming different doses of lutein on visual function in healthy persons with long-term computer display light exposure.
Subjects and methods
Subjects
Thirty-seven healthy subjects were recruited, aged 22–30 years. The average daily computer usage time was longer than 10 h during the previous 2 years. The subjects' levels of education, income and marital status were recorded at the time of recruitment. A detailed optometric examination was conducted and no clinically detectable signs of ocular disease or other abnormalities were found. Participants with a history of smoking, alcohol consumption, BMI ≥ 30 kg/m2, allergies, ocular diseases and participants taking vitamins or other food supplements containing lutein were excluded from the study. The medical ethics committee of Peking University approved the protocol. All participants provided signed consent forms after the nature of the study was provided to them.
Study design
The study was a randomized, double-blind, placebo-controlled, 12-week intervention study. At recruitment, each subject was randomly assigned to one of three equal groups on the basis of sex: Group L6, who received 6 mg lutein/d (n 12); Group L12, who received 12 mg lutein/d (n 13); and a control group (Group Placebo), who received a maltodextrin placebo (n 12). All capsules of the lutein supplement were provided by Beijing Yuguang Bioscience Research Center Co. Ltd (Beijing, China). The Food and Drug Administration of China certified that the capsules contained 6 or 12 mg lutein. To ensure compliance, the capsules were dispensed to participants per day by professional staff and they were asked to take the capsules on the spot. In addition, we kept a record on a card after the capsules had been taken. They were requested to avoid excessive intakes of food items rich in lutein without any other modification of habitual diet assessed using FFQ and 3 d weighed food record at baseline and final study visit(10).
Levels of serum lutein and visual performance indices were measured at the onset and the end of the intervention.
Serum lutein concentrations
Fasting blood samples (5·0 ml) were obtained to determine serum lutein. Blood specimens were processed at the central laboratory of the School of Public Health, Peking University (Beijing, China). After clotting for 60 min, serum was separated from blood by centrifugation at 3000 g at 4°C for 10 min (Sorvall centrifuge; Sorvall Instruments, Newtown, CT, USA), then aliquoted into three amber-coloured tubes and stored at − 70°C until the time of measurement (within 5 months). All procedures were performed in subdued light.
Serum lutein concentrations were quantified with the Agilent 1100 HPLC system(Reference Khachik, de Moura and Chew11). A C18 column (150 mm × 4·6 mm internal diameter, 5 μm; Supelco, Bellefonte, PA, USA) with a C18 pre-column was used to separate the analytes and the detection was set at 450 nm. Quantification was accomplished by comparing the peak area of the analyte with the peak area of a known amount of standard in a calibrator solution. Calculations were corrected based on the peak area of the internal standard (Sigma-Aldrich, St Louis, MO, USA).
Visual function examination
Uncorrected visual acuity (UCVA) and best-spectacle corrected visual acuity (BSCVA) were measured with decimal charts in an examination room with standardized lighting conditions.
Contrast sensitivity as well as glare sensitivity was measured using the contrast glare tester (CGT-1000; Takagi Seiko, Nagano, Japan). The CGT-1000 is able to determine accurately contrast sensitivity and glare sensitivity in a rapid and simple automated manner. It measures thirteen-step contrast thresholds using concentric ring-shaped visual targets that are equivalent to visual angles of 6·3, 4·0, 2·5, 1·6, 1·0, and 0·7° at 0·35 m with a constant background luminance of 10 cd/m2. Glare sensitivity is measured by adding glare sources of 50 cd/m2 around the visual targets, which automatically switch on to evaluate contrast sensitivity with simultaneous glare around.
Statistical analyses
Decimal visual acuity (VA) was converted to a logarithm of minimal angle of resolution, while contrast sensitivity and glare sensitivity were converted to the logarithm of inverse values. Differences of baseline characteristics among groups were tested with χ2 test or ANOVA. The changes during the supplementation were assessed using paired t tests and ANOVA. Univariate associations between baseline VA and VA change from baseline were evaluated using the Pearson correlation. All the calculations were conducted with SPSS 10.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics
The baseline characteristics of participants are summarized in Table 1. No statistical differences were observed among the groups for age, sex, BMI, dietary nutrient intake and serum lutein concentration. The three groups also did not differ in visual performance indices, except for higher contrast sensitivity at 4·0° in Group Placebo (P = 0·045).
Table 1 Baseline characteristics of the subjects*
(Mean values and standard deviations)
* Group L6 received 6 mg lutein/d; Group L12 received 12 mg lutein/d; the control group (Group Placebo) received a maltodextrin placebo.
† There were no significant differences among the three groups, P>0·05 (ANOVA or χ2 test).
Nutritional status
Nutrient intakes were assessed at baseline and week 12. There was no evidence of time-dependent changes or intra-group differences in dietary consumption of these nutrients among groups during the follow-up, except for dietary zinc in Group Placebo, decreasing from 10·5 to 8·7 mg over time (P = 0·041).
Serum lutein concentrations
After a 12-week intervention, serum lutein significantly increased in both intervention groups. There was a larger magnitude of increase in serum lutein in the group that took the larger dose. Increases in serum lutein concentrations at week 12 were approximately 1·71- and 2·23-fold for the 6 and 12 mg doses, respectively, whereas no change was observed in the placebo group (Table 2).
Table 2 Changes in serum lutein concentration and visual function during the supplementation‡
(Mean values and standard deviations)
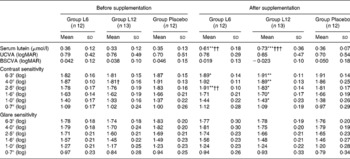
BSCVA, best-spectacle corrected visual acuity; logMAR, logarithm of minimal angle of resolution; UCVA, uncorrected visual acuity.
Mean values were significantly different from those before supplementation (paired t test): *P < 0·05, **P < 0·01, ***P < 0·001.
Mean values were significantly different from those of the control group (Group Placebo) (ANOVA): †P < 0·05, ††P < 0·01, †††P < 0·001.
‡ For details of subjects and procedures, see the Subjects and methods section. Group L6 received 6 mg lutein/d; Group L12 received 12 mg lutein/d; the control group (Group Placebo) received a maltodextrin placebo.
Visual acuity
Except for a slight decrease of UCVA logarithm of minimal angle of resolution in Group L12, no significant changes of UCVA were found during lutein supplementation. The change of BSCVA was basically consistent with UCVA. However, the values of BSCVA had a greater decrease both in Group L6 and Group L12, whereas there were also no significant changes in the three groups.
Pearson correlation was performed in the three groups respectively to determine if there might be statistical associations between VA at baseline and the change of VA from baseline. There were significant negative correlations between baseline UCVA and UCVA change from baseline (r 0·724, P = 0·042) and between baseline BSCVA and BSCVA change from baseline (r 0·798, P = 0·016) in Group L12, whereas no significant correlations were observed in Group L6 and Group Placebo.
Contrast sensitivity and glare sensitivity
Inter-group comparison of changes in contrast sensitivity thresholds at multiple visual target sizes over time revealed a trend towards higher thresholds in Group L6, and especially with a greater effect in Group L12. Statistically significant changes were found at visual angles 6·3 and 2·5° in Group L6 and at visual angles higher than 0·7° in Group L12, while the change of the Group Placebo was non-significant. The ANOVA analyses for contrast sensitivity among groups showed a significant difference at 2·5° (F 6·39, P = 0·003).
Compared with baseline measurements, none of glare sensitivity thresholds showed a considerable change over time. Though not statistically significant, there was a slight trend in glare sensitivity improvement in Group L12.
Discussion
High expectations have accompanied the increasing indirect evidence that there may be a beneficial effect of lutein on retinal degenerative disease, especially age-related macular degeneration and cataracts. At present, there is very little published data about visual function and lutein supplementation in healthy populations, especially in persons with long-term computer display light exposure. As mentioned earlier, we are unaware of any previous randomized placebo-controlled trial of lutein in Chinese subjects. In the present study, we evaluated how serum lutein concentration in human subjects responded to supplementation with lutein. During the 12-week period of supplementation, levels of serum lutein in both intervention groups rose markedly with increasing doses of lutein, regardless of the baseline lutein status. The present result was consistent with data from another recent report about lutein supplementation(Reference Rosenthal, Kim and de Monasterio12).
Previous studies had suggested a beneficial effect of lutein on VA. The study conducted by Richer(Reference Richer13) demonstrated that supplementation with diets containing five ounces of spinach (equivalent to approximately 14 mg lutein) and purified lutein four to seven times per week could improve VA of fourteen age-related macular degeneration patients. Olmedilla et al. (Reference Olmedilla, Granado and Blanco14) supplemented five cataract patients with lutein capsules (7 mg/d) for up to 2 years, and found that VA of lutein-supplemented patients improved nearly one line on the Snellen visual acuity chart compared with the placebo group. In the present study, we found that there was slight improvement of UCVA and BSCVA as a result of the supplementation, especially in Group L12, although this was not statistically significant. It indicated that there was weak evidence in favour of a positive effect of lutein supplementation in improving VA. The non-significant results might be due to delayed effect of lutein on VA in a short time period. Another possible reason was the different VA levels among the subjects in the present study and their study. The subjects in studies conducted by Richer and Olmedilla were patients with retinal degenerative disease, while our subjects were selected from a young healthy population with good vision. Furthermore, if the baseline VA inversely affected the effect of lutein supplementation, then changes in the subjects with good vision might have been limited more than changes in the patients with diseases. In fact, highly significant negative associations were observed between baseline VA and the change in VA among subjects in Group L12, which implied that the subjects with low vision might benefit more from future lutein interventions.
Some people have normal VA, but they have poor quality of vision in both photopic and mesopic conditions, especially if they suffer from long-term computer display light exposure(Reference Orr, Barron and Schein15). Thus, VA as the sole measure of visual outcome is inadequate and visual outcome should be measured in terms of contrast vision(Reference Mangione, Gutierrez and Lowe16). Over the past few years, several methods had been developed to assess a subject's quality of vision, most of which were based on determining contrast sensitivity(Reference Nousiainen, Kalviainen and Mantyjarvi17). In the present study, we found the contrast sensitivity increased with supplementation in intervention groups, and a statistically significant rise was observed at most visual angles in Group L12 after supplementation. The present study demonstrated that supplementation with lutein could improve contrast sensitivity thresholds. The findings from the present study confirmed other earlier reports suggesting increased levels of contrast sensitivity as a result of supplementation with lutein(Reference Olmedilla, Granado and Blanco14, Reference Richer, Stiles and Statkute18). In contrast, it should be underlined that there were statistically significant improvements in contrast sensitivity in healthy eyes, rather than age-related macular degeneration and cataract patients(Reference Richer, Stiles and Statkute18, Reference Olmedilla, Granado and Blanco19). The importance of the present finding, if replicated in larger studies, rested on the fact that any putative beneficial effect of visual performance would not be restricted to subjects without evidence of established disease. Although the mechanism for the improvement in contrast sensitivity by lutein supplementation remained unknown, a plausible explanation was that supplementing lutein induced a substantial increment in macular pigment which could improve visual performance via reduction of longitudinal and lateral chromatic aberration in the eye and its action as a modulator in signal-transduction pathways.
Additionally, in contrast with the findings of some previous studies(Reference Olmedilla, Granado and Blanco14, Reference Mares-Perlman, Fisher and Klein20), there was no statistically significant change of glare sensitivity over time. The results of the present trial revealed that lutein supplementation was not effective in improving glare sensitivity. Although previous studies claimed some success with selected patients, the present study found that lutein supplementation resulted in non-significant improvement of glare sensitivity in healthy subjects. This was probably because the subjects in previous studies were hospital patients with ocular diseases. Their threshold for photophobia responses was much lower for lights of short wavelengths(Reference Stringham, Fuld and Wenzel21). However, the subjects with long-term computer display light exposure were likely to tolerate higher levels of light energy before the photophobia threshold was reached(Reference Hedge, Sims and Becker22). Therefore, our estimates of the efficacy of lutein supplementation to glare sensitivity might be an underestimate in comparison with other earlier reports.
The strengths of the present study included the high rates of compliance and follow up, and the prospective and randomized design. Furthermore, there were no dietary restrictions or changes and dietary nutrient intakes of each group remained almost unchanged during the supplementation.
In summary, the results of the present pilot study showed that lutein supplementation for 12 weeks was effective for reaching serum lutein concentrations comparable to those that led to improvement in visual performance, especially in contrast sensitivity. It also provided important evidence for the further investigation of the role of lutein supply with respect to visual function.
Acknowledgements
The present study was conducted at the Department of Nutrition and Food Hygiene, School of Public Health, Peking University, with funding from the Chinese Nutrition Society. There are no conflicts of interest. Each author contributed to the manuscript. X.-M. L. was the chief of the study and the leader of the experimenters, L. M. was a chief experimenter of the study and responsible for preparation of the manuscript, Z.-Y. Z., X.-R. X, Y. L. and R. X. were experimenters and did the statistical analysis.






