Background
According to World Health Organization (WHO) classification, the Eastern Mediterranean Region (EMR) comprises 22 countries with a total population of nearly 679 million.1 These countries are: Afghanistan, Bahrain, Djibouti, Egypt, Iran (Islamic Republic of), Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syrian Arab Republic, Tunisia, United Arab Emirates and Yemen.
The prevailing situation of war, insurgencies, political conflict and civil unrest in many countries of the region has dramatically influenced substance use problems in every aspect, from production and trafficking to availability and pattern of use. This is compounded by the long-standing position of this region as one of the largest opium production sites globally.2 These instabilities prevent health and social care systems from providing and sustaining harmonised and integrated effective services. Additionally, increased production and availability of different types of stimulant, especially captagon, has also become a major drug problem in the regionReference Al-Imam, Santacroce, Roman-Urrestarazu, Chilcott, Bersani and Martinotti3 (Fig. 1). From the information available the general situation of substance use in the EMR region indicates that in 2017 about 4.2 million disability-adjusted life-years (DALYs) were lost due to substance use disorders7 (Fig. 2). The regional estimated crude death rate due to substance use disorders in 2015 was reported as 1.5 per 100 000 population, which has not changed since 2000.10 Although this is lower than the global estimate in 2015 (2.3/100 000), the figures should be carefully considered owing to possible weaknesses in the collection of the epidemiological data.
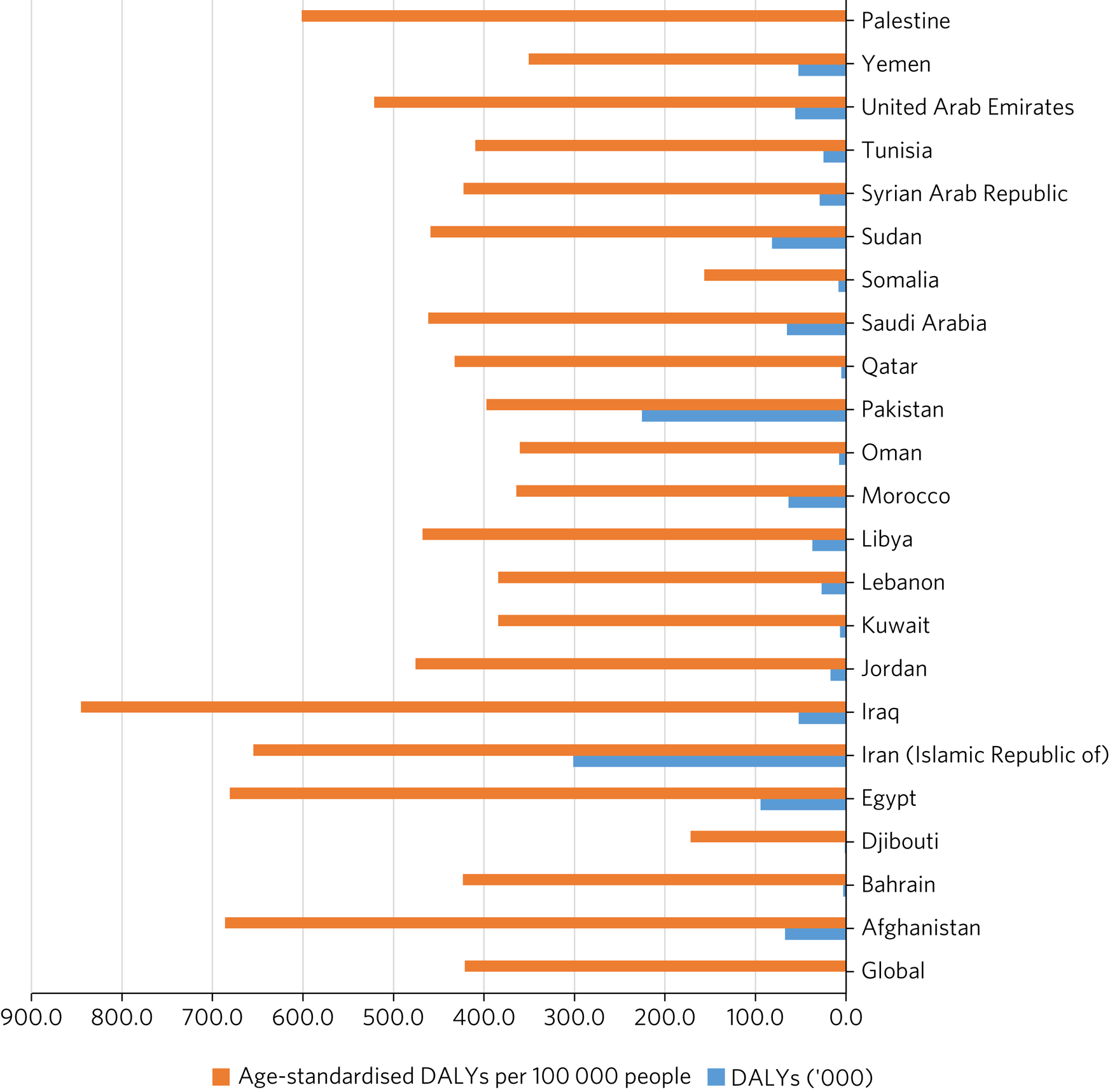
Fig. 2 Age-standardised disability-adjusted life-years (DALYs) per 100 000 people (2016) and total DALYs (’000) (2015) in the Eastern Mediterranean region compared with the global estimate.Reference Degenhardt, Charlson, Ferrari, Santomauro, Erskine and Mantilla-Herrara8,9 Some data were not available.
Pattern of substance use in the region
The EMR has been the scene of prominent production and seizure of opioids, cocaine, amphetamine-type stimulants and khat.
Opioids
Opioids remain the main cause of mortality related to use of illicit substances in the region. The second- and third-highest global death rates per 100 000 from opioid overdoses occur in Libya and the United Arab Emirates (UAE) respectively.Reference Ritchie and Roser11 Also, opium smoking is a traditional practice in countries such as Afghanistan, Iran and Iraq.
Tramadol is an opioid that is widely used to treat moderate to severe pain and has also been used off-label in the treatment of sexual dysfunction such as premature ejaculation. There is growing evidence of non-medical use of tramadol in the EMR, reflected in the number of people in treatment for tramadol-related problems and the number of tramadol overdose deaths reported in some countries, particularly among young people.12 Different studies have concluded that the high levels of misuse of tramadol are a result of its easy availability in pharmacies (including without medication refills in some of these countries) and illicit markets, low price compared with illicit drugs, perceptions among users that tramadol is safe as it is a prescription medication, and the ease with which it can be hidden. Having in mind that less than 10% of tramadol users have a medical source,Reference Abd-Elkader, Kabbash, El-Sallamy, El-Sawy and Gad13 the non-medical use of tramadol has been reported by many countries, including Egypt, Iran, Jordan, Lebanon, Libya, Qatar, Saudi Arabia and the UAE. Among Egyptian adolescents, tramadol use is more prevalent than heroin.Reference Rabie, Shaker, Gaber, El-Habiby, Ismail and El-Gaafary14 Tramadol use in the Iranian general population has been estimated at 4.9% among males and 0.8% among females.Reference Rostam-Abadi, Gholami, Amin-Esmaeili, Safarcherati, Mojtabai and Ghadirzadeh15 Increasingly, tramadol has been placed under national control in most EMR countries and is therefore only legally accessible by prescription. Such tight control is concerning because it may restrict the medical use of tramadol, particularly in countries of the region where regulatory mechanisms make other opioids (opioid agonist treatments for opiate addiction) less available for medical use.
Amphetamine-type stimulants, including captagon
The increasing trend of clandestine manufacture and use of amphetamine-type stimulants has become a major concern in countries such as Iran, Morocco and Pakistan. There is also a high demand for fenethylline (captagon) tablets in some countries of the region, especially in Syria, Lebanon and countries in the Arabian Peninsula.16 Captagon® was first introduced for its beneficial effects on hyperactivity, depression and narcolepsy, but its addictive and hallucinogenic features made it a popular illegal psychoactive substance.Reference Wu, Feng, He, Kwon, Wang and Xie17 Captagon® itself is no longer manufactured and counterfeit captagon tablets are mostly combined with amphetamine, caffeine, ephedrine, quinine, theophylline acetaminophen and diphenhydramine and may cause unpredictable complications.Reference Al-Imam, Santacroce, Roman-Urrestarazu, Chilcott, Bersani and Martinotti3 In Saudi Arabia, there are more treatment admissions registered as a result of captagon use than opioid use.Reference Shadloo, Amin-Esmaeili, Haft-Baradaran, Noroozi, Ghorban-Jahromi and Rahimi-Movaghar18
In addition to the established patterns, there have been emerging regional trends of substance use not only related to cultural and geographical expectations in the region but also as a result of the large number of displaced populations. Captagon is an illustration of this trend.Reference Crabtree19 A novel concern about captagon use in Syria and neighbouring countries is that soldiers from all parties to the conflict use the drugs as combat stimulants (‘chemical courage’).Reference Wu, Feng, He, Kwon, Wang and Xie17 Meantime the current unstable situation in Syria has forced some traffickers to move production of captagon to Libya, Jordan, the UAE, Saudi Arabia and Sudan.Reference Crabtree19
Khat
Catha edulis, commonly known as khat, is a flowering plant growing in the khat belt countries in the Horn of Africa and the Arabian Peninsula. Khat misuse and dependency is still the major illicit substance use-related problem in countries such as Djibouti, Yemen, Somalia and southern provinces of Saudi Arabia.Reference Numan20 Most of the effect of chewing khat is thought to come from two chemicals that are structurally related to amphetamine. In Saudi Arabia, khat use is mostly prevalent in the Jazan region in the south of the country on the Yemeni border. A community-based study conducted in the Jazan region reported an overall prevalence of 29% of current khat chewing among respondents. Khat chewing was about four times higher among males than females in both current and lifetime users.Reference Mahfouz, Rahim, Solan, Makeen and Alsanosy21 It is reported that nearly 67.9% of adults in Yemen have at least one lifetime episode of khat use.Reference Numan20
People who use khat frequently report increased levels of energy, alertness and self-esteem, better ability for communication, sensations of elation, enhanced imaginative ability and a greater capacity for associating ideas. The literature suggests that khat use is associated with personal/public health and social problems. Khat chewing might reduce productivity considering the large amount of time individuals spend on khat chewing. Additionally, another group of studies suggested a possible association between heavy khat consumption and psychosis.Reference Manghi, Broers, Khan, Benguettat, Khazaal and Zullino22
Multiple substance use
Multiple substance use is a common practice in the EMR and adulterated substances available on the drug market have added to the vulnerability of people with substance use to various health hazards, making the clinical picture of drug intoxication complicated. For example, in some countries of the EMR people have added amphetamine-type stimulant use to opium use – drugs with completely different profiles of intoxication and withdrawal symptoms.Reference Alblooshi, Hulse, El Kashef, Al Hashmi, Shawky and Al Ghaferi23 Amphetamine-type stimulant use by patients under methadone maintenance treatment, especially women, is also a potential threat to treatment success.Reference Radfar, Cousins, Shariatirad, Noroozi and Rawson24 Lead poisoning among people who use opium has been a problem predominantly observed in Iran due to the impurity of opium products.Reference Alinejad, Aaseth, Abdollahi, Hassanian-Moghaddam and Mehrpour25 The impurity of drugs might be due to the addition of heavy metals by local retailers, to produce heavier packages and therefore higher prices.Reference Ghane, Zamani, Hassanian-Moghaddam, Beyrami and Noroozi26 The other routine scenario is adding hallucinogens or sedatives or even other pharmacological formulas to improve the experience of the person who uses the drug.Reference Akhgari, Etemadi-Aleagha, Jokar and Preedy27 Therefore, many people who have used a single street substance may present with a mixed clinical picture.
Conclusions
The EMR has a unique nature due to the presence of conflict and emergency in a number of countries. One may hypothesise that a combination of (a) social instability with additional increase in forcibly displaced populations, (b) increased demand in these substances for personal consumption by the affected heterogenous populations in the region and involved combatants, as well as (c) the enhanced production and distribution of these emerging drug markets has synergistically created the 'perfect storm' across the Eastern Mediterranean countries. This heterogeneity is reflected in the hybrid pattern of substance use and the emergence of new trends. The presence of a significant number of populations on the move due to internal displacement or migration affects the capacity of national health systems to effectively manage the evergrowing substance use problem and to meet the needs of the population. Accurate epidemiological data are needed to allow a better understanding of the impact of this problem on both general and marginalised populations.
Key points of this article are summarised in Box 1.
Box 1 Key points
• Within the EMR there is increasing use of opioids (tramadol) and stimulants (captagon and khat) outside the usual cultural and/or medical boundaries for these potentially psychoactive substances.
• Regional political instabilities have fuelled the use, production and trafficking of these substances, potentially creating problems within healthcare systems.
• Being known as the traditional production and trafficking hub for various drugs demands the importance and need for more attention to control the substance use situation in the EMR. This can only be achieved with reliable and accurate data collection.
• The exclusive video abstract (available at: https://vimeo.com/bjpsych/bji-2021-53) also summarizes the key points of this paper.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bji.2021.53.
Data availability
Data availability is not applicable to this article as no new data were created or analysed in this study.
Acknowledgements
We thank Mahdi Amiri (Student Research Committee, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran) for his efforts in designing the video abstract (https://vimeo.com/bjpsych/bji-2021-53) and Faezeh Shahalami (Department of English Literature, Allameh Tabataba'i University, Tehran, Iran) for her contribution in recording narrations for the video abstract.
Author contributions
All the authors contributed to the conception of the paper. A.A., H.M.A. and A.M.B. reviewed the literature and drafted the first versions of the textual content and figures; all ten authors then revised it and added their comments. H.M.A. and A.A. finalised the manuscript, which was finally approved by the other authors.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.