1.1 Introduction and Background
This document provides a new edition and an update to the 2015 NEPTUNE guidance on the clinical management of harms resulting from acute intoxication and from the harmful and dependent use of ‘club drugs’ and ‘novel psychoactive substances’ (NPS).
The guidance is evidence-based and is a response to the gap in knowledge and experience in the management of these drugs. There is evidence that clinicians often feel poorly equipped to assess and manage the harms of NPS and report that more education on emerging drugs and misuse patterns is needed.Reference Lank, Pines and Mycyk1 It has also been noted that continued education on NPS is fundamental for the provision of improved harm reduction services, which can enhance overall care for NPS service users.Reference Ramos C, Guirguis A and Smeeton N2
Patterns of drug use continue to be dynamic. At the time of publication of this second edition, the quantity and range of drugs available to people is wider than ever. Recreational users typically use a wide repertoire of substances:
‘Traditional’ drugs continue to be the most used (depending on country, but e.g. cannabis, cocaine, amphetamines).
Novel psychoactive substances (NPS) are used along with these traditional drugs, but have not replaced them.
Increase of non-medical use of prescription drugs.
This document focuses on the health-related harms of club drugs and NPS and their clinical management.
The use of substances referred to as ‘club drugs’ has been well established for many decades. It includes illicit substances, e.g. cocaine and amphetamine, as well as NPS.
The use of NPS is a relatively more recent global phenomenon, with 120 countries and territories from all regions of the world having reported one or more NPS to the United Nations Office on Drugs and Crime (UNODC) Early Warning Advisory on New Psychoactive Substances.3
Novel psychoactive substances have been found in most of Europe and North America, as well as Oceania, Asia and South America, and in a number of African countries. To some extent, however, NPS are primarily a North American and European phenomenon. Although NPS affects all regions of the world, there are diverse regional patterns, in terms of both the type and number of NPS reported by individual countries. The NPS situation also differs by country from one year to the next.4
1.2 NEPTUNE Aims and Guidance Development
1.2.1 Objectives of NEPTUNE
This document is the 2022 update of the 2015 guidance on the harms and management of NPS and club drugs, developed by NEPTUNE (Novel Psychoactive Treatment UK Network). This edition has been funded and supported by EU-Action Against Drugs and Organised Crime (EU-Act).5
The aim of the guidance is to improve confidence, competence, and skills of clinicians in the detection, assessment, and management of the harms associated with the use of NPS.
Specific areas addressed include:
Detection/identification. Recognising the significant psychological, physical, and social risks which can be associated with club drugs and NPS, and equipping professionals to be able to recognise problematic use, associated harms, and dependence.
Assessment. Assessment of the problems related to the use of club drugs and NPS, including the assessment of both direct and indirect harms.
Management. Clinical management of acute and chronic harms related to the use of club drugs and NPS – based on the best available evidence.
Harmr eduction. Interventions aimed at preventing morbidity and mortality among individuals presenting to clinical settings, including measures to reduce the harms of club drugs and NPS for individuals and communities and to help patients achieve and sustain recovery and well-being.
This document provides guidance, not guidelines. The implementation of NEPTUNE at national levels must take place within the principles of national and international guidelines, national and local protocols, as well as the international standards and broad principles for the treatment of substance misuse disorders.6, 7
The implementation of NEPTUNE learning into clinical practice must adapt the learning to take into account factors specific to the region, country or sector where they are implemented. This includes the needs, priorities, legislation, policies, systems of healthcare delivery and resources of the various countries. Adaptation should be carried out without undermining the validity of the evidence-based training. Local and national protocols, including prescribing protocols, should be used.
For up-to-date information, it is also recommended that clinicians contact the Poisons Centres in their region, where available. These are specialised units that advise on, and assist with, the prevention, diagnosis, and management of poisoning. Their structure and function varies around the world; however, at a minimum, a poisons centre is an information service. Some centres may also include a toxicology laboratory and/or a clinical treatment unit.8
1.2.2 Why Produce Guidance on Club Drugs and Novel Psychoactive Substances?
The underlying principles of good clinical practice in relation to the users of club drugs and NPS are the same as for harmful and dependent drug misuse in general.
Clinicians’ existing experience of the treatment of other commonly used drugs (such as heroin, alcohol or cannabis for example) is very relevant to the treatment of club drugs and NPS.
However, good assessment and management of the harms of club drugs and NPS must also consider the particular challenges posed by novel drugs and address them directly. These include challenges posed by:
New drugs (rapidly changing profile and ever-increasing numbers of substances, with poorly understood harms);
New populations in treatment (including new patterns of drug use and contexts of harm);
New harms (some club drugs are associated with harms not previously linked to illicit drug use, e.g. ketamine-related ulcerative cystitis);
New manifestation of drug-related harms which are familiar to clinicians (e.g. dependence and withdrawal associated with gamma-hydroxybutyrate (GHB).
NEPTUNE therefore aims to improve clinicians’ knowledge of the specific issues relating to NPS and to support evidence-based practice at local levels. It also aims to help improve clinicians’ confidence in working with patients who use NPS, by providing the following:
1.3 Target Audience for the Guidance
1.3.1 Primary Audience
This guidance is aimed primarily at a clinical audience and most specifically clinicians who manage physical and mental health problems associated with harmful or/and dependent drug use and ensuing acute or chronic problems.
These will include clinicians working in specialist drug treatment and recovery services, as well as in emergency departments. The document is also relevant to professionals working with populations at risk of drug-related harms and associated poorer treatment outcomes, such as mental health services, prison health services, primary care, sexual health services, HIV treatment, hepatology and others.
1.3.2 Other Audiences
Although not directly aimed at them, this document is also a resource for funders/commissioners and policy-makers in developing local, national or regional services. It also provides patients and carers with information on what interventions should be available.
1.4 The Process of Developing the Guidance
1.4.1 Method for the Literature Review
This document is based on a comprehensive review of the English language literature on the harms and the clinical management of a range of club drugs and NPS, using systematic methods. A multi-disciplinary group of people were involved in developing the NEPTUNE framework and the guidance document was independently peer reviewed.
The first edition of this guidance was published in March 2015.This edition also includes a review of the research literature published until 2021.
For the review of the evidence, studies were identified using electronic searches of Medline, Medline Plus, the Cochrane Library, CINAHL, Current Content, Embase, PUBMED, PsychINFO, Google Scholar and the Science Citation Index. In addition, bibliographies of articles were screened for additional relevant studies.
The outputs of searches were considered against sets of inclusion and exclusion criteria. The citations produced by these searches were then screened via their abstract. Those considered relevant were identified and subjected to critical assessment.
The critical assessment of the evidence was based on the framework developed by the British Association for Psychopharmacology for the development of guidelines for the management of substance misuse.Reference Lingford-Hughes, Welch, Peters and Nutt9 This classifies the strength of evidence as follows:
Strong research evidence (e.g. Cochrane reviews, meta-analyses, high-quality randomised controlled trials);
Research evidence (e.g. controlled studies or semi-experimental studies);
Emerging research evidence (e.g. descriptive or comparative studies, correlation studies, evaluations or surveys and non-analytic studies, e.g. case reports, case series);
Expert panel evidence/consensus;
Expert by experience evidence (service users/patients);
Lack of evidence (no evidence, for or against);
Conflicting evidence.
The 2021 update of the 2015 NEPTUNE guidance document continues to suggest that the evidence base on NPS remains relatively small, albeit exp-anding.Reference Santos-Toscano R, Guirguis A and Davidson D.10
In particular, studies on the toxicity and management of the harms of NPS and risks associated with long-term use and dependence liability are few, partly because most NPS have limited or no medical use, and partly because some of these substances have only recently emerged.
Overall, a review of the evidence shows that there continues to be limited robust evidence, in particular from meta-analyses or high-quality randomised controlled trials, and even controlled and semi-experimental studies are few. The bulk of the research available provides what is referred to as emerging research evidence, as it is based principally on non-experimental descriptive studies, consisting mainly of case reports and series and a small number of prospective observational studies, retrospective cohort studies and analysis of patient records.
This document therefore does not give definitive answers on the clinical management of NPS, but broad guidance based on the current best available evidence.
1.4.2 Substances and Drug Groups Covered by This Guidance
1.4.2.1 Classifying Novel Psychoactive Substances
Just over psychoactive drugs (NPS) have been reported for the first time in the last decade or so. Because of the very large number of NPS that have been detected and those that will emerge in the future, it is not possible to cover them all in any detail within the confines of this work. Nor is it realistic for clinicians to remember information on all NPS.
In order to deal with these large numbers of NPS and to future-proof this guidance, a two-pronged approach has been adopted.
Categorising Groups of Novel Psychoactive Substances
In order to understand the harms of NPS and how to manage them, it is useful to be able to classify them into different categories. Classification of NPS could be achieved using a variety of approaches, including chemical structure or pharmacological effect.
However, a useful method of categorising NPS is according to their primary psychoactive, physical and psychiatric effects and to use categories that clinicians working with the effects of substance misuse are already familiar with (see Figure 1.1).
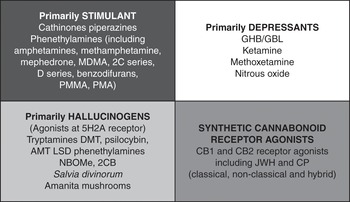
Figure 1.1 Categorising substances by their primary psychoactive effects
A drug’s primary effects will provide a conceptual framework for NPS, which will help clinicians navigate the hundreds of new substances detected in recent years, while allowing them to draw on their existing experience of substance misuse.
This classifies NPS and club drugs into the following groups:
Primarily stimulants
Primarily depressants
Primarily hallucinogens
Synthetic Cannabinoid Receptor Agonists (SCRAs) are put in a category of their own and are classified as a fourth separate category, as they do not fit easily into the other groups. This is because they are such a chemically and pharmacologically diverse group that their specific harms and clinical management also varies widely.
Although these classifications provide a useful framework for this guidance, it is important to note that they are not rigid categories. In reality, many drugs have a combination of effects, often dose-related, e.g. a primarily depressant drug can have stimulant effects at low doses. In addition, people will sometimes use NPS as part of a wider repertoire of illegal drugs and alcohol. The co-ingestion of more than one drug is common.
Most NPS are designed to provide legal alternatives to controlled substances, and have harms similar to those associated with the controlled drugs they have been manufactured to mimic.
The proximal mechanisms of most of these effects (as far as they are known) are shown in Table 1.1.
Table 1.1 Proximal mechanisms of drug effects
| Drug | Primary (proximal) target | Brain effect |
|---|---|---|
| Alcohol | Agonist at GABA and antagonist at glutamate receptors | Increases GABA; blocks NMDA glutamate receptors |
| Benzodiazepines | Agonists at benzodiazepine site on GABA-A receptor | Increase GABA |
| GHB | GHB and GABA-B receptor agonist | Mimics GABA; inhibits dopamine release |
| Ketamine | NMDA glutamate receptor antagonist | Blocks glutamate |
| Khat (natural cathinone) | Releases ephedrine, a dopamine releaser | Mild increase in noradrenaline and dopamine |
| Mephedrone (synthetic cathinone) | Releases dopamine and blocks reuptake | |
| Natural cannabis | Cannabis CB1 receptor agonist | Stimulates endo-cannabinoid signalling, leading to a change in cortical and memory function |
| Cocaine | Blocks dopamine reuptake site | Greatly increases dopamine |
| Amphetamines (dexamphetamine and methyl) | Release dopamine and block reuptake | Greatly increase dopamine and noradrenaline |
| MDMA | Blocks serotonin and dopamine reuptake | Increases serotonin and dopamine functioning |
| Hallucinogens | Agonists at serotonin 5-HT2A receptors | Change across-cortex signalling |
| Opioids | Agonists at endorphin receptors | Produce euphoria, reduce pain |
Agonist = drug that activates or stimulates a receptor; Antagonist = drug that blocks a receptor.
1.4.2.2 Focus on Particular Substances
The second prong of our approach is to focus in more detail on some commonly used NPS drugs (as well as their derivatives and related compounds) and those that potentially cause most harm.
Where a particular NPS is not discussed in this document, clinicians can refer to the broad groups to which it belongs and can extrapolate information on the management of its acute and chronic harms, while taking into account potential differences in potency, toxicity, half-life and length of effect.
1.5 Background: What Are Club Drugs and Novel Psychoactive Substances?
1.5.1 What Is a Club Drug?
‘Club drugs’ is a short-hand term used for convenience to refer to a group of psychoactive substances typically used in dance venues, house parties, music festivals and sometimes in a sexual context. The term therefore describes a diverse group of substances with different actions.
1.5.2 What Is a Novel Psychoactive Substance?
The term ‘novel psychoactive substance’ (NPS) has been used to describe a diverse group of substances that rapidly emerged from the early to mid-2000s.Reference Peacock A, Bruno R and Gisev N11
The UNODC defines NPS as ‘substances of abuse, either in a pure form or a preparation, that are not controlled by the 1961 Single Convention on Narcotic Drugs or the 1971 Convention on Psychotropic Substances, but which may pose a public health threat’.
Most NPS are thought to be manufactured to mimic the effects of controlled drugs. NPS were developed initially as ‘legal’ replacements to established controlled drugs such as cannabis, heroin, cocaine and MDMA. They are sold openly, in some countries at least, as well as on the Internet in branded products advertised as ‘legal highs’ or ‘research chemicals’ or as ‘food supplements’, in attempts to make these substances attractive to users.
Many hundreds of NPS have been reported for the first time in the last decade. There is no doubt that the producers of novel NPS and ‘legal highs’ are well aware of the legal framework surrounding illicit substances and are continuously replacing controlled compounds with an array of compounds, which are modified to avoid legal control. Given the very numerous possibilities for altering the structure of chemicals, the list of substances produced is likely to grow continuously.12 New substances are produced very quickly to replace those that are placed under legal control by various states.13
As the number of NPS grew rapidly, by 2013 the number of NPS already exceeded the number of psychoactive substances controlled at the international level.14 By December 2021, a total of 1,124 unique new substances have been reported to the UNODC Early Warning Advisory (EWA) on NPS by Governments, laboratories and partner organisations. These can be grouped as follows: stimulants 36%, SCRAs 29%, classic hallucinogens 15%, opioids 9%, dissociatives 3%, sedatives/hypnotics 3% and not yet assigned 5%.15, 16
In Europe, 830 new psychoactive substances were being monitored by the end of 2020 by the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA), 46 of which were detected for the first time in Europe in 2020.17
Not all NPS detected continue to be available over time, as some appear for the first time and then disappear from the market. The World Drug Reports suggest that the overall number of NPS present on the market has stabilised at approximately 500 substances per year over the period 2015–2019.
In terms of the use of NPS and despite the continuing increase in the emergence of new NPS, one study suggested that a core group of over 80 NPS have become established as recreational drugs, supplementing traditional drugs that are misused and becoming part of the repertoire of substances available for consumption.Reference Corkery, Guirguis, Papanti, Orsolini, Schifano and Zawilska18
Currently, most NPS are stimulants, followed by synthetic cannabinoid receptor agonists and a smaller number of hallucinogenics and opioids.19, 20 It has been noted that the increase in the number of opioid NPS and benzodiazepine NPS potentially signals that new psychoactive substances are increasingly more targeted at the long-term and more problematic drug users.21
Novel psychoactive substances are generally produced in bulk quantities by chemical and pharmaceutical companies often in China or India, or in clandestine laboratories in Europe. They are then shipped to Europe, where they are processed into products, packaged and marketed.22
It has been argued that these substances are not ‘legal’ but are instead ‘not prohibited’. Their non-controlled status does not reflect their safety, but rather the lack of regulation over their production, distribution and use.Reference Reuter23, Reference McNabb, Russell, Caprioli, Nutt, Gibbons and Dalley24 Many are untested and have unknown psychological and toxicological effects.Reference Peters and Martinez-Ramirez25, Reference Maurer26
Not all NPS are ‘novel’. ‘New’ does not always mean a new invention but could refer to substances that have recently been made available for recreational use, e.g. mephedrone was reportedly first synthesised in 1929, but emerged as a recreational substance of misuse as late as 2007.27 Other ‘new’ substances were synthesised and patented in the 1970s or earlier, but recently their chemistry has been modified slightly to produce psychoactive effects similar to those of well-established illicit substances.
1.5.3 Changes in Legal Control of Novel Psychoactive Substances
The legal position of some NPS has changed over time. At the international level, up to March 2019, the Commission on Narcotic Drugs placed 48 NPS under international control. These control measures have to be implemented into the national legal framework of each country.28
Other NPS continue to be outside International Drug Control Conventions. However, their legal status differs widely from country to country. To date, approximately 60 countries have implemented legal responses to control NPS by amending existing legislation or through innovative legal instruments.
Some countries have adopted controls on entire substance groups of NPS using a so-called generic approach, or have introduced analogue legislation that invokes the principal of ‘chemical similarity’ to an already controlled substance to control substances not explicitly mentioned in the legislation.29
These controls have limited the open sale of these products. They may also have played a role in reducing the number of NPS detected for the first time. However, challenges remain.
1.5.4 Development and Spread of Large Numbers of Novel Psychoactive Substances
Although the number of NPS has been growing at a very fast pace, it has been noted that this yearly increase appears to be slowing down in recent years. In Europe, it has been reported that the number of new substances identified for the first time each year peaked in 2014–2015, but has since stabilised at levels comparable to 2011–2012.30
The causes of this are unclear, however may reflect the results of sustained efforts to control new substances in Europe and legislation in some countries. This may have resulted in reducing the incentive for producers to keep ahead of legal controls and develop new compounds. In addition, control measures and law enforcement operations in China targeting laboratories producing NPS may also have played a role.31, 32
Nonetheless, and despite reduction in yearly number of NPS detected, challenges continue and new ones emerge. NPS continue to appear at the rate of one per week. There is also no evidence that the overall availability of NPS has reduced and the drugs may still be available more covertly on the illicit market.33
Some NPS are also now well-established in the drugs market, most particularly SCRAs and synthetic cathinones.34 There is also some evidence the tightening of regulation may have sometimes led to the decrease in the number of people using NPS, but users instead switched to other types of drugs.Reference Tanibuchi, Matsumoto, Shimane and Funada35
There are also changes in the type of substances being detected for the first time globally, with new substances increasingly targeted at long-term and more problematic drug users, particularly NPS synthetic opioids and benzodiazepines.36, 37, 38, 39, 40 Problematic NPS use is also increasingly found in some vulnerable groups in Europe, e.g. people who inject drugs and homeless people, and has been associated with increased levels of physical and mental health problems.41
1.6 Club Drug and Novel Psychoactive Substance Use
1.6.1 Overall Drug Use
Novel psychoactive substances have not replaced traditional illicit drugs, but exist alongside them.
Data from European countries on NPS are available from half the countries, but are often not comparable. Existing information suggests that use of NPS is overall low in comparison to traditional illicit club drugs. NPS nonetheless are consumed and are more likely to be used by some population sub-groups.
1.6.2 Club Drug Users and Contexts of Use
Different people will use substances for different reasons and each chapter in this text will look at the subjective effects of a substance desired by people who use it.
There is some research that has looked at why people use NPS specifically, which includes the fact that users turn to NPS as a substitute to traditional drugs when these are prohibited or when there is reduced supply or perceived drop in quality.Reference Measham, Moore, Newcombe and Welch42
There is also evidence that the motives for using NPS are curiosity, enhancement of social situations, the enjoyable effects, a desire to ‘get high’, and a belief that NPS are safer and more convenient.Reference Corazza, Simonato, Corkery, Trincas and Schifano43, Reference Sande44, Reference Winstock, Lawn, Deluca and Borschmann45, Reference Measham, Moore, Newcombe and Welch46
Novel psychoactive substances were also used because they were seen as facilitating a novel and exciting adventure, as promoting self-exploration and personal growth, functioning as coping agents, enhancing abilities and performance, fostering social bonding and belonging, and acting as a means for recreation and pleasure.Reference Soussan C and Andersson M47
It has been argued that the motives for NPS use may be associated with both the groups of users and the specific types of NPS being consumed. Benshop et al.’s (2020) exploratory and confirmatory factor analysis identified five factors across a number of countries: coping, enhancement, social, conformity and expansion motives. Overall, marginalised users scored higher on coping and conformity motives. Nightlife groups showed higher endorsement of social motive, whereas online community users showed higher scores on expansion motives. Various types of NPS were also associated with different motives. Motives for use of the specific substances are also discussed in the relevant sections throughout this chapter.Reference Benschop, Urbán and Kapitány-Fövény48, Reference Corazza, Simonato, Corkery, Trincas and Schifano49, Reference Johnson, Johnson and Portier50, Reference Measham, Moore, Newcombe and Welch51, Reference Sande52, Reference Werse and Morgenstern53, Reference Winstock, Lawn, Deluca and Borschmann54
Some NPS, e.g. mephedrone, are also used for sexual enhancement, including by gay and bisexual men who use it in the context of ‘chemsex’.Reference Maxwella S and Shahmanesh M55
1.6.3 Population Groups Most Likely to Use Novel Psychoactive Substances
There is evidence that levels of NPS- and drug use are higher among particular populations. These are the following:
1.6.3.1 Young People
The use of club drugs and NPS occurs in nearly all age groups, but studies have also shown that young people are more likely to use them than older people and that they are mainly used by young males.Reference Soussan C, Andersson M and Kjellgren56, Reference Soussan and Kjellgren57, Reference Bonaccorso S, Metastasio A and Ricciardi A58
In general, clubbing and club drug use, as part of a socially active lifestyle, has been associated with elevated sexual health risksReference Mitcheson, McCambridge, Byrne, Hunt and Winstock59 and a history of promiscuous sexual activity.Reference Sutherland, Peacock and Whittaker60
1.6.3.2 Poly-drug Use
The users of club drugs and NPS will typically use a wide repertoire of substances. The co-ingestion of more than one substance (simultaneous use), including alcohol, increases the risk of adverse effects,Reference Singh AK. Alcohol61 as is discussed in greater detail in later chapters of this text.
In comparison to other drug users, NPS users have higher levels of poly-drug use, and a history of overdose on any drug in the past year.Reference Sutherland, Peacock and Whittaker62
1.6.3.3 ‘Clubbers’ and People Who Frequent Night-Time Economy Leisure Venues
Studies have consistently shown that drug use is more commonly reported in surveys carried out in nightlife settings (like clubs, bars or music festivals) than among the general population.63 There is evidence that people who use the night-time economy, and dance clubs or nightclubs in particular, are more likely to use club drugs than the general population.Reference Measham and Moore64, Reference Hoare and Flatley65 Young adults attending nightlife events in pubs and discos are also more prone to poly-substance use, mainly combining NPS with alcohol and cocaine.Reference Vento, Martinotti and Cinosi66 There is also some evidence that the use of club drugs and NPS is higher among people who attend electronic dance music parties at nightclubs, festivals and ‘raves’ than those who do not.Reference Fernández-Calderóna F, Cleland CM and Palamar JJ.67, Reference Fernández-Calderón, Lozano and Vidal68, Reference Palamar, Griffin-Tomas and Ompad69, Reference Palamar, Acosta, Ompad and Cleland70, Reference Palamar, Acosta, Sherman, Ompad and Cleland71, Reference Palamar, Barratt, Ferris and Winstock72
Other targeted surveys have also shown variations by user of different types of venues in the night-time economy, e.g. those attending nightclubs reporting significantly higher levels of drug use than bar/pub attenders.Reference Measham and Moore73
There is some evidence that increased levels of drug use were associated with a higher frequency of visits to pubs, bars and nightclubs. E.g., in the UK, use of any Class A drug (including MDMA and cocaine) in the last year was around 11 times higher among those who had visited a nightclub at least four times in the past month (22.4%) compared with those who had not visited a nightclub (2.1%).74
1.6.3.4 Lesbian, Gay, Bisexual and Transgender Populations (LGBT+)
There is evidence that levels of club drug use among men who have sex with men (MSM) and among lesbian, gay, bisexual and transexual (LGBT) people, are higher than in the general population.Reference Schuler75, Reference Newcomb, Birkett and Corliss76, Reference Corliss, Rosario and Wypij77, Reference Mereish, Goldbach and Burgess78, Reference Seil and Desai79, Reference Goldbach, Tanner-Smith and Bagwell80, Reference Marshal, Dermody and Shultz81 Club drugs have been described as a popular aspect of socialisation.Reference Halkitis and Palamar82
There are concerns over associations between club drug and NPS use and high-risk sexual behaviours among a minority of MSM. This includes concern over ‘chemsex’, a term used to describe sex between men that occurs under the influence of drugs immediately preceding and/or during the sexual session,83, Reference Abdulrahim, Whiteley, Moncrieff and Club Drug84 with methamphetamine, GHB/GBL and mephedrone the drugs most often reported.
A combination of factors, including high-risk sexual practices and injecting drug use, have been described as ‘a perfect storm for transmission of both HIV and hepatitis C (HCV), as well as a catalogue of ensuing mental health problems’.Reference Kirby and Thornber-Dunwell85 Whereas not all individuals involved in ‘chemsex’ practice engage in high-risk behaviours, ‘chemsex’ has been associated with risk and adverse effects.Reference Ahmed86, Reference Evers, Hoebe and Dukers-Muijrers87, Reference Frankis, Flowers, McDaid and Bourne88, Reference Giorgetti, Tagliabracci A and Schifano F89, 90, 91, 92, 93, 94, Reference O’Reilly95, Reference Pollard, Nadarzynski and Llewellyn96, Reference Pufall97, Reference Stevens and Forrest98
1.6.3.5 Problem Drug Users
As mentioned previously, NPS are increasingly targeted at established long-term drug users, such as people dependent on opioids or benzodiazepines. In addition, in some European countries, stimulant NPS and most particularly synthetic cathinones are one of the main substances injected by problem drug users. This will be discussed in further detail below.
1.6.3.6 Homeless Populations and Prison Inmates
In some countries, synthetic cannabinoid receptor agonists (SCRAs), in particular, have been associated with homeless people and with prison populations. This will be discussed in further detail in the following.
1.6.3.7 ‘Psychonauts’
‘Psychonaut’ is a term given to a group of people who have been described as having a relatively good understanding of how NPS work, based on them experimenting with a wide variety of traditional and new substances. Psychonauts will document their experience. NPS are typically consumed in a familiar and relatively controlled environment, with dosages often carefully measured and timed. Their experiences are often made available to other psychonauts through online fora.Reference Ruane D.99
Internet sites and moderated discussion fora and blogs are used to share information about newer compounds, feedback on the effects of drugs and harm reduction advice developed through experience.100 The Internet and sites such as Drugs Forum, Bluelight and Erowid, provide platforms for sharing experience and information.Reference Schifano, Deluca and Baldacchino101 These user sites have also provided researchers with some understanding of these drugs in instances where scientific evidence was not available and it is suggested that they are a good source of information for researchers for the better understanding of NPS.102
1.6.4 New Markets and User Communication about Drugs
‘Traditional’ methods remain the most common ways to acquire drugs (dealers, friends, family), both classic drugs and NPS. However, the Internet now occupies a growing role in the sale of drugs, with significant drug sales on the darknet and the potential to grow.
Novel psychoactive substances can sometimes be bought on the ‘clearnet’ (a part of the Internet accessible to standard search engines) or from the ‘dark web’ (a part of the Internet only accessible through specialist anonymising web browsers), with the ‘darknet’ also selling controlled substances.103, Reference Corazza, Schifano and Farre104, Reference Corazza, Schifano and Simonato105, Reference Corazza, Valeriani, Bersani and Spice106, 107 It has been reported that when compared with current estimates of the annual retail value of the overall EU drug market, sales volumes on darknet markets are currently modest, but growing.108
For a growing number of people, the Internet is now the first place they look when searching for recreational drugs and their related information, especially when faced with the rapid and baffling proliferation of NPS.109 A study carried out in the Netherlands has shown that online customers are sometimes willing to pay more for the convenience of purchasing drugs online.110
The Internet has also had an impact on drug use patterns and behaviours. A UNODC 2020 publication has reported that more than a quarter of people who started using drugs before they began buying drugs on the darknet, then consumed a wider range of drugs, and approximately 10% reported that that they consumed a different class of drugs.111
Especially when not controlled, NPS have been marketed as ‘plant food’, ‘bath salts’, ‘research chemicals’, ‘incense’ or ‘herbal highs’ and are typically labelled as ‘not for human consumption’.112, Reference Hout113
There is also some evidence that NPS, as well as traditional drugs, are sometimes acquired through social media. The most commonly used technology to acquire drugs is that of mobile phones. Phone-based drug delivery services, sometimes known as ‘ring and bring drug phone lines’ or ‘dial-a-drug’ are increasingly common. This is true for NPS as well as traditional illicit substances, and the European market for cocaine has been described as undergoing a process of ‘Uberisation’, where more sellers provide ‘fast delivery anywhere at any time’.114
1.7 Brief Overview of the Effects and Harms of Club Drugs
1.7.1 How Drugs Work
Most NPS are designed to provide legal alternatives to controlled substances, and have effects similar to those associated with the controlled drugs they have been manufactured to mimic.
As mentioned previously, drugs can be classified in various ways – according to chemical structure, pharmacological activity or psychological effects.Reference Werse and Morgenstern53, Reference Winstock, Lawn, Deluca and Borschmann54, Reference Schifano115, Reference Schifano, Orsolini, Duccio Papanti and Corkery116
1.7.2 Toxicity and Other Acute Harms
The harms associated with club drugs and NPS can, as with ‘traditional’ drugs including alcohol, be ranked based on the relative harms.Reference van Amsterdam, Nutt, Phillips and van den Brink117
‘Toxicity’ generally refers to the extent to which a substance causes functional or systemic damage to a living organism.Reference Gable118, Reference Gable119
Our knowledge of the effects and toxicity of many NPS remains limited, as it is often mainly based on user reports and clinical intoxication cases, with very limited pharmacological and toxicological data available.Reference Luethia D, Kolaczynskaa KE, Doccia L, Krähenbühla S, Hoenerb MC and Liechti ME.120
There is nonetheless enough evidence to show that club drugs and NPS are associated with a range of harms.121 The growing market for new substances has been linked to an increase in the number of serious adverse events – particularly non‐fatal and fatal poisonings.Reference Elliott S and Sedefov R122, 123, Reference Evans‐Brown and Sedefov124
There are wide variations in the toxicity of the various club drugs and NPS, including their single-dose lethal toxicity.Reference Gable125 An index for fatal toxicity has been developed, showing differences between the various NPS and demonstrating that GHB/GBL, AMT, synthetic cannabinoid receptor agonists (SCRAs) and benzofurans had a higher fatal toxicity than other NPS.Reference King LA and Corkery JM.126 In recent years, benzodiazepine NPS have also been linked with fatalities, such as the case of etizolam and other ‘street’ benzodiazepines.127 Similarly, new opioids including fentanyl NPS have been associated with high levels of acute toxicity.
The harm associated with any drug of potential misuse may include: the physical and mental health harms to the individual user caused by the drug; overdose; the dependence-inducing potential of the drug; and the effects of drug use on families, communities and society.Reference Nutt, King, Saulsbury and Blakemore128 All aspects need to be considered when assessing the impact of a drug.
In addition, individuals vary greatly with respect to metabolism and vulnerability to physical and mental health problems. A number of other factors are also linked to acute toxicity:
The consumption of more than one substance will increase the chances of acute toxicity, particularly when drugs with similar physiological effects are combined (e.g. sedatives such as GHB and alcohol, or stimulants such as cocaine and amphetamine).
The risk of overdose is increased by repeated administration of the drug.
The safety ratio of drugs does not reflect the metabolic or functional tolerance that a user may have developed.
Non-drug variables can alter toxic reactions significantly (e.g. the psychological effects of the environment, diet, stress, expectation etc.).Reference Bonaccorso S, Metastasio A and Ricciardi A58, Reference Gable129
The mode of administration, with injecting not only exposing the user to the risk of bacterial infections but also increasing the risk of overdose and dependence.130
Drug purity and adulterants can affect toxicity.
Club drugs and NPS pose a particular challenge to clinicians and constitute a public health challenge for the following reasons:Reference Corazza, Schifano and Farre131
these substances are not approved for human consumption;
they are associated with a number of unknown adverse effects;
insufficient information is available in peer-reviewed scientific journals on harms;
they appear in increasingly sophisticated (i.e. non-powder) forms and remain unregulated;
they are often synthesised in underground laboratories by modifying the molecular structure of controlled drugs, raising concerns over the presence of contaminating agents;
they are largely available online to everyone, ‘just a click away’.
Whereas all users of club drugs face the risk of acute toxicity, the harms caused by club drugs encompass a wide range of different patterns. Club drugs are associated with harmful use, which can be physical harms (e.g. ketamine can lead to ulcerative cystitis) or mental (e.g. psychosis associated with synthetic cannabinoids).
Although still limited, we have an increasing understanding of the harms associated with NPS through animal and human studies.Reference Costa, De Luca, Piras, Marongiu, Fattore and Simola132
Recently, information has been provided through the Tox-Portal, an online tool developed in collaboration with The International Association of Forensic Toxicologists (TIAFT) that collects data on toxicology and harm related to the use of NPS at a global level.133 This has shown the following:
synthetic cannabinoids, synthetic opioids and synthetic stimulants account for the majority of NPS reported to the UNODC EWA Toxicology Portal.
Synthetic cannabinoids in particular remain harmful, persistent and prevalent.
Poly-drug use continues to be a factor and an important consideration in NPS fatalities.
Benzodiazepine-type NPS feature highly in cases of driving under the influence of drugs.134
Some NPS have also been shown to have a liability to produce dependence and some have been associated with a withdrawal syndrome, which can be severe, for example in the case of GHB/GBL.
1.7.3 Particular Challenges of Novel Psychoactive Substances
1.7.3.1 Unpredictability of Novel Psychoactive Substances: Products Which Are Not What They Claim to Be
The non-regulated production techniques involved in manufacturing NPS create large variation in dosage, potency or even the content of an NPS product, making it difficult to predict effects on users. There are, of course, no regulations concerning content, potency, point of sale and purchase ageReference Guirguis A, Girotto S, Berti B and Stair JL135, and even branded products that look the same and have similar lists of chemical content, may in fact be very different.
Although unpredictability of the content of a product was also a factor with traditional substances to an extent, it is argued that what is distinctive about NPS is that this is significantly more so than with traditional drugs.Reference Addison M, Stockdale K and McGovern R136
People using NPS often have poor knowledge of what they are consuming. The reasons for this include:
Research has shown that there is significant variation in the content of ‘legal high’ products bought over the Internet.Reference Brandt, Sumnall, Measham and Cole137, Reference Brandt, Sumnall, Measham and Cole138, Reference Davies, Wood and Smith139, Reference Ramsey, Dargan and Smyllie140, Reference Ayres and Bond141, Reference Baron, Elie and Elie142
NPS preparations and products sold for recreational purposes can include a combination of different NPS and/or traditional drugs. Products can contain a mixture of two or three different active compounds (including controlled compounds).143 This can increase the risk of adverse effects, as well as potentially altering clinical presentations.
For example, the analysis of samples seen by the Home Office Forensic Early Warning System (FEWS) – 2016/2017 showed that 35% of the samples analysed contained a mixture of two or more substances .144
Branded products of the same name can contain different active compounds, depending on time, place and batch purchased.Reference Baron, Elie and Elie145, Reference James, Potts and Thomas146, Reference Kalasinsky, Hugel and Kish147, Reference Parrott148, Reference Cole, Bailey, Sumnall, Wagstaff and King149, Reference Tanner-Smith150 One study found that six out of seven products analysed did not contain the advertised active ingredients but, rather, some controlled traditional drugs.Reference Baron, Elie and Elie151
Research to shed light on the purity and price of 10 NPS in the European Union (France, United Kingdom (UK), the Netherlands, Czech Republic and Poland) investigated the products in each of these countries purchased from different webshops. The study found that a considerable proportion of NPS were mislabelled by the webshops. In most instances, highly similar NPS analogues were sold instead of the specific compounds advertised. However, in some cases, the contents were entirely different to those advertised, the consequences of which could cause serious harm. For instance, α-PVP is a much more potent stimulant than 4-FA and it was present in one sample advertised as 4-FA.Reference Brunt, Atkinson and Nefau152
In some cases, studies have shown that NPS analogues similar to more commonly used substances were sold instead of the specific compounds advertised.Reference Brunt, Atkinson and Nefau153 Sometimes much stronger substances were used than the one advertised. For example, NPS drugs with hallucinogenic effects such as 25I-NBOMe have been sold as LSD to users who were not aware that they have consumed other substances, with a considerably higher dose than equivalent doses of LSD.Reference Brunt, Atkinson and Nefau154
Similarly, NPS are sometimes substituted in place of traditional drugs or other NPS and consumed by users who are not aware of the substitution. In some cases, much more potent substitutions are made. Later chapters will look for example at substitution of MDMA by PMA/PMMA, LSD by 25I-NBOMe,Reference Kalasinsky, Hugel and Kish155, Reference Parrott156, Reference Cole, Bailey, Sumnall, Wagstaff and King157, Reference Tanner-Smith158 or fentanyl substituted for, or used to adulterate, heroin.Reference Ciccarone, Ondocsin and Mars159, Reference Unick and Ciccarone160, Reference Tomassoni161, Reference Fairbairn, Coffin and Walley162, Reference Krause, Plörer and Koller163, Reference Cicero, Ellis and Kasper164, Reference Ciccarone, Ondocsin and Mars165 As will be discussed later, this can be associated with severe harm and overdose.
1.7.3.2 New Generations of Substances and Novel Psychoactive Substances Over the Years
The ‘market’ for club drugs and NPS appears to have gradually become more sophisticated. For example, a Spanish study of 2C-B reported that samples collected appeared to change over time from poorly elaborated forms such as powder, to tablets, which become the most common form.Reference Caudevilla-Gálligo, Riba and Ventura166
Importantly, new formulations of various NPS have become available over time. They are often more potent than earlier forms and may be associated with greater harms. For example,
Four generations of synthetic cannabinoid receptor agonists ((SCRA). Newer generations appear to be associated with severe adverse reactions, such as catatonia, serious toxicity and death. (For more information see Chapter 13)
New generation synthetic cathinones. E.g. compounds such as α-PVP and MDPHP (also known as ‘monkey dust’) are associated with more severe effects than previous cathinones. (For more information see Chapter 11)
Hallucinogens. For example, 25B-NBOMe is a highly potent 2C-B derivative even at microgram-level doses. (For more information see Chapter 14.)
1.7.3.3 Limited Drug Testing
One of the attractions of NPS to people who use them is the limited ability of standard drug tests to identify them. This may lead the user to feel that they can use NPS without risk of detection by occupational services or law enforcement.
This, however, can pose challenges to clinicians. There are currently very limited accurate clinic-based testing devices for most of the NPS, despite continued developments in the area of chemical standards, analytical capability and forensic detection of compounds.
It has been argued that although toxicological screening tests are not routinely used in most hospitals across Europe, they can be helpful, mostly in cases of use of unknown agents and unclear clinical presentations, provided that the results are rapidly available and interpreted correctly.167
In addition, not all laboratories have the capacity to detect the more uncommon substances. Reference standards are essential for forensic and toxicological investigations for new psychoactive substances; however, these are not available in many laboratories.168
The diagnosis of acute toxicity associated with NPS will in most cases be made by clinical assessment. As rapid urine or serum field tests are not commonly available, analytical assessment should not be considered a component of routine diagnosis of NPS. Assessment should be based on the recognition of the clinical toxidrome associated with the NPS used and the potentially harmful modes of use, with other causes of presentation excluded.
1.8 Response to Club Drug and Novel Psychoactive Substance Use
1.8.1 Novel Psychoactive Substance and Drug-Related Presentations to Hospital Emergency Departments
Accurate data on emergency hospital admissions resulting from club drug and NPS use in the UK were difficult to obtain for a variety of reasons, not least because ICD-10 codes did not include specific codes for NPSReference Wood DM, De La Rue L and Hosin AA169, Reference Wood, Conran and Dargan170, Reference Shah, Wood and Dargan171 and because coding is generally based on clinical condition at presentation.Reference Wood DM, De La Rue L and Hosin AA172
More recently, the new classification of substance use disorders and problems in ICD-11 includes a range of diagnostic categories that cover a broad spectrum of health conditions reflecting different levels and patterns of substance use.173 ICD-11 also covers some NPS and club drugs, for example synthetic cathinones,174 SCRAs175 and MDMA.176
It has been suggested that these changes may in part help with some of the coding issues, enabling better understanding of the burden of healthcare utilisation related to the use of a wider range of substances.Reference Wood DM, De La Rue L and Hosin AA177 However, in clinical practice, clinicians may not record drug-related codes, but codes based on clinical presentation. In addition, the rapidly emerging number of NPS means that some may not codeable under existing ICD-10 and even ICD-11 codes.
Data on acute drug-related hospital presentations associated with NPS continue to be limited,178 but have been improving. Interventions have taken place in Europe for a number of years now, including the European Drug Emergencies Network (Euro-Den), in order to address this current paucity of reliable data.Reference Wood, Heyerdahl and Yates179
Euro-Den data from 31 sentinel sites in 21 countries reported that there were 23,947 acute drug toxicity presentations reported by the Euro-DEN Plus centres over the four-year period between January 2014 and December 2017. These represented a median of 0.3% of all emergency presentations to the sentinel hospitals. Amongst those, NPS were seen in 9% of presentations over the four-year period, with significant geographical variation in the involvement of NPS in presentations.180
Data on deaths associated with club drugs and NPS also remain limited, and it has been argued that the absence of European forensic toxicology guidelines for drug-related death investigations is a barrier to improving monitoring and practice in this area.181
However, there is evidence that NPS, including synthetic opioids, synthetic cannabinoid receptor agonists and synthetic cathinones continue to be associated with acute intoxications and deaths. As with all drug-related deaths, fatalities often involve the use of more than one substance (poly-drug use).182
Emergency medicine physicians and other clinicians should seek advice on the diagnosis, treatment and care of patients who may have been poisoned with a club drug or an NPS, including from national or regional poisons information services. Interventions provided must be based on local, national and international protocols and guidelines.
1.8.2 Sexual Health Services
The association between substance misuse, including alcohol use, and high-risk sexual behaviours is well established, although evidence of a causal relationship is limited.
There is also some evidence from some countries that the prevalence of drug use is higher among the patients of sexual health services than the general population and most particularly patients who identify as men who have sex with men (MSM). For example, one study of patients at a London sexual health clinic reported significantly higher rates of past month drug use than in the general adult population in England and Wales. This was particularly so among MSM.Reference Hunter, Dargan, Benzie, White and Wood183
Patients of sexual health services who misuse alcohol and drugs have also been identified as higher-risk groups for poor sexual health outcomes. Substance misuse interventions in these settings have been recommended.184, 185, 186, 187
It has therefore been argued that sexual health services may provide opportunistic encounters to identify patterns of recreational drug use, explore motivations for use and implement strategies to reduce harms related to drug use.Reference Hunter, Dargan, Benzie, White and Wood188, 189, 190, 191 It has been suggested that patient assessment in sexual health services should include a history of alcohol and recreational drug use.192 Integrated services have also been suggested.193
1.8.3 Substance Misuse Treatment Services
International Standards for Treatment of Drug Use Disorders have been developed by the UNODC-WHO, and provide the rules and minimum requirements for clinical practice and the generally accepted principles of patient management in any healthcare system.194
A set of best practice principles that should underlay drug dependence treatment has been identified and defined by the United Nations Office for Drugs and Crime (UNODC) and the World Health Organization (WHO), and are listed in Box 1.1.195
Box 1.1 Outline of the Key Principles and Standards for the Treatment of Drug Use Disorders
Principle 1: Availability and accessibility of drug dependence treatment
Principle 2: Screening, assessment, diagnosis and treatment planning
Principle 3: Evidence-informed drug dependence treatment
Principle 4: Drug dependence treatment, human rights, and patient dignity
Principle 5: Targeting special subgroups and conditions
Principle 6: Addiction treatment and the criminal justice system
Principle 7: Community involvement, participation and patient orientation
Principle 8: Clinical governance of drug dependence treatment services
Principle 9: Treatment systems: policy development, strategic planning and coordination of services
Building on these principles, at a practical level, drug treatment services and systems can consider the following to improve their understanding:
Amending data recording tools to ensure NPS use and associated adverse health effects are accurately recorded
Engaging in research to build the evidence base for treatment interventions
1.8.4 Overview of the Interventions for the Screening, Identification and Management of Drug Harms in the Target Settings
The different target organisations (treatment settings) of the NEPTUNE guidance have different roles in the detection, identification and management of chronic harms and/or dependence resulting from the use of club drugs and NPS. This is determined by the competence of clinicians to deliver substance misuse treatment and particular pharmacological, psychosocial and recovery interventions.
Table 1.2 provides a summary of the role of each of the target settings and the aims of the interventions provided in terms of the screening, identification, assessment and management of the harms linked to the use of club drugs. Further information on the level of intervention needed is also presented in Chapter 2.
Table 1.2 The role of particular settings and the aims of interventions provided
| Detection | Assessment | Brief intervention | Complex intervention (acute) | Complex intervention (chronic) | |
|---|---|---|---|---|---|
| Primary care | ✓ | ✓ | ✓ | ||
| Emergency department | ✓ | ✓ | ✓ | ✓ | |
| Sexual health | ✓ | ✓ | ✓ | ||
| Substance misuse treatment | ✓ | ✓ | ✓ | Some | ✓ |
1.9 Reducing Drug-Related Harms
The reduction of the harms associated with the use of club drugs and NPS are to a very large extent based on the same principles that must be adopted for the reduction of harms associated with traditional drugs.
A number of measures are adopted by users or recommended by professionals, including regulating the quantity of drugs used, spacing out doses within a session of substance use, and not combining multiple stimulants or depressants.Reference Panagopoulos and Ricciardelli196, Reference Fernández-Calderón, Lozano-Rojas and Rojas-Tejada197, Reference Greenspan, Aguinaldo and Husbands198, Reference Cruz199
A study has shown that polysubstance-using festival attendees who frequently adopt dosing-related harm reduction strategies frequently experience less drug-related harm. However, whereas many users will adopt harm reduction strategies frequently, others will rarely carry out protective strategies, suggesting that there is still a need to encourage use of these strategies among this population.Reference Fernández-Calderón F, Díaz-Batanero C and Barratt MJ200