Book contents
- Practical Healthcare Epidemiology
- Practical Healthcare Epidemiology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Section 1 Getting Started
- Section 2 Infection Prevention Basics
- Chapter 6 Epidemiologic Methods in Infection Control
- Chapter 7 Isolation
- Chapter 8 Disinfection and Sterilization in Healthcare Facilities
- Chapter 9 Improving Hand Hygiene in Healthcare Settings
- Chapter 10 Surveillance: An Overview
- Chapter 11 Outbreak Investigations
- Section 3 Major HAI Categories: Surveillance and Prevention
- Section 4 Antimicrobial-Resistant Organisms
- Section 5 Special Settings
- Section 6 Special Topics
- Index
- References
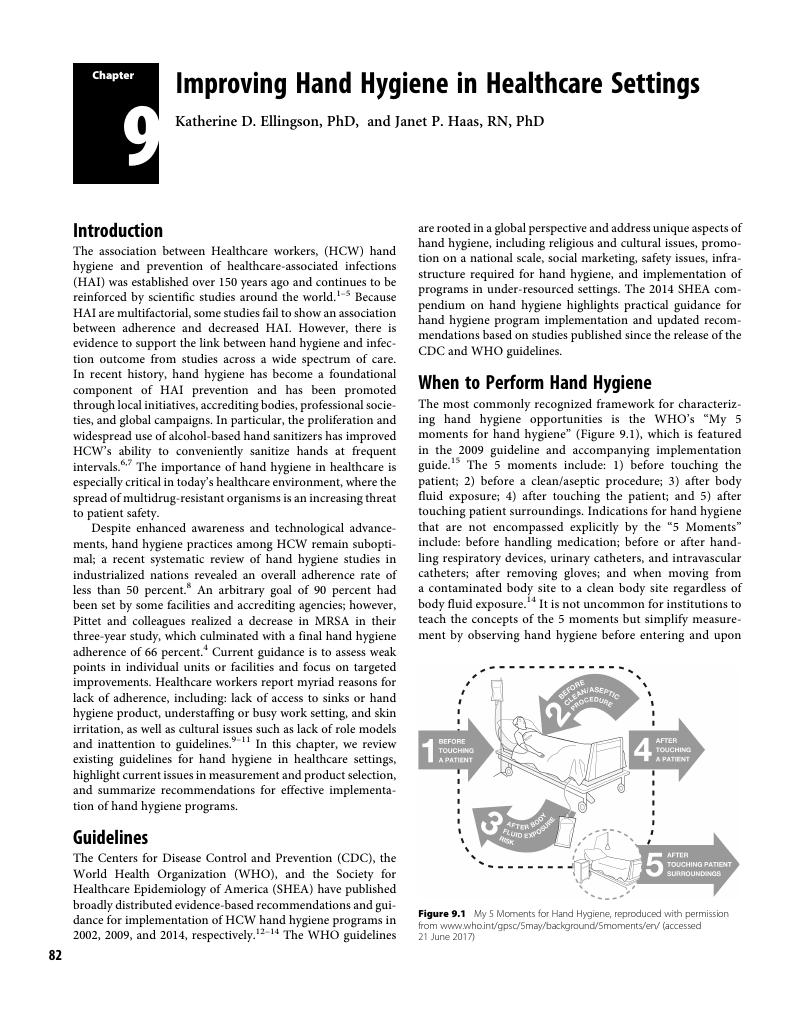
Chapter 9 - Improving Hand Hygiene in Healthcare Settings
from Section 2 - Infection Prevention Basics
Published online by Cambridge University Press: 02 April 2018
- Practical Healthcare Epidemiology
- Practical Healthcare Epidemiology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Section 1 Getting Started
- Section 2 Infection Prevention Basics
- Chapter 6 Epidemiologic Methods in Infection Control
- Chapter 7 Isolation
- Chapter 8 Disinfection and Sterilization in Healthcare Facilities
- Chapter 9 Improving Hand Hygiene in Healthcare Settings
- Chapter 10 Surveillance: An Overview
- Chapter 11 Outbreak Investigations
- Section 3 Major HAI Categories: Surveillance and Prevention
- Section 4 Antimicrobial-Resistant Organisms
- Section 5 Special Settings
- Section 6 Special Topics
- Index
- References
Summary
- Type
- Chapter
- Information
- Practical Healthcare Epidemiology , pp. 82 - 91Publisher: Cambridge University PressPrint publication year: 2018