Introduction
Veno-venous ECMO allows gas exchange and is used to support failing lungs. The cardiovascular system remains intact, and the heart continues to pump the blood around the patient’s body.
A simplified view of veno-venous ECMO is that the blood is taken from and returned to the venous system. If the blood is circulated through a functioning oxygenator, gas exchange will happen. If there is no oxygenator (or no gas flow through the oxygenator), the blood will just return in the same state as it drained (perhaps a bit cooler if no heat exchanger is in place). The whole-blood volume (including the proportion that went through the ECMO circuit) is pumped by the heart through the lungs and circulation.
Veno-venous ECMO is usually instituted in the context of severe acute respiratory failure. It supports oxygenation and CO2 removal and allows the implementation of safer ventilation strategies. This is inaccurately referred to as ‘protective’ ventilation (any positive-pressure ventilation is deemed to cause damage to the lung) and could be called the ‘least-damaging lung ventilation’.
Veno-venous ECMO can be continued for as long as appropriate; investigations are directed at confirming the underlying diagnosis and ensuring specific therapy is administered.
Patients supported with veno-venous ECMO frequently have additional non-pulmonary organ failure and require a high level of critical care support (e.g. acute renal failure).
The day-to-day management of patients on veno-venous ECMO includes all that is common to critically ill patients plus some specific elements. This chapter describes those specific elements.
Locally agreed protocols for the care of ECMO patients should be incorporated into training.
Monitoring of the patient on veno-venous ECMO has been described in Chapter 4.
Stabilization on veno-venous ECMO
Insertion of ECMO cannulas should ideally take place in an operating room. A variety of configurations can be used. It is often striking how rapidly ventilation and other support can be modified after veno-venous ECMO support has been started.
Lung ventilation can be adapted immediately after veno-venous ECMO has been established. The aim is to institute a less-damaging mechanical ventilation with lower levels of pressure. Multiple publications are available, but most clinicians would agree to aim for a standard setting (Table 8.1). Veno-venous ECMO circuits are very efficient at exchanging CO2. While unproven, it makes sense to decrease the patient PaCO2 progressively to avoid extreme vasoactive responses. This can easily be achieved by initiating veno-venous ECMO with a low gas sweep through the oxygenator (e..g 2 L/min) that is progressively increased (e.g. within the first hour). A low gas sweep will usually not affect oxygenation as transfer of O2 will be limited by other factors (as long as the delivered fraction of O2 in the sweep gas is 100%). In veno-venous ECMO, the inspired fraction of O2 in the sweep gas should always be 100%. As explained in previous chapters, oxygenation in patients supported with veno-venous ECMO is dependent on the blood flow in the circuit in relation to the patient’s cardiac output.
| Peak airway pressure <25 cmH2O (strictly less than 30 cmH2O) |
| Tidal volume ≤ 6 mL/kg |
| Positive end-expiratory pressure (PEEP) at 10 cmH20 |
| Respiratory rate at 10 min |
| FiO2 30–50% |
| Inspiratory : expiratory ratio of 1 : 2 |
| Allow spontaneous breaths within pressure and volume parameters |
Inotropes and other vasoactive drugs will often have been increased to very high levels to maintain some haemodynamic stability in critically ill patients awaiting veno-venous ECMO (often wrongly interpreted as a reason to consider veno-arterial support). This is often exacerbated by high airway and intrathoracic pressure, low O2 levels, high doses of sedative agents, high CO2 and profound acidosis. The rate of infusion of these drugs can (and should) very often be decreased rapidly.
Red blood cell transfusion is advocated by some, as the O2 content in the blood will be limited and extra red blood cells will increase the O2-carrying capacity. Others advocate the use of restrictive transfusion policies identical to those used in other critically ill patients. Justification for a liberal transfusion strategy is that veno-venous ECMO rarely increases the PaO2 to normal physiological levels. In the absence of a guarantee that a PaO2 as low as 6 kPa is acceptable, many clinicians will transfuse in the early stages of support. The increased oncotic pressure offered by red blood cell transfusion may be added benefit in critically ill patients in whom the systemic inflammatory response is increased by the use of an ECMO circuit.
If the PaO2 remains low despite optimal blood flow through the ECMO circuit, it can be presumed that the issue is either inadequate flow for body weight (especially in patients in excess of 100 kg) or high cardiac output leading to a small proportion of circulating blood going through the ECMO circuit. Solutions to this problem include: (1) the insertion of an additional drainage cannula to increase flow through the ECMO circuit as long as the return cannula can accommodate the increase in flow and pressure; and (2) measures to decrease O2 consumption (such as cooling the core temperature using the heater/cooler in the ECMO circuit to modify the patient’s body temperature) or actions to reduce the cardiac output (β-blockers are sometimes used to achieve this, but questions remain on the overall physiological impact this may have). (Note that double-lumen cannulas have an optimized return lumen size for the drainage lumen size, and that adding an extra cannula to improve flow will have only a limited effect.)
If the venous blood is highly desaturated, a second oxygenator may be incorporated into the circuit. While this is difficult to model, this definitely increases the transit time for blood in each oxygenator, and post-oxygenator PaO2 will be higher.
After stabilization, the patient can now undergo multiple non-invasive tests to determine the cause and remedy the insult that led to respiratory failure.
Oxygenation during veno-venous ECMO
During veno-venous ECMO support, fully O2-saturated blood from the ECMO circuit mixes in the right atrium with deoxygenated venous return that has not passed through the ECMO circuit, and then passes into the right ventricle and pulmonary artery.
Systemic arterial oxygenation is determined by the relative proportions of oxygenated ECMO blood flow and deoxygenated venous return, and by the degree of pulmonary dysfunction, O2 consumption, amount of recirculation in the ECMO circuit and oxygenator efficiency.
As described in Chapter 4, recirculation refers to oxygenated blood from the return cannula flowing directly to the drainage cannula of the ECMO circuit, without passing through the lungs and systemic circulation. Recirculation can be identified by high O2 saturation in the drainage limb (pre-oxygenator) of the ECMO circuit, and often by visual inspection of the drainage limb for ‘flashes’ of red oxygenated blood mixing with deoxygenated blood. The recirculation fraction increases with increasing ECMO flow. At higher ECMO flow rates, the beneficial effect of increasing flow on the proportion of oxygenated blood entering the pulmonary artery will be offset by an increase in recirculation. In these circumstances, reducing pump speed may actually result in improved oxygenation. Recirculation is higher with a suboptimally positioned ECMO cannula (the best distance between the tip of two cannulas is said to be 10 cm), low cardiac output and low intravascular (specifically right atrial) volume.
ECMO blood flow should initially be set to deliver the maximum flow, typically 5 L/min, without excessive negative pressure in the drainage limb of the ECMO circuit; this should produce a rise in arterial O2 saturation. Sweep gas should be kept at 100% O2. Thereafter, oxygenation can be controlled by adjusting circuit blood flow and not by altering FiO2 or positive end-expiratory pressure (PEEP) on the ventilator. Generally a PaO2 greater than 6 kPa (50 mmHg) and O2 saturation greater than 85% are adequate. Occasionally, lower values have to be accepted.
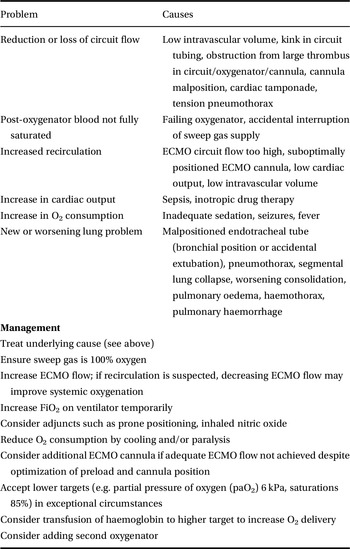
Hypoxaemia while on veno-venous ECMO should be assessed and managed as outlined in Table 8.2.
| Problem | Causes |
|---|---|
| Reduction or loss of circuit flow | Low intravascular volume, kink in circuit tubing, obstruction from large thrombus in circuit/oxygenator/cannula, cannula malposition, cardiac tamponade, tension pneumothorax |
| Post-oxygenator blood not fully saturated | Failing oxygenator, accidental interruption of sweep gas supply |
| Increased recirculation | ECMO circuit flow too high, suboptimally positioned ECMO cannula, low cardiac output, low intravascular volume |
| Increase in cardiac output | Sepsis, inotropic drug therapy |
| Increase in O2 consumption | Inadequate sedation, seizures, fever |
| New or worsening lung problem | Malpositioned endotracheal tube (bronchial position or accidental extubation), pneumothorax, segmental lung collapse, worsening consolidation, pulmonary oedema, haemothorax, pulmonary haemorrhage |
| Management | |
| Treat underlying cause (see above) | |
| Ensure sweep gas is 100% oxygen | |
| Increase ECMO flow; if recirculation is suspected, decreasing ECMO flow may improve systemic oxygenation | |
| Increase FiO2 on ventilator temporarily | |
| Consider adjuncts such as prone positioning, inhaled nitric oxide | |
| Reduce O2 consumption by cooling and/or paralysis | |
| Consider additional ECMO cannula if adequate ECMO flow not achieved despite optimization of preload and cannula position | |
| Accept lower targets (e.g. partial pressure of oxygen (paO2) 6 kPa, saturations 85%) in exceptional circumstances | |
| Consider transfusion of haemoglobin to higher target to increase O2 delivery | |
| Consider adding second oxygenator | |
Mechanical ventilation in patients during veno-venous ECMO
Decreasing the impact of mechanical ventilation is thought to be one of the reasons that veno-venous ECMO is of benefit in patients with acute lung injuries.
Ventilator-associated lung injury can be limited by reducing the tidal volume and airway pressures. As the gas exchange is almost fully supported by ECMO, a reduction in mechanical ventilation will allow less-damaging ventilation, so-called ‘protective’ ventilation. Most patients can be managed with tidal volumes lower than 6 mL/kg of predicted body weight and peak airway pressures lower than 25 cmH2O.
It is possible to stop all mechanical ventilation. In some scenarios, this is the only option available (e.g. massive lung haemorrhage). It is unknown whether the absence of ventilation is better than a low level of mechanical ventilation.
Selected patients can be woken up during veno-venous ECMO, extubated and left to breathe spontaneously. (The respiratory drive can be decreased or even stopped by adjusting the level of gas sweep across the oxygenator. Some patients may be awake and talking but not ventilating.)
High-frequency oscillatory ventilation is an alternative approach to providing ‘protective’ ventilation, and may be useful in combination with ECMO in patients with severe barotrauma. In these situations, ultra lung rest may be provided by using high-frequency oscillatory ventilation with a low mean airway pressure.
Tidal volume and peak inspiratory pressure
An ideal tidal volume of 6 mL/kg is merely an arbitrary volume chosen by the Acute Respiratory Distress Syndrome Clinical Network (ARDSNet) investigators and shown to be better than a higher volume. In fact, sick lungs may not be able to accommodate a tidal volume of 6 mL/kg.
Selecting a maximum peak pressure is an added safety measure, as the plateau pressure will be lower. Ideally, the chosen pressure should be below the upper inflection point on a pressure–volume curve (after which the pressure rises rapidly with no increase in volume).
The transthoracic pressure is theoretically more important, and multiple measures can be taken. In practical terms, limiting the peak airway pressure to a maximum of 30 cmH2O seems to be right. Most patients can be managed with peak airway pressures lower than 25 cmH2O.
Positive end-expiratory pressure
The best PEEP is the one that avoids alveolar collapse and lowers wall stress on inflation. It should not affect the patient’s haemodynamic status to a great extent.
The pressure–volume curve can be helpful, as the opening pressure can be seen as the lung starts to inflate, but its interpretation can be complex and it needs to account for lung hysteresis. Moreover, this is compounded by the fact that the lung, even more so when diseased, is not homogenous.
Patients with bronchospasm may trap some air, building their own PEEP.
Mode of ventilation
Pressure control modes are the most logical modes of ventilation in patients with lung injury. Alternatively, volume control modes with a strict limit in the set peak pressures allow a reduction of the damaging effects of mechanical lung ventilation.
Spontaneous modes can be used in awake patients. Of note, awake patients with severe lung injury will often appear distressed because they are tachypnoeic. Tachypnoea is not always a sign of distress, as a small lung vital capacity will lead to an earlier triggering of stretch receptors, leading to a compensatory high respiratory rate.
Adjuncts to mechanical ventilation
Fluid balance
Removing excess water optimizes lung mechanics and pulmonary gas exchange. This should be initiated as soon as possible after veno-venous ECMO initiation.
Removing excess water may be difficult in the first few hours of ECMO support because of the acute response caused by the primary insult and the intense inflammatory response caused by the ECMO circuit. It is, however, critical to ensure that this happens as soon as the acute inflammatory response is controlled and stability has been established.
Tracheostomy
Tracheotomy, either percutaneous or surgical, may be performed to provide a more secure airway, facilitate a reduction in sedation, improve comfort and ultimately aid weaning from ventilation.
However, tracheostomy increases the risk of major haemorrhage, and this should be assessed in each patient. Early tracheostomy has not been shown to be associated with increased survival.
In selected patients, tracheal extubation (with or without non-invasive ventilation) can be considered, with the potential benefits of reducing the risks of oropharyngeal instrumentation and orotracheal intubation, improving communication and aiding compliance with rehabilitation.
Prone positioning
Prone positioning of adult patients on veno-venous ECMO may be considered. It can be done safely and effectively as long as great care is taken to secure all tubes and lines, and ensuring all pressure areas are well protected.
In addition to improving ventilation–perfusion relationships, it facilitates the drainage of pulmonary secretions, and may reduce right ventricular pressure overload and ventilator-associated lung injury.
Inhaled nitric oxide
Inhaled nitric oxide improves oxygenation in patients with acute lung injury by improving ventilation–perfusion matching and lowering pulmonary vascular resistance. Clinical trials have not demonstrated a mortality benefit, and it has no place in the management of the patient on veno-venous ECMO.
Key points
Veno-venous ECMO allows gas exchange in the venous blood.
The institution of least-damaging lung ventilation is thought to be beneficial.
Patients can be extubated and breathe spontaneously on veno-venous ECMO.