Staffing
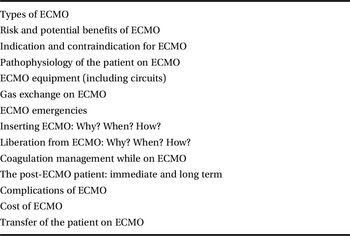
An ECMO service is entirely dependent on its people. The team is organized to provide a continuous service, 24 h a day. Table 2.1 provides an example of a list of the key members of the team. This will vary from centre to centre, depending on local and national organizational factors.
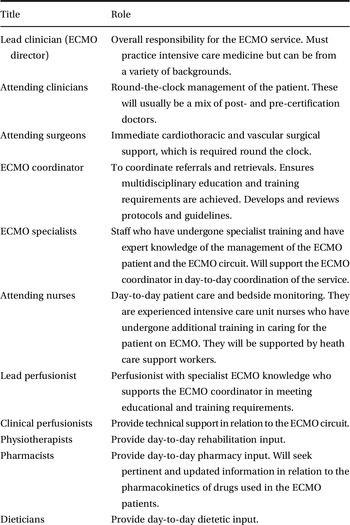
All members of the team require specialist knowledge in managing the ECMO patient, and a robust teaching programme should be established. The volume of activity of a centre should be sufficient to allow availability of the required resources for training. Staff training should be mandatory. Regular refreshers should be provided and competencies regularly assessed. Table 2.2 lists the topics that the in-house training programme should cover. The ELSO provides regularly updated guidelines and resources for the training and continuous education of the ECMO specialist.
Table 2.2 Specialized topics to be covered in the training of an ECMO clinician
| Types of ECMO |
| Risk and potential benefits of ECMO |
| Indication and contraindication for ECMO |
| Pathophysiology of the patient on ECMO |
| ECMO equipment (including circuits) |
| Gas exchange on ECMO |
| ECMO emergencies |
| Inserting ECMO: Why? When? How? |
| Liberation from ECMO: Why? When? How? |
| Coagulation management while on ECMO |
| The post-ECMO patient: immediate and long term |
| Complications of ECMO |
| Cost of ECMO |
| Transfer of the patient on ECMO |
The team of educators must be allocated time and resources to attend state-of-the-art conferences. Educators can then ensure their local programme is up to date. Training should include regular water drills, during which a primed circuit is used without being connected to a patient. This allows familiarization with the equipment and identification of potential issues. Staff are trained to recognize and manage specific ECMO emergencies, and then do it again and again.
A list of competencies expected from each role for clinicians involved in the management of the patient on ECMO is useful. These can be developed at the local or national level, and the ELSO provides examples and ready-to-use lists.
Multidisciplinary meetings should be scheduled on a regular basis and newly acquired knowledge and experience shared to ensure the whole team continues to learn and evolve.
Doctors
Doctors looking after ECMO patients will require multiple skills. The ideal ECMOlogist would be a surgeon, intensivist, chest physician and anaesthesiologist combined. This person should have acquired the skills of many different specialities. As this is rather unusual, a good ECMOlogist will be a ‘connexist’, i.e. someone who can recognize his/her own limitations and call on others’ expertise. The closest to this ideal are intensive care doctors as they are usually working in this manner.
The starting point for any doctor wishing to learn ECMO is a thorough understanding of the ECMO circuit itself (see Chapter 3). The second key clinical skill to acquire is how to select the right patients, i.e. patients requiring support while recovering from a reversible insult or eligible for another type of long-term support (see Chapter 5).
The ECMO community has a great tradition of supporting each other. These days, multiple courses are available to teach the basics of ECMO. Clinicians involved in ECMO are always willing to help each other.
Adult intensive care skills are central to the safe delivery of ECMO, and all the basics of intensive care management should be adhered to.
ECMO is a complete system of care, not just a bolt-on accessory.
Junior doctors should be involved in all aspects of the care of ECMO patients. The first skill they will need to acquire is to recognize their limitations and when to call for help.
ECMO specialist
The ECMO specialist has a key role. They are immediately available in the clinical area and are the first line between ECMO and the patient. They require advanced skills to ensure no harm comes to the patient. They are the first line in managing the patient and circuit emergencies and, in addition to excellent technical skills, should have effective communication skills and the ability to work in stressful situations.
The ECMO specialist will be skilled in the care of patients on ECMO, and should have a strong intensive care background.
The ECMO specialist must achieve competency through completing the necessary training and assessment. Practical skill sessions concentrate on circuit surveillance, troubleshooting and emergency procedures. Emergency procedures such as air embolus removal are practised repeatedly to ensure competency.
The ECMO specialist can undertake other roles, such as ensuring appropriate anticoagulation, and titrating ECMO flow and gas to ensure adequate levels of cardiac and/or respiratory support.
ECMO specialists can be nurses who have undergone additional training, or can come from other specialities, such as perfusion or medical backgrounds.
All nurses caring for the ECMO patient must have basic skills specific to both the intensive care unit (ICU) and the ECMO patient. They must be able to act immediately in a case of a catastrophic failure of the ECMO circuit. An ECMO circuit must never be left in the hands of a practitioner who is not qualified to look after it.
ECMO coordinator
The ECMO coordinator usually refers to a highly experienced ECMO specialist with clinical, educational and managerial responsibility for the ECMO programme. This person may be supported by deputy coordinators and shift leaders who are experienced ECMO specialists to ensure round-the-clock availability. They are involved in the development of all ECMO-related protocols.
This coordination is an essential part of ensuring the safety of the patient on ECMO. It ensures communication between team members and smooth management of patient referral, transport, cannulation and ongoing care.
ECMO director
The ECMO director is an ECMO clinician nominated to have overall managerial and clinical responsibility for the ECMO programme. The ECMO director does not need to dictate the care of each patient but leads a team to deliver the best possible care.
Perfusionist
Perfusionists are experts in the management of extracorporeal circuits, and their main expertise is with short-term cardiopulmonary bypass used in the operating theatre. A perfusionist will need additional training to gain the knowledge required to manage the ECMO circuit.
Perfusionists are an integral and important part of many ECMO programmes. It is usual practice in some institutions for a perfusionist to prime the ECMO circuit and initiate ECMO before handing management of the circuit over to the ECMO specialist. Once the patient is returned to the ICU and established on ECMO, the perfusionist’s role includes circuit or component replacement and transport of the patient to other areas of the hospital, such as the catheter laboratory or the computed tomography (CT) scanner.
A perfusionist who has developed a special interest in ECMO can act as the lead of all perfusionists in an institution and should ensure that knowledge and good practice are shared.
Perfusionists should be involved in circuit design and modifications, management of ordering and stock levels, equipment maintenance and development of protocols.
Transfer team
ECMO is a specialist support that may not be provided in all institutions. A centre will need a minimum number of cases per year to maintain expertise and justify the set-up expenses. Most patients requiring ECMO will need to be transferred from one centre to an ECMO centre.
Patients referred to the ECMO centre will often be unstable, and transfer on ECMO will be necessary.
The difficulty of commencing ECMO on a patient outside the comfortable surroundings of one’s own hospital should not be underestimated.
The transfer team will include at least a doctor and a transfer-trained ECMO nurse. The team must be trained and equipped to work in any of the vehicles and with all the equipment that might be used.
Other members of the team
Other doctors, nurses and allied health professionals will be involved in the care of the ECMO patient. It is helpful to try and identify one or two individuals in each department who are interested in ECMO, so that they can develop specific expertise with these patients.
Table 2.1 lists the many specialties required. Surgeons (general, cardiothoracic and vascular), physiotherapists, cardiologists, microbiologists, dieticians, haematologists, radiologists and occupational therapists are all frequently involved in care of the adult patient on ECMO. Specific knowledge will be required from each of them.
Infrastructure
An ECMO centre must be located in an area of sufficient population density to ensure that patients are regularly admitted and a minimum number are supported each year. This number is often the subject of intense debate, but we estimate that expertise and investment will be maintained if a centre supports around 20 patients per year. The relationship between volume and outcome is recognized in many clinical specialities.
The centre must be easily accessible by road, or by fixed wing or rotary aircraft. A helipad directly linked to the hospital is ideal.
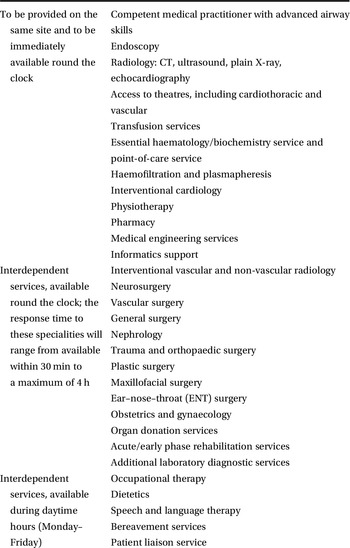
The required facilities (Table 2.3) mean that ECMO services will usually be based in tertiary referral centres that can provide round-the-clock cardiothoracic and vascular support, alongside other services such as advanced imaging and specialist microbiology.
The ECMO service will often be part of the ICU, but some centres have dedicated ECMO units. These are specialist ICUs looking solely after the ECMO patient, similar to burns units.
Adult and paediatric ECMO services have historically been combined due to the common technology. It is our opinion that patients are best served in a unit specializing in the original insult (respiratory or cardiac), rather than based on the technology used. An adult patient will not be treated the same way if supported in a paediatric ECMO unit, specialized in the management of neonates or young children with congenital diseases. Local or national organization may influence this.
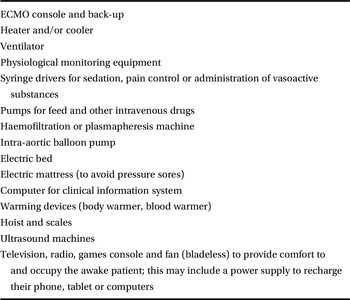
The minimum specification for the bed space is the same as that required for an intensive care patient. There must be sufficient power points (and these must be resilient in case of power failure). A patient on ECMO may require numerous devices requiring electrical power, as listed in Table 2.4. The ECMO circuit will require a gas supply in addition to that required for the ventilator.
Table 2.4 Examples of electrical devices required for a single ECMO patient
| ECMO console and back-up |
| Heater and/or cooler |
| Ventilator |
| Physiological monitoring equipment |
| Syringe drivers for sedation, pain control or administration of vasoactive substances |
| Pumps for feed and other intravenous drugs |
| Haemofiltration or plasmapheresis machine |
| Intra-aortic balloon pump |
| Electric bed |
| Electric mattress (to avoid pressure sores) |
| Computer for clinical information system |
| Warming devices (body warmer, blood warmer) |
| Hoist and scales |
| Ultrasound machines |
| Television, radio, games console and fan (bladeless) to provide comfort to and occupy the awake patient; this may include a power supply to recharge their phone, tablet or computers |
ECMO provides support for many patients with transmissible diseases that may be fatal, so it is important that isolation facilities are available. ECMO centres may have to accept several patients with identical issues (e.g. H1N1 influenza virus or Legionella outbreak, or multiple casualties following a blast or chemical injuries). The possibility of grouping patients as a cohort (i.e. isolation of a group of patients) should be available. The team should be trained in using personal protection equipment, and the facilities should allow full isolation. Some centres use personal protection equipment and strict isolation for all newly admitted patients with an acute respiratory disease requiring ECMO support.
The patients need access to an operating room 24 h a day, 7 days a week, and this must be easily accessible from the ICU. Similarly, patients need round-the-clock access to imaging facilities (CT scanner, cardiac catheter and cardiac electrophysiology laboratories). Access to these facilities must be straightforward, with established procedures to minimize mishaps during transfer. All these facilities should be located in the same building and ideally on the same floor (unfortunately, not many hospitals are designed this way).
ECMO equipment needs to be stored when not in use. This requires secure facilities. A technical service must be readily available. It is essential that all equipment is maintained with a programme in place to enable regular maintenance while ensuring adequate equipment is available for clinical use.
For most centres, the majority of patients will come from other centres. Retrieval processes must be in place, including appropriate transport vehicles and trolleys, adapted to the requirements of the ECMO patient (see Chapter 10).
Organization
Clear lines of accountability and good communication are key to the success of the ECMO service. The large multidisciplinary team involved in the management of these patients requires excellent coordination. Conflicting demands must be arbitrated by a clinician with experience and knowledge in the management of these patients. Examples include the general surgeon requiring that anticoagulation be discontinued after a laparotomy in a patient with an arterial reperfusion line or the cardiologist requiring a set of cardiac outputs via a pulmonary artery catheter. The ECMO team must reconcile these differences, assess the risk/benefit ratio between conflictual demands and sometimes make very difficult decisions.
The ECMO service will be intrinsically linked to other services and must have access to a vast range of highly specialized experts. For patients requiring ECMO due to cardiac failure (see Chapter 9), the availability and involvement of heart failure physicians and surgeons is indispensable. These patients may only be able to progress to a permanent ventricular assist device or heart transplantation. For patients with respiratory failure and requiring ECMO, the availability and involvement of physicians with a variety of interests are required. These interests include lung transplantation, interstitial lung disease, chronic obstructive pulmonary disease and vasculitis.
Systemic review of patients on ECMO by a multidisciplinary team happens in the same way as for other critically ill patients. Dedicated clinical multidisciplinary meetings are essential and must be part of the routine of the unit.
As most patients will be referred from other centres, systems should be in place to allow for the triage and retrieval of these patients. Each unit will have appropriate mechanisms to record patient details and clinical reasoning leading to the decision to admit or not and to commence ECMO or not.
The financial and business administration of the programme is often overlooked in this type of book but is increasingly important. ECMO is an expensive mode of support that may be perceived as wasteful by colleagues in other specialities, especially if patient dies after a prolonged duration of support. Data to support expenditures must be collected.
The impact on other services must be recognized. ECMO is resource intensive, and this is sometimes detrimental to other patients, as the ICU facility may not be available or staff may be occupied by the demands of ECMO patients.
Clinical governance should include continuous data collection and analysis. Benchmarking against others, such as reporting to an international registry (see Chapter 15), is important. A review of all patients referred (admitted or not) should be conducted at regular intervals. A registry of clinical incidents should be kept and the lessons learnt shared.
All protocols and guidelines should be easily accessible and regularly updated.
Regular national and international meetings, as well as peer review by other clinicians running similar services, can help to improve quality.
A research programme should ideally be in place. This can range from supporting multicentre projects to multidisciplinary collaboration or in-house complex innovative projects. Appropriate resources need to be allocated.
ECMO centres admitting patients with respiratory disease should be part of a sentinel network to allow rapid detection of new virulent pathogens (e.g. Legionella, Middle East respiratory syndrome coronavirus (MERS-CoV), H1N1 influenza virus or emerging pathogens).
Key points
ECMO requires a multidisciplinary team, with many roles available around the clock.
The ECMO service must be part of a larger network of services, only possible in large centres.
A large referral population is required to ensure that the ECMO service maintains its expertise.