Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Esfahani, Hamid
Darvishghanbar, Mahsa
and
Farshid, Behzad
2018.
Enhanced bone regeneration of zirconia-toughened alumina nanocomposites using PA6/HA nanofiber coating via electrospinning.
Journal of Materials Research,
Vol. 33,
Issue. 24,
p.
4287.
Luo, You-Ran
Zhang, Li
Chen, Cheng
Sun, Dong-Yuan
Wu, Peng
Wang, Yue
Liao, Yun-Mao
Cao, Xiao-Yan
Cheng, Cheng-Kung
Tang, Zi-Qing
and
Liang, Xing
2018.
The delayed degradation mechanism and mechanical properties of β-TCP filler in poly(lactide-co-glycolide)/beta-tricalcium phosphate composite suture anchors during short-time degradation in vivo.
Journal of Materials Research,
Vol. 33,
Issue. 24,
p.
4278.
Thomas, Ashley
Johnson, Eldin
Agrawal, Ashish K.
and
Bera, Japes
2019.
Preparation and characterization of glass–ceramic reinforced alginate scaffolds for bone tissue engineering.
Journal of Materials Research,
Vol. 34,
Issue. 22,
p.
3798.
Moncal, Kazim K.
Aydin, R. Seda Tigli
Abu-Laban, Mohammad
Heo, Dong N.
Rizk, Elias
Tucker, Scott M.
Lewis, Gregory S.
Hayes, Daniel
and
Ozbolat, Ibrahim T.
2019.
Collagen-infilled 3D printed scaffolds loaded with miR-148b-transfected bone marrow stem cells improve calvarial bone regeneration in rats.
Materials Science and Engineering: C,
Vol. 105,
Issue. ,
p.
110128.
Dong, Tao
Mi, Ruixin
Wu, Mi
Zhong, Nongping
Zhao, Xia
Chen, Xin
and
Shao, Zhengzhong
2019.
The regenerated silk fibroin hydrogel with designed architecture bioprinted by its microhydrogel.
Journal of Materials Chemistry B,
Vol. 7,
Issue. 27,
p.
4328.
Li, Yuchao
Liao, Chengzhu
and
Tjong, Sie Chin
2019.
Synthetic Biodegradable Aliphatic Polyester Nanocomposites Reinforced with Nanohydroxyapatite and/or Graphene Oxide for Bone Tissue Engineering Applications.
Nanomaterials,
Vol. 9,
Issue. 4,
p.
590.
Moncal, Kazim K.
Ozbolat, Veli
Datta, Pallab
Heo, Dong N.
and
Ozbolat, Ibrahim T.
2019.
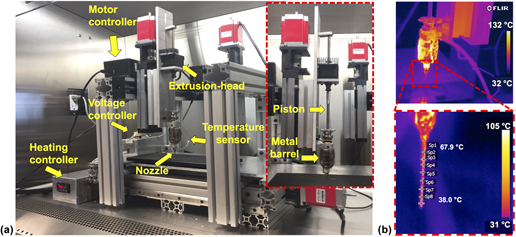
Thermally-controlled extrusion-based bioprinting of collagen.
Journal of Materials Science: Materials in Medicine,
Vol. 30,
Issue. 5,
Thilakan, Jaya
Mishra, Ruchi
Goel, Sudhir K.
and
Arya, Neha
2019.
Biomaterials in Orthopaedics and Bone Regeneration.
p.
175.
Fathi-Achachelouei, Milad
Keskin, Dilek
and
Tezcaner, Aysen
2020.
Biomaterials for Organ and Tissue Regeneration.
p.
113.
Gerdes, Sam
Mostafavi, Azadeh
Ramesh, Srikanthan
Memic, Adnan
Rivero, Iris V.
Rao, Prahalada
and
Tamayol, Ali
2020.
Process–Structure–Quality Relationships of Three-Dimensional Printed Poly(Caprolactone)-Hydroxyapatite Scaffolds.
Tissue Engineering Part A,
Vol. 26,
Issue. 5-6,
p.
279.
Kampleitner, Carina
Changi, Katayoon
Felfel, Reda M.
Scotchford, Colin A.
Sottile, Virginie
Kluger, Rainer
Hoffmann, Oskar
Grant, David M.
and
Epstein, Michelle M.
2020.
Preclinical biological and physicochemical evaluation of two-photon engineered 3D biomimetic copolymer scaffolds for bone healing.
Biomaterials Science,
Vol. 8,
Issue. 6,
p.
1683.
Mota, Carlos
Camarero-Espinosa, Sandra
Baker, Matthew B.
Wieringa, Paul
and
Moroni, Lorenzo
2020.
Bioprinting: From Tissue and Organ Development to in Vitro Models.
Chemical Reviews,
Vol. 120,
Issue. 19,
p.
10547.
Ghorbani, Farnaz
Li, Dejian
Ni, Shuo
Zhou, Ying
and
Yu, Baoqing
2020.
3D printing of acellular scaffolds for bone defect regeneration: A review.
Materials Today Communications,
Vol. 22,
Issue. ,
p.
100979.
Kim, JuYeon
Kim, WonJin
and
Kim, GeunHyung
2020.
Scaffold with micro/nanoscale topographical cues fabricated using E-field-assisted 3D printing combined with plasma-etching for enhancing myoblast alignment and differentiation.
Applied Surface Science,
Vol. 509,
Issue. ,
p.
145404.
Pitjamit, Siwasit
Thunsiri, Kittiya
Nakkiew, Wasawat
Wongwichai, Tunchanok
Pothacharoen, Peraphan
and
Wattanutchariya, Wassanai
2020.
The Possibility of Interlocking Nail Fabrication from FFF 3D Printing PLA/PCL/HA Composites Coated by Local Silk Fibroin for Canine Bone Fracture Treatment.
Materials,
Vol. 13,
Issue. 7,
p.
1564.
Doyle, Stephanie E.
Henry, Lauren
McGennisken, Ellen
Onofrillo, Carmine
Bella, Claudia Di
Duchi, Serena
O'Connell, Cathal D.
and
Pirogova, Elena
2021.
Characterization of Polycaprolactone Nanohydroxyapatite Composites with Tunable Degradability Suitable for Indirect Printing.
Polymers,
Vol. 13,
Issue. 2,
p.
295.
Wang, Zongliang
Agrawal, Prajwal
and
Zhang, Yu Shrike
2021.
Nanotechnologies and Nanomaterials in 3D (Bio)printing toward Bone Regeneration.
Advanced NanoBiomed Research,
Vol. 1,
Issue. 11,
Han, Yanting
Wei, Qianqian
Chang, Pengbo
Hu, Kehui
Okoro, Oseweuba Valentine
Shavandi, Amin
and
Nie, Lei
2021.
Three-Dimensional Printing of Hydroxyapatite Composites for Biomedical Application.
Crystals,
Vol. 11,
Issue. 4,
p.
353.
Yang, Xiangjun
Wang, Yuting
Zhou, Ying
Chen, Junyu
and
Wan, Qianbing
2021.
The Application of Polycaprolactone in Three-Dimensional Printing Scaffolds for Bone Tissue Engineering.
Polymers,
Vol. 13,
Issue. 16,
p.
2754.
Ashwin, A.J.
and
Jafferson, J.M.
2021.
State of the art direct ink writing (DIW) and experimental trial on DIW of HAp bio-ceramics.
Materials Today: Proceedings,
Vol. 46,
Issue. ,
p.
1298.