Introduction
Autism spectrum disorder (ASD) is a heterogeneous neurodevelopmental condition with a specific combination of impairments in social communication and interaction, sensory anomalies, repetitive behaviours and varying levels of intellectual disability beginning early in life (Lord et al., Reference Lord, Elsabbagh, Baird and Veenstra-Vanderweele2018, Reference Lord, Brugha, Charman, Cusack, Dumas, Frazier, Jones, Jones, Pickles, State, Taylor and Veenstra-VanderWeele2020). Neurodiversity paradigm regards ASD as a form of variation within a diversity of minds (Pellicano and den Houting, Reference Pellicano and den Houting2022) and recognises that some of ASD is also related to cognitive strengths, notably in areas such as excellent attention and memory to details, and a strong drive to detect patterns (Baron-Cohen, Reference Baron-Cohen2017; Jones et al., Reference Jones, Akram, Gordon, Murphy and Sharkie2021). Unfortunately, the impairments of ASD usually continue into adulthood in most cases, which may lead to the limited social integration of patients, poor employment prospects, a high incidence of mental health problems and a low workforce participation rate of parents or caregivers (Doran et al., Reference Doran, Einfeld, Madden, Otim, Horstead, Ellis and Emerson2012; Howlin and Magiati, Reference Howlin and Magiati2017). The estimated financial burden of supporting an individual with ASD and intellectual disability across his or her lifespan amounts to 2.4 million dollars in the USA (Buescher et al., Reference Buescher, Cidav, Knapp and Mandell2014).
The Global Burden of Disease Study (GBD) 2010 estimated that the prevalence of ASD seemed to have remained relatively stable between 1990 and 2010 (Baxter et al., Reference Baxter, Brugha, Erskine, Scheurer, Vos and Scott2015). Several new studies presumed that the incidence of ASD increased over time, but this hypothesis is based on data from administrative records rather than community-based research (Lord et al., Reference Lord, Brugha, Charman, Cusack, Dumas, Frazier, Jones, Jones, Pickles, State, Taylor and Veenstra-VanderWeele2020). According to the National Health Interview Survey in the USA, the prevalence of ASD among US children aged 3–17 years increased between 2009 and 2017 (1.1–2.5%) (Zablotsky et al., Reference Zablotsky, Black, Maenner, Schieve, Danielson, Bitsko, Blumberg, Kogan and Boyle2019). Conversely, in India, the crude prevalence of ASD was 0.4% in 2017, with a decreased trend from 1990 to 2017 (India State-Level Disease Burden Initiative Mental Disorders Collaborators, 2020). The diverse spatiotemporal changes in ASD in different countries have revealed the complexity of controlling the burden of ASD. However, the latest spatial patterns and temporal trends of ASD burden at the global, regional and national levels are still lacking, which is essential for targeted public policy-making, such as social support services and healthcare resource allocation. The GBD 2019 is the latest systematic epidemiological study of global diseases and their risk factors, which uses all known data on diseases or disorders from administrative and community survey sources to establish and analyse correlations to assess trends, thereby making the data more systematic and reliable (GBD 2019 Diseases and Injuries Collaborators, 2020; GBD 2019 Risk Factors Collaborators, 2020). Based on GBD 2019, this study aimed to quantify the burden of ASD at the global, regional and national levels and provided a theoretical basis for the formulation of ASD supports and services tailored to different characteristics.
Methods
Data source
In compliance with the conditions of GBD data usage, data for the disease burden of ASD from 1990 to 2019 were exacted with the online Global Health Data Exchange (GHDx) query tool from the Institute for Health Metrics and Evaluation (http://ghdx.healthdata.org/gbd-results-tool). The analytical framework for the GBD 2019 and estimation methods of ASD burden have been delineated in previous studies (Baxter et al., Reference Baxter, Brugha, Erskine, Scheurer, Vos and Scott2015; GBD 2019 Diseases and Injuries Collaborators, 2020). Every step of this research adhered to the Guidelines for Accurate and Transparent Health Estimates Reporting (Stevens et al., Reference Stevens, Alkema, Black, Boerma, Collins, Ezzati, Grove, Hogan, Hogan, Horton, Lawn, Marušić, Mathers, Murray, Rudan, Salomon, Simpson, Vos and Welch2016). ASD definition was based on the clinical threshold as established by the Diagnostic and Statistical Manual of Mental Disorders (DSM), the International Classification of Disease criteria (ICD), the Chinese Classification of Mental Disorders (CCMD) or diagnosed by a clinician using established tools. The ASD in the GBD study covered five sub-disorders based on DSM-IV-TR: autistic disorder (299.00), pervasive developmental disorder, pervasive developmental disorder not otherwise specified (299.80), Rett's disorder (299.8), Asperger's disorder (299.8) and childhood disintegrative disorder (299.10), and covered eight sub-disorders based on ICD10: childhood autism (F84.0), atypical autism (F84.1), Rett syndrome (F84.2), other childhood disintegrative disorder (F84.3), overactive disorder associated with mental retardation and stereotyped movements (F84.4), Asperger syndrome (F84.5), other pervasive developmental disorders (F84.8) and pervasive disorder unspecified (F84.9). The systematic collection of epidemiological ASD burden was conducted by GBD 2019 in three stages involving electronic searches of the peer-reviewed literature in PsycInfo, Embase and PubMed databases; the grey literature; expert consultation to report estimates of prevalence, incidence, remission and excess mortality for ASD. According to GBD inclusion criteria, a total of 167 original data sources of ASD were given for morbidity modelling by parameter. The extracted data underwent three types of age and sex splitting processes, including available presentation, splitting by MR-BRT analysis (a Meta-Regression with Bayesian priors, Regularisation, and Trimming analysis), and assessing by DisMod-MR 2.1 (disease model-Bayesian meta-regression 2.1, a Bayesian meta-regression modelling tool) (GBD 2019 Diseases and Injuries Collaborators, 2020). Estimates of ASD with known biases were adjusted or crosswalked accordingly prior to DisMod-MR 2.1. DisMod-MR 2.1 synthesises epidemiological data for ASD outcomes from disparate settings and sources, adjusting for different case definitions or diagnostic criteria and sampling methods to generate internally consistent estimates of prevalence, incidence, remission and mortality by location, year, age group and sex (India State-Level Disease Burden Initiative Mental Disorders Collaborators, 2020). All computations in GBD were done 1000 times, each time drawing from the distribution of the sampling error of data inputs, the uncertainty of data corrections for measurement errors, the uncertainty in coefficients from model fit and the uncertainty of severity distributions and disability weights (Global Research on Developmental Disabilities Collaborators, 2018). To describe the disease burden of ASD in different geographic units, the 204 countries and territories were separated into 21 GBD regions according to a geographic hierarchy, such as high-income Asia Pacific, Central Latin America and Central Europe, which were also simplified into seven super GBD regions, such as high-income regions. In addition, the 204 countries and territories were further classified into five regions in terms of their corresponding SDI in 2019 (socio-demographic index, a composite indicator of a country's lag-distributed income per capita, average years of schooling and the total fertility rate in females under the age of 25 years), namely, low, low-middle, middle, high-middle and high SDI regions (GBD 2019 Demographics Collaborators, 2020; GBD 2019 Diseases and Injuries Collaborators, 2020).
Statistical analysis
Based on the GBD global reference population, we applied the age-standardised incidence rate (ASIR), age-standardised prevalence rate (ASPR) and age-standardised disability-adjusted life years (DALYs) rate (ASDR) to quantify the ASD burden by location, sex and SDI from 1990 to 2019 for eliminating the effect of age composition in comparisons. DALYs represent the sum of years of life lost prematurely and years lived with disability. The 95% uncertainty intervals (UIs) for every metric in the GBD study were produced based on the 25th and 975th ordered values of 1000 random draws of the posterior distribution (GBD 2016 Neurology Collaborators, 2019). We further used the average annual percentage change (AAPC) to describe the temporal trend in various age-standardised rates (ASRs) of ASD burden from 1990 to 2019. We performed a regression model fitting the natural logarithm of the ASR with the calendar year, namely, ln (ASR) = α + β* calendar year + ɛ, to estimate the AAPC with its 95% confidence interval (CI) based on the formula of 100 × (exp (β) − 1) (Yang et al., Reference Yang, Quam, Zhang and Sang2021b, Reference Yang, Zhang, Zhang, Chu and Sang2022). Additionally, to explore the influential factors for AAPCs in ASD, we evaluated the correlation between AAPCs and baseline burden in 1990 as well as SDI in 2019 using the Spearman rank correlation test at the national level. The ASRs of ASD in 1990 could serve as the disease burden at baseline, and the SDI in 2019 is a composite indicator to reflect the availability and level of health care in different countries or regions (Yang et al., Reference Yang, Fang, Chen, Zhang, Yin, Man, Yang and Lu2021a, Reference Yang, Zhang, Zhang, Sang, Chen and Zuo2021c). All statistical analyses in this study were performed using R program version 4.0.3 (https://www.R-project.org/). A two-sided p value of <0.05 was considered statistically significant.
Results
Global burden and temporal trend in ASD
In 2019, there were 60.38 × 104 (95% UI 50.17–72.01) newly-diagnosed ASD patients worldwide, compared with 60.29 × 104 (95% UI 50.14–71.83) in 1990. The ASIR per 100 000 population increased slightly from 9.17 (95% UI 7.62–10.92) in 1990 to 9.32 (95% UI 7.75–11.12) in 2019, with the AAPC of 0.06 (95% CI 0.04–0.07) (Table 1). Besides, the accumulated number of ASD patients increased from 203.36 × 105 (95% UI 168.57–242.23) in 1990 to 283.25 × 105 (95% UI 235.01–338.11) in 2019 globally, with a relatively stable ASPR of about 370 (95% UI 305.95–441.19) cases per 100 000 population over the past 30 years (online Supplementary Table S1). Similarly, there were 43.07 × 105 (95% UI 28.22–62.32) DALYs worldwide attributable to ASD in 2019, showing an increase of 38.67% since 1990 (31.06 × 105; 95% UI 20.25–45.14), and kept a relatively stable ASDR with around 56 (95% UI 36.82–81.52) per 100 000 population during the period (online Supplementary Table S2).
Table 1. Incidence and age-standardised incidence rate per 100 000 people for autism spectrum disorder in 1990 and 2019, and its average annual percentage change from 1990 to 2019

No., number; ASIR, age-standardised incidence rate; UI, uncertainty interval; AAPC, average annual percentage change; CI, confidential interval.
Variation in ASD burden at regional and national level
In 2019, the ASRs of incidence, prevalence and DALYs in ASD were all highest in high SDI regions, followed by high-middle SDI regions, and lowest in low-middle SDI regions and middle SDI regions. The ASIR significantly increased in high SDI regions from 1990 to 2019 (AAPC = 0.36, 95% CI 0.31–0.41), while remained stable in other SDI regions (Table 1). Moreover, the ASPR and ASDR both slightly increased in all SDI regions, especially in high regions (online Supplementary Tables S1 and S2).
Among the 21 GBD regions, high-income North America, high-income Asia Pacific and Western Europe were the three regions with the highest ASIR of ASD in 2019, from 14.18 to 16.41 per 100 000 population. However, South Asia, Oceania, and North Africa and Middle East were the three regions with the least ASIR, from 7.6 to7.73 per 100 000 population (Table 1). Alarmingly, high-income North America not only showed the highest ASIR in 2019, but also showed the largest increase in ASIR from 1990 to 2019 (AAPC = 0.80, 95% CI 0.67–0.93). The distributions of ASPR and ASDR in different GBD regions were similar to the distribution of ASIR (online Supplementary Tables S1 and S2).
The ASIR of ASD varied more than three times across 204 countries and territories in 2019, ranging from Taiwan (5.44/100 000) to Andorra (18.56/100 000). The ASD-related ASIR exceeded 13 per 100 000 in 25 countries, such as Andorra, the UK, Sweden, Japan and USA (Fig. 2, online Supplementary Table S3). Conversely, the ASIR in 2019 was lower than 7.5 per 100 000 in Taiwan, Samoa, Democratic People's Republic of Korea and other 16 countries (Fig. 2, online Supplementary Table S4). The geographic distribution of ASPR and ASDR for ASD in 2019 was highly consistent with the distribution of ASIR (Fig. 2, online Supplementary Fig. S1). Besides, the countries with the largest populations, including China, India and USA, had the most incident cases, prevalent cases and DALYs in 2019 (online Supplementary Fig. S1).
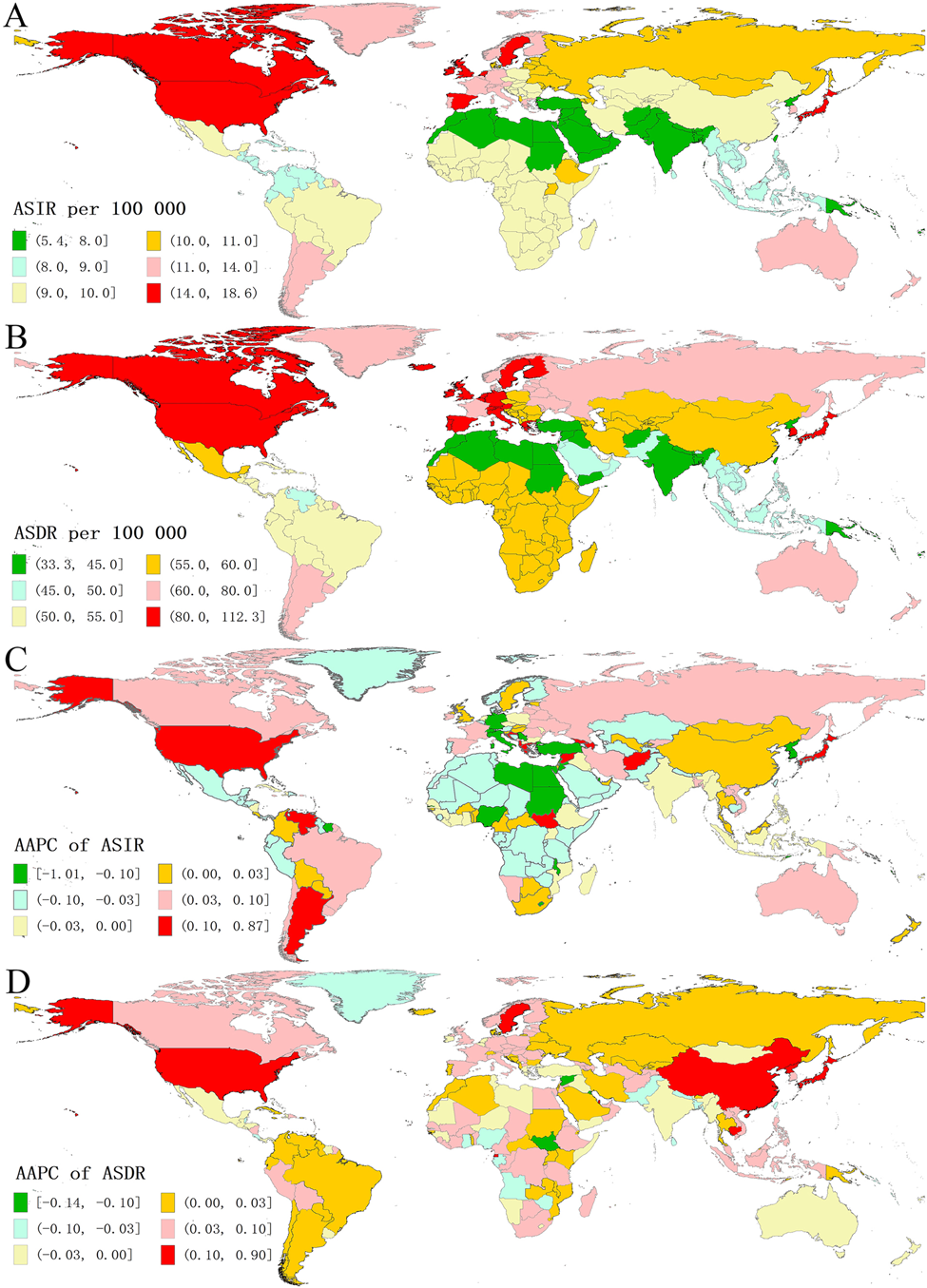
Fig. 1 The global disease burden of autism spectrum disorder in 204 countries and territories. (A) ASIR in 2019; (B) ASDR in 2019; (C) AAPC of ASIR from 1990 to 2019; (D) AAPC of ASDR from 1990 to 2019. ASIR, age-standardized incidence rate; ASDR, age-standardized DALYs rate; AAPC, average annual percentage change.
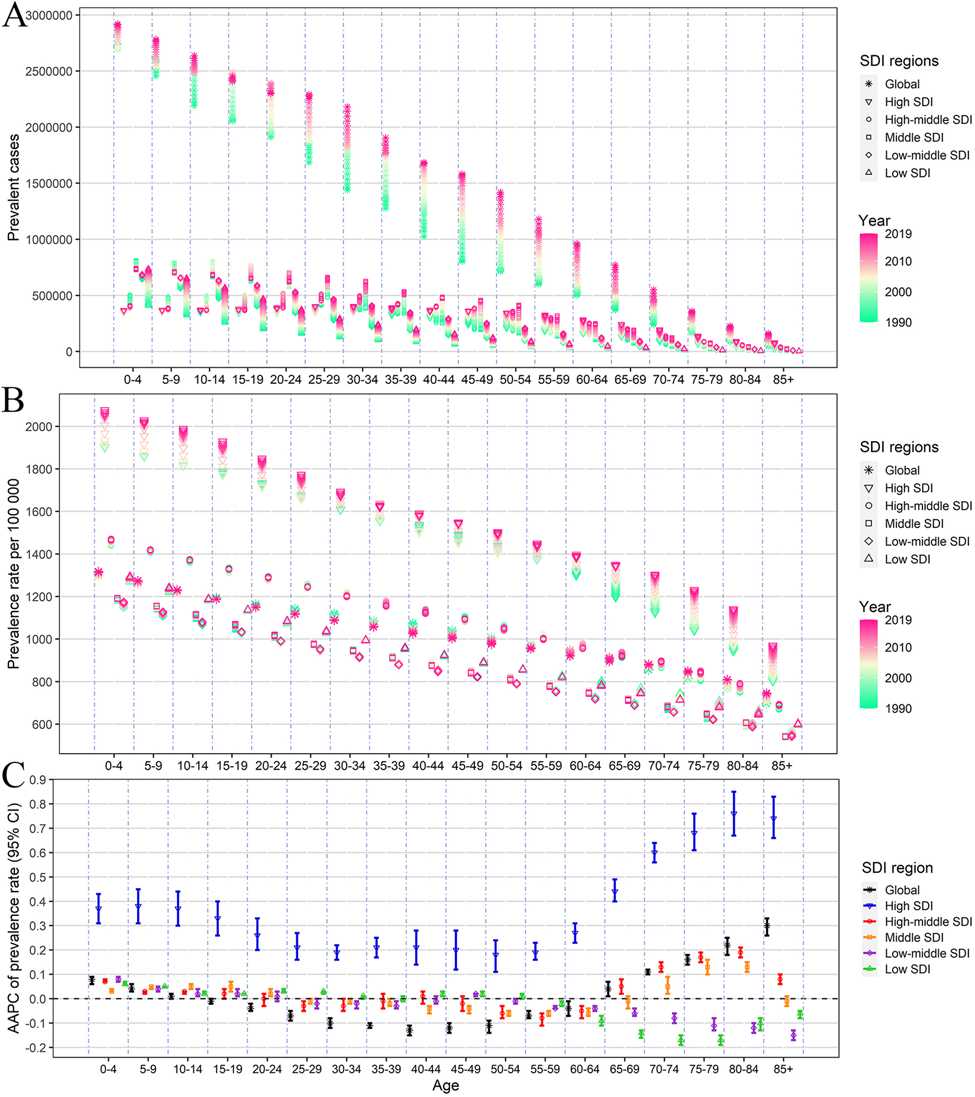
Fig. 2 The annual burden and its change of autism spectrum disorder by different age groups, and SDI regions, from 1990 to 2019. (A) prevalent cases; (B) prevalence rate; (C) AAPC of prevalence rate. SDI, sociodemographic index; AAPC, average annual percentage change.
From 1990 to 2019, the largest annualised growth rate of ASRs was all observed in the USA (AAPC of ASIR = 0.87; AAPC of ASPR = 0.91; AAPC of ASDR = 0.90), and the AAPC of ASIR exceeding 0.10 was found in other 16 countries and territories, such as Andorra, Syria, Japan and Albania (Fig. 2, online Supplementary Fig. S1 and Table S5). Moreover, the AAPC of ASPR exceeding 0.1 was observed in other 12 countries and territories, such as Qatar, Maldives, Equatorial Guinea, Japan, where the AAPC of ASDR also exceeded 0.1 (Fig. 2, online Supplementary Fig. S1 and Table S6). Overall, in most countries, the absolute value of AAPC is less than 0.1, which indicates that the burden of ASD in these countries has remained relatively stable.
Variation in ASD burden by sex and age
In 2019, the ASRs for ASD in males were about three times those in females, despite that the gender disparity in ASRs was narrowed slightly over the past 30 years because the increasing trend was pronounced among females (Table 1, online Supplementary Tables S1 and S2). Regarding the age groups, the prevalent cases and DALYs were both highest in the youngest age groups, and decreased with age (Fig. 3a and online Supplementary Fig. S2A). Besides, prevalent cases significantly increased in all age groups over the past 30 years at the global level, especially among 25–55 years old age groups (Fig. 3a). From 1990 to 2019, the prevalence rate due to ASD was highest in the high SDI regions, which showed an upward trend in all age-specific groups especially among the population aged over 65 years. For other SDI regions, the prevalence rate kept relatively stable in almost all age-specific groups. However, among the population aged over 65 years, the prevalence rate presented increasing trends globally, especially in the higher SDI regions (Fig. 3b and c). A similar distribution of age-specific DALYs and DALYs rates was observed during the same period (online Supplementary Fig. S2).

Fig. 3 The factors affecting the change of age-standardized incidence rate of autism spectrum disorder from 1990 to 2019. (A) ASIR in 1990 and AAPC of ASIR at the national level; (B) SDI in 2019 and AAPC of ASIR at the national level; (C) Annual change in ASIR along with the SDI across 21 GBD regions from 1990 to 2019. The blue line was an adaptive association fitted with Loess regression based on all data points. The ρ indices and P values were derived using Spearman rank analysis. ASIR, age-standardized incidence rate; AAPC, average annual percentage change; SDI, socio-demographic index; GBD, Global Burden of Disease Study.
The influential factors for AAPC
We analysed the relationship between the initial burden of ASIR, ASPR and ASDR in 1990 and AAPC values in 204 countries or territories (Fig. 1, online Supplementary Figs S3 and S4). There was a weak positive association between the AAPC of ASDR and initial ASDR in 1990 at the national level (ρ = 0.15, p = 0.0379). Moreover, we found that the AAPC in ASIR and ASPR were both positively associated with SDI in 2019 (ρ = 0.15, p = 0.0344; ρ = 0.21, p = 0.0028). Figure 1c presented the relationship between ASIR of ASD and SDI over time in 21 GBD regions, expressed in the annual time series from 1990 to 2019. The ASIR in most GBD regions remained relatively stable over time, but high-income North America, high-income Asia Pacific, Southern Latin America, Australasia presented an obvious climbing trend. Similar changing trends of ASPR and ASDR with SDI in 21 GBD regions were found in online Supplementary Figs S3C and S4C.
Discussion
Based on the GBD 2019, this study showed the most up-to-date patterns and trends of the worldwide burden estimates associated with ASD from 1990 to 2019 at the global, regional and national levels. Our analysis revealed that there was a slight upward trend of ASIR for ASD, whereas the ASPR and ASDR both showed relatively stable trends over the past 30 years globally. Although changes in global ASIR (1.6% growth) were less prominent, high SDI regions such as high-income North America and high-income Asia Pacific have displayed larger increases. Globally, the increase of DALYs is largely due to the changing age patterns and accumulating cases in older age. But taking into account population changes and age composition, the ASDR remain stable from 1990 to 2019. Of note, among the population aged over 65 years, the ASPR and ASDR both presented increasing trends globally, especially in the higher SDI regions. These data confirm that the burden of ASD in some regions and populations is undergoing significant change and that ASD is becoming an even greater public health concern.
The estimates of ASD burden varied somewhat across world regions and countries (Baxter et al., Reference Baxter, Brugha, Erskine, Scheurer, Vos and Scott2015). Our current results presented that the ASIR of ASD varied more than three times across 204 countries and territories in 2019. Previous studies have presented that the prevalence of ASD in developed countries is significantly higher than the global prevalence (Elsabbagh et al., Reference Elsabbagh, Divan, Koh, Kim, Kauchali, Marcín, Montiel-Nava, Patel, Paula, Wang, Yasamy and Fombonne2012; Lyall et al., Reference Lyall, Croen, Daniels, Fallin, Ladd-Acosta, Lee, Park, Snyder, Schendel, Volk, Windham and Newschaffer2017), and lower rates are reported in resource-limited countries, where epidemiological data are more difficult to collect (Tomlinson et al., Reference Tomlinson, Yasamy, Emerson, Officer, Richler and Saxena2014). Similarly, our data showed that the greatest burden fell on high SDI regions, such as high-income Asia Pacific, high-income North America, Western Europe and Australasia. Besides, the high SDI regions also showed the largest increasing trends in the ASRs from 1990 to 2019. A possible explanation is that in high SDI regions, much of the increase may be attributed to detailed information records and diagnostic creep (the process of gradually broadening the definitions of a certain disorder) (Lyall et al., Reference Lyall, Croen, Daniels, Fallin, Ladd-Acosta, Lee, Park, Snyder, Schendel, Volk, Windham and Newschaffer2017; Fabiano and Haslam, Reference Fabiano and Haslam2020). However, the additional influence of other non-etiologic factors (such as specific screening, diagnostic criteria, public awareness and availability of services), as well as etiologic factors (including genetic and environmental risk factors) cannot be ruled out (Xu et al., Reference Xu, Strathearn, Liu and Bao2018; Hyman et al., Reference Hyman, Levy and Myers2020). A population-based study showed that an increased risk of autism presenting with comorbid intellectual disability has actually been found among children of migrants from these regions in high-income countries (Magnusson et al., Reference Magnusson, Rai, Goodman, Lundberg, Idring, Svensson, Koupil, Serlachius and Dalman2012). It is worth noting that the ASIR of ASD in some Western European Countries, especially in Germany, Italy and Switzerland, showed a slight downward trend from 1990 to 2019, which may be related to the serious problem of ageing and lower birth rates, and further research is needed. Nonetheless, the burden of ASD in most regions and countries has remained relatively stable, which may be related to the under-identification of autistic children caused by limited ASD awareness and diagnostic services (Sun et al., Reference Sun, Allison, Wei, Matthews, Auyeung, Wu, Griffiths, Zhang, Baron-Cohen and Brayne2019). A large percentage (up to 75%) of ASD patients display co-morbid psychiatric or neurological disorders, which may complicate the accurate diagnosis of ASD (Sharma et al., Reference Sharma, Gonda and Tarazi2018), and may be confused with other mental health disorders due to crossover symptoms (Fusar-Poli et al., Reference Fusar-Poli, Brondino, Politi and Aguglia2022). Moreover, the misunderstandings and stigmatisation of ASD highlight disparities in ASD diagnosis, education and service provision (Yu et al., Reference Yu, Stronach and Harrison2020). The potential impact of culturally specific social cognitive processing styles on the burden of ASD remains uncertain and requires further investigation (de Leeuw et al., Reference de Leeuw, Happé and Hoekstra2020).
Our research found that ASD burden was significantly higher in males than in females, with the ratio of men to women in terms of incidence, prevalence and DALYs being about 3:1, which is consistent with the GBD 2010 estimates (Baxter et al., Reference Baxter, Brugha, Erskine, Scheurer, Vos and Scott2015). The gender differences in the burden of ASD showed a slight shrinking trend because the increasing trend was pronounced among females. The predominance of males with ASD is a well-recognised feature of the disease (Fombonne et al., Reference Fombonne, MacFarlane and Salem2021). However, to a large extent, the origin of sex differences is not well understood. Accruing evidence suggested that autistic female individuals might be underdiagnosed owing to a different presentation of ASD symptoms, higher rates of internalising difficulties and higher rates of camouflaging (Halladay et al., Reference Halladay, Bishop, Constantino, Daniels, Koenig, Palmer, Messinger, Pelphrey, Sanders, Singer, Taylor and Szatmari2015; Weir et al., Reference Weir, Allison and Baron-Cohen2021). Camouflaging, defined as strategies used to appear less autistic in social interactions, is argued to be a key feature of the female autistic phenotype (Wood-Downie et al., Reference Wood-Downie, Wong, Kovshoff, Mandy, Hull and Hadwin2021); however, this behaviour can come at serious personal cost, worsening mental health problems and even increasing risk of suicidality (Hull et al., Reference Hull, Petrides, Allison, Smith, Baron-Cohen, Lai and Mandy2017; Cassidy et al., Reference Cassidy, Bradley, Shaw and Baron-Cohen2018). It is, therefore, necessary to accurately diagnose and identify females with autism-like features, and provide specialised support for females whose impairments may be under-recognised traditionally.
Our results present the prevalent cases and the prevalence rates of ASD gradually decreased with age, with the peak in the age group of 0–4 years. ASD symptoms are typically present at the age of 3 years, although symptoms may not fully manifest until school age or later (Lyall et al., Reference Lyall, Croen, Daniels, Fallin, Ladd-Acosta, Lee, Park, Snyder, Schendel, Volk, Windham and Newschaffer2017). This age-related difference may be related to the fact that the person with the most obvious ASD symptoms has already been diagnosed at an early stage (Happé et al., Reference Happé, Mansour, Barrett, Brown, Abbott and Charlton2016). However, patients with milder forms of ASD may not be diagnosed until they reach adulthood (Alpert, Reference Alpert2021). Interestingly, we observed that from 1990 to 2019, the number of prevalent cases around the world showed an increasing trend in all age groups, especially in the 25–55 age group. The growing awareness of ASD among the general population, parents and mental health professionals has significantly contributed to this rise in diagnoses (Zablotsky et al., Reference Zablotsky, Black, Maenner, Schieve, Danielson, Bitsko, Blumberg, Kogan and Boyle2019); however, part of the growing number of cases of ASD could be attributed to the identification of the so-called ‘lost generation’, who has started to seek a first formal diagnosis after the release of the DSM-5 (Lai and Baron-Cohen, Reference Lai and Baron-Cohen2015). It is worth noting that the prevalence rate of ASD showed a significant upward trend globally among the elderly over 65 years old, especially in high, high-middle SDI regions. Due to the ageing population, the number of elderly people with ASD may increase in the near future. Therefore, it is also a very meaningful work to further study the phenotype and diagnosis of ASD in the elderly (van Niekerk et al., Reference van Niekerk, Groen, Vissers, van Driel-de Jong, Kan and Oude Voshaar2011).
The aetiology of ASD is extremely complex and uncertain (Emberti Gialloreti et al., Reference Emberti Gialloreti, Mazzone, Benvenuto, Fasano, Alcon A, Kraneveld, Moavero, Raz, Riccio, Siracusano, Zachor, Marini and Curatolo2019). A number of epidemiological studies have found positive associations between socioeconomic status and the prevalence of ASD (Durkin et al., Reference Durkin, Maenner, Baio, Christensen, Daniels, Fitzgerald, Imm, Lee, Schieve, Van Naarden Braun, Wingate and Yeargin-Allsopp2017). In our study, we further discussed the relationship between the AAPCs in ASD burden and SDI in 2019 and baseline burden in 1990, which has not been previously reported. Our results showed that the annualised increasing trend of ASPR due to ASD was associated with the increasing SDI, which indicated that countries with higher SDI have experienced a more rapid increase in ASPR of ASD from 1990 to 2019. Possible reasons involve better access to health care resources and educational services, universal screening, effective surveillance system, lowered stigma and other environmental or biological basis (Becker, Reference Becker2018; Yu et al., Reference Yu, Lien, Liang and Kuo2021). In addition, we found that there was a weak positive association between the AAPC of ASDR and initial ASDR in 1990 at the national level, which could be explained by the fact that ASD has not received enough attention in the field of global public health (Baxter et al., Reference Baxter, Brugha, Erskine, Scheurer, Vos and Scott2015). It may be of great significance to make extensive use of family, community and school resources to involve more patients and related personnel, and formulate appropriate early prevention and intervention measures (Jones et al., Reference Jones, Akram, Gordon, Murphy and Sharkie2021).
Although GBD collaborators have improved on the data and methods used to estimate the burden of mental disorders based on all available data sources, there are still several limitations that need to be noted. First, the GBD estimation of ASD is reconstructed by mathematical models based on the limited availability and quality of sources, which may deviate from the actual data to a certain extent, especially in older people and some underdeveloped regions with extremely scarce prior information (GBD 2019 Diseases and Injuries Collaborators, 2020). Second, due to the higher probability of undiagnosed and untreated ASD in developing countries, the burden of ASD may be underestimated to a certain extent. Third, the GBD data were collected from various databases and institutions with different defined disorder categories and diagnostic methods, which might have caused heterogeneity in the data and influenced the consistency of burden estimation. Fourth, co-occurring conditions are common in children and adults with ASD, but the GBD study does not include the specific harm of ASD-related comorbidities in the estimate of ASD burden. Finally, this study lacks an estimate of the risk factors leading to the burden of ASD. Hopefully, future research will focus on this aspect.
The global burden of ASD is substantial and continues to increase, despite differences in gender, age, geographic location and socioeconomic status over the past three decades. Based on the specific characteristics of ASD burden across the world, public health officials and policy makers can formulate more detailed prevention and intervention strategies, such as developmental surveillance, autism-specific screening, social support systems, greater acceptance and inclusion, and communication and education interventions, especially for high-income countries, children and male populations. This research emphasises the global importance of ASD, and it is essential for effective policy making on a global scale.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796022000178
Data
The data that support the findings of this study are openly available at http://ghdx.healthdata.org/gbd-results-tool, an open-source online data repository hosted at the Institute for Health Metrics and Evaluation (IHME).
Acknowledgements
We would also like to thank the countless individuals who have contributed to the Global Burden of Disease Study 2019 in various capacities.
Author contributions
Study design: X. R. Y., M. L.; data collection: Z. L., L. J. Y., H. C., Y. F., T. C. Z., X. L. Y., J. Y. M.; data analyses: Z. L., L. J. Y.; results visualisation: Z. L., L. J. Y., H. C., Y. F., T. C. Z., X. L. Y., J. Y. M.; results interpretations: all authors; manuscript writing: Z. L., L. J. Y.; manuscript revising: X. R. Y., M. L.
Financial support
This work was supported by the National Key Research and Development Program of China (grant number: 2021YFF1201101), the National Natural Science Foundation of China (grant numbers: 82103912, 82173591 and 81973116), the China Postdoctoral Science Foundation (grant number: 2021M700080), and the Shandong Provincial Natural Science Foundation (grant number: ZR2020QH302). The funders were not involved in the collection, analysis or interpretation of the data, or the writing or submitting of this report.
Conflict of interest
None.
Ethical standards
The GBD 2019 study is a publicly available database and all data were anonymous. Our study protocol was approved by the Institutional Review Boards of Qilu Hospital of Shandong University with approval number KYLL-202011(KS)-239.








