INTRODUCTION
We use the term telemedicine to encompass the use of telecommunications technology (including the transmission of video, still images, radiological studies, physiological data, and pathology results) to provide health care services to a patient. Typically, these patients are at a distance from the provider. Telemedicine has been used for many years to close geographical and resource-related gaps in health care services. Since the 1960s, forays into providing health care through telemedicine have been of interest to providers and have aimed to provide more timely and convenient care to patients in rural or remote settings who do not have the same access to specialist care.
Initial attempts to introduce telemedicine systems in the 1960s and 1970s were limited by the costs and limitations of the technology.Reference Murphy and Bird 1 - Reference Fuchs 3 Early telemedicine programs were externally funded with the intention of producing self-sustaining telemedicine networks. The cost of these programs, with the technology available at the time, made this goal difficult to achieve, so the burgeoning interest in telemedicine as the new frontier in medicine waned.Reference Perednia, Allen and DA 4 , Reference Grigsby 5
With increasing centralization of specialized care and expectations of equal access, regions with dispersed populations have looked for options for bringing expertise to the remote bedside. As technology has advanced in quality and dropped in cost, telemedicine has made a resurgence and is gaining acceptance as a modality to decrease transfers between hospitals, shorten the time between first medical contact and therapy, and improve the quality of care.
Current applications for telemedicine span the breadth of practice and include stroke evaluation and care, psychiatric evaluations, surgical consultations, and multidisciplinary trauma care.Reference Ward, Jaana and Natafgi 6 - Reference Roots, Bhalla and Birns 10 Innovative applications are being introduced on an increasingly frequent basis and include tele-mentoring of ultrasound examinations, videophone instructions from 9-1-1 dispatchers to layperson rescuers, and disaster response approaches.Reference Dyer, Cusden and Turner 11 - Reference Llewellyn 14 An application that is gaining momentum and may improve emergency care in rural centres is the use of telemedicine in the emergency department (ED).
Telemedicine stands to offer much in the way of decision support and critical care advice to rural emergency physicians.Reference Macht, MacKenzie and Ginde 15 - Reference Henderson, Isom and Summers 17 Patients presenting to an ED are often medically undifferentiated that creates certain challenges for the practitioner responsible for their care, especially in resource-poor environments. n small centres where only one physician is working at a time with no direct consultant support, a second pair of eyes in the form of a telemedicine physician could be a pivotal and important support to improve recruitment efforts for rural communities.Reference Leap 16 The acutely ill or traumatized patient may be quite complex and may benefit from consultation with a physician with more experience or specific training.
The purpose of this paper was to collect and summarize the currently available literature on the use of real-time video-based technologies to support the management of patients presenting to EDs.
METHODS
The format of a scoping review (as described by Arksey et al.Reference Arksey and O’Malley 18 in 2005) was selected for this project with the aim to evaluate the breadth and variety of research activity being conducted in ED-based telemedicine and to identify gaps that may currently exist. As this is a relatively new area of study and the applications are potentially significant for many avenues of emergency medicine, a scoping review format was thought to be the best way to identify specific questions or knowledge gaps for future study.
Data sources and searches
The search strategy was developed with the assistance of a librarian at our university health sciences library. We searched Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, the Cochrane Database, Database of Abstracts of Reviews of Effects (DARE), and PubMed for all publications since the earliest date available in each database (date of search February 15, 2016) using the search terms “telemedicine AND (emergency medicine OR emergency medical service OR remote consultation OR emergency service, hospital OR rural health OR hospital rural).” The results were restricted to studies in humans and the English language. We also reviewed the references in the reviews that were located in the search to identify other potentially relevant records.
Study selection
Two authors (DK and DH) screened the search results in a reference manager software and excluded publications not relevant to the scope of this project based on title and a review of the abstracts. If the articles could not be satisfactorily excluded based on information available in the title, abstract, or both, the full text was obtained for clarification. Disagreement was resolved by inclusion of the article for an in-depth review.
Publications meeting the following criteria were included: 1) full-text articles; 2) articles addressing the use of telemedicine to support patient care in pre-hospital or ED settings; and 3) clinically focused articles in which applications of telemedicine were employed on patients, not in simulation studies or mathematical modelling studies. Exclusion criteria were: 1) letters/opinion pieces and review articles (although review articles were used to find other relevant articles for inclusion); 2) methods of implementation that were not video-based, including the sharing of still images, ultrasound images, and audio-only modalities; 3) telemedicine used solely for a single subspecialty or specific emergency medicine presentation (for example, telemedicine systems specifically and exclusively used for cerebral vascular attack [CVA]/stroke evaluation, trauma, acute burn injuries, psychiatry, non-routine disaster response, or pre-hospital mentoring of non-health-care-trained providers); and 4) telemedicine use in chronic care patients.
Final selection of studies for inclusion was made by consensus (Figure 1 outlines the process of selection and exclusion). The included articles were grouped into categories based upon how telemedicine was being used to enhance emergency patient care and are summarized below and in Table 1.
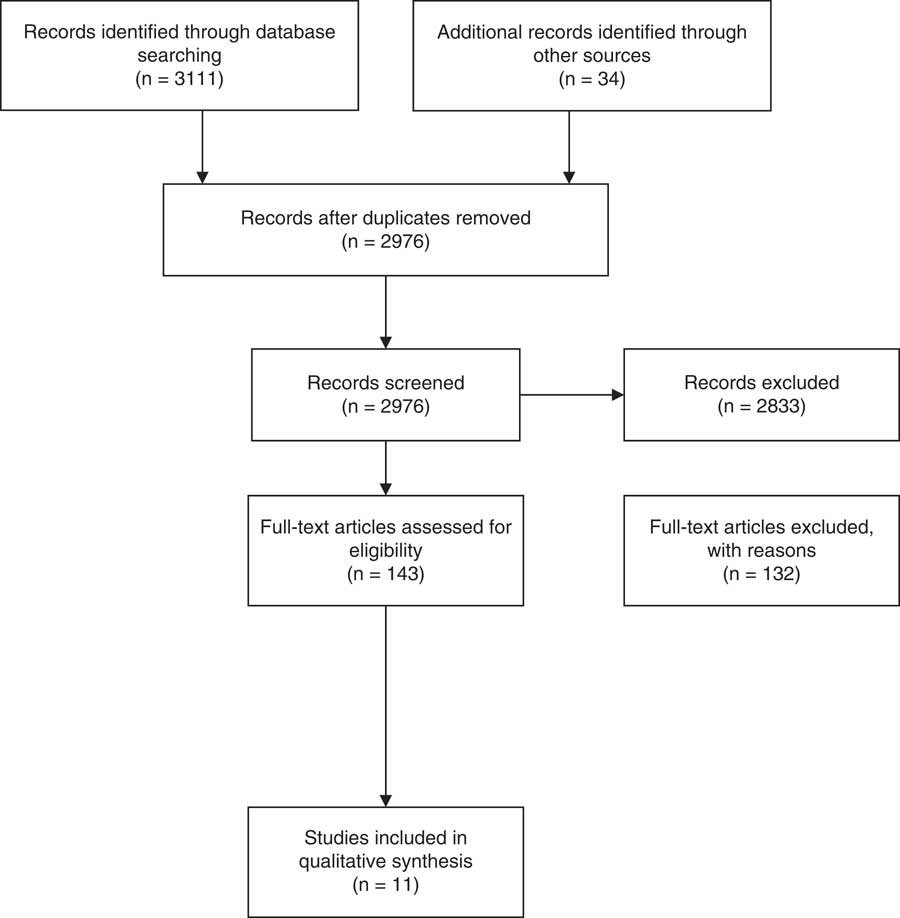
Figure 1 Study Selection Flow Diagram
Table 1 Summary of selected studies
ED=emergency department; ICU=intensive care unit.
RESULTS
Summary
For the purpose of this review, Table 1 was used to summarize the selected studies briefly. In this review, we found that the evidence available regarding the use of telemedicine systems is, for the most part, limited to qualitative outcomes such as patient or physician satisfaction. If quantitative measures have been used, treatment outcomes such as time to treatment or transfer and proportion of patients transferred have been proposed as potential markers regarding the utility of this method of support for rural providers. Attempts to gather evidence of improved patient outcomes following the implementation of a telemedicine system is currently lacking and would add strength to the arguments for using this technology. The currently available evidence that is summarized in more detail in this article indicates that there is potential for the use of this technology to treat injuries ranging from minor musculoskeletal injuries to acute life-threatening cardiovascular disease processes. Beyond directing management, the evidence suggests that this technology may assist both with decision-making regarding transfer between hospitals and with the effectiveness of the transfer itself by facilitating communication between teams of providers.
Minor treatment applications for telemedicine in the ED
Telemedicine is being increasingly seen as a way to provide physician expertise to remote or rural hospitals that would not otherwise have the benefit of this level of care.Reference Henderson, Isom and Summers 17 , Reference Craig and Patterson 19 In many of these minor treatment-type centres, nursing staff and technicians had previously provided the majority of care with minimal access to physician support. In theory, with access to this service, more comprehensive care could be provided by physicians at a distance, as either a second opinion or the primary care provider.
The first study to look at this construct was a randomized controlled trial performed by Brennan et al.Reference Brennan, Kealy and Gerardi 20 in 1999 in two hospitals in New Jersey. This study randomized patients with minor complaints (from a preselected list of 15 complaints that they felt could be managed remotely, such as abrasions, bronchitis, minor burns, otitis media, and wound checks) for evaluation either by a telemedicine doctor or through an “in-person” physician assessment.Reference Brennan, Kealy and Gerardi 20 Physicians at the centre took turns providing both services and completed post-encounter surveys, as did patients and nursing staff. This service was well received in general, and there were no differences in the outcomes (return to the ED within three days or need for further treatment). Patients who had telemedicine treatment rated their experience better than their last conventional ED visit.
A group in Scotland implemented a system of minor treatment telemedicine, starting with 10 sites in 2000 and expanding to 14 sites in 2004.Reference Brebner, Brebner, Ruddick-Bracken and Wootton 21 - Reference Brebner, Brebner and Ruddick-Bracken 23 Their system connected rural physicians and nurses with academic emergency specialists in Aberdeen to discuss patients and share information. In their analyses of this system, they noted that the consults were frequently brief, averaging 10 minutes in duration and usually involving requests for interpretation of radiographs. A more recent evaluation of the same system focused on longitudinal data from one peripheral site to detect differences in management that occurred as users became more accustomed to the telemedicine system.Reference Ferguson, Rowlands and Palombo 24 They noted that transfer rates from the peripheral hospital to the academic centre decreased from 31% to 23% over the course of the study that was postulated to represent increasing confidence in the hub doctor’s ability to care for patients at a distance.
Telemedicine for transfer triage
Telemedicine proponents maintain that telemedicine can serve as a method for avoiding the unnecessary transfer of ED patients from a rural location to a central academic hospital. A descriptive analysis of a system in North Carolina found that the transfer rate for teleconsults was 32%, which was significantly higher than the background rate of transfers (5%).Reference Stamford, Bickford, Hsiao and Mattern 25 However, after adjusting for the severity of the injury, it was projected that 30% of the possible transfers were averted by telemedicine consultation. Furthermore, in 24% of the teleradiologic consults and 52% of the tele-diagnostic consults, treatment was changed using telemedicine, either through the revision of diagnosis or by suggestions from the consultant regarding alternative management options.
Telemedicine for management of acutely ill patients with life-threatening illnesses
With the utility of telemedicine reasonably well established for the management of minor injuries, interest in the use of this technology for managing patients with life-threatening injuries began to grow. In 2008, a trial in New South Wales, Australia, instituted a system known as the Virtual Critical Care Unit (ViCCU) to connect clinicians in a smaller district ED with emergency medicine and intensive care specialists from a larger academic hospital.Reference Westbrook, Coiera and Brear 26 They used this technology for patients who were designated as triage category 1 or certain categories of category 2 (emergent patients) and compared several patient outcomes before and after implementation of this system. This study concluded that while there were some significant changes in management patterns, there were no significant differences in patient outcomes for the patients treated using the ViCCU system. The proportion of patients able to be safely discharged home from the rural hospital increased with the ViCCU system. However, the median length of stay for patients admitted to either hospital did not change over the course of the study. There were no significant changes in treatment time for critical care or major trauma patients. Interestingly, the number of procedures performed on patients in the rural setting increased with the ViCCU system for critical care patients, but not for trauma patients. A free text feedback survey raised some concerns from consulting specialists about an increased workload and sense of responsibility, but both rural and specialist physicians reported that patient management was improved with the system and that there was better support available for the rural centre.
Telemedicine consultation is also being used to coordinate and facilitate management of patients requiring resuscitation prior to and during aeromedical retrieval in Australia.Reference Sharpe, Elcock, Aitken and Furyk 27 The patients in this study, presenting with cardiac or respiratory arrests, were managed using telemedicine until the arrival of the retrieval team. Of eight such cases managed over a 12-month period, telemedicine did not delay aeromedical retrieval in any case. In five of the eight cases, it was felt that higher-quality information was available to the academic centre and retrieval team that aided in the effective transfer of the patient. Most survey respondents thought that telemedicine improved the overall quality of care provided to the patient; however, this survey had a relatively low response rate, small sample size, and no objective measures of patient outcomes. Likewise, in the Upper Midwest of the United States, a user survey evaluating a telemedicine emergency service indicated overall satisfaction with the service, and interviewees reported a reduction in the number of transfers required and improved coordination of care between the transferring hospital and accepting centre.Reference Mueller, Potter, MacKinney and Ward 28
Telemedicine applications combining urgent teleconsultation with scheduled teleconsultation
The Dakota Telemedicine System began in 1995 and links a level 2 trauma centre with three rural hospitals and their associated clinics.Reference Lambrecht 29 They offered consultations with a number of specialties, 24% of which were for emergency physicians. They divided the emergency medicine consultations into triage categories ranging from immediate consultations for emergent patient management to scheduled consults. The average length of a teleconsultation was 3.5 minutes, and the majority of emergency medicine teleconsultations (96%) involved some form of radiographic interpretation. Based on surveys provided to the participating physicians, there was generally positive feedback about this system.
Another model for non-urgent telemedicine consults in the ED was implemented in Western Australia whereby a hybrid system of teleconsultation was created.Reference Herrington, Zardins and Hamilton 30 Requests for videoconferencing consults with the emergency medicine physician were made by phone if immediate help was required or by fax if there were non-urgent questions. Examples of cases managed with this system include resuscitation efforts and reductions of dislocated joints. Feedback regarding the program indicated that it allowed isolated medical staff, nurses, or general practitioners to provide more effective care and to avoid transfer of patients in some cases. Nurses expressed increased confidence in managing sick patients, but the study did not include any measures of patient outcome.
DISCUSSION
The 2010 Academic Emergency Medicine consensus conference made several recommendations regarding research priorities to improve the provision of integrated and regionalized emergency medicine. The Inter-hospital Communications and Transport workgroup published a list of top priority research questions and highlighted among them are multiple questions on the potential applications of telemedicine for improving patient distribution, patient transfers, and ultimately patient outcomes.Reference Rokos, Sanddal, Pancioli, Wolff and Gaieski 31 The aim of this scoping review was to identify and summarize the body of evidence briefly by examining the ways in which telemedicine is being used currently in an ED setting and in what situations it has been implemented to improve the quality of patient care.
Physicians staffing EDs in rural and remote areas often have less formal training than those who work in large urban environments.Reference Bhimani, Dickie, McLeod and Kim 32 - Reference Kocher, Sklar and Mehrotra 34 Paradoxically, these physicians work in an environment that offers them significantly less support if taking care of critically ill patients. While the application of telemedicine to connect ED physicians at a distance is still in its infancy, this review found a range of diverse models being implemented worldwide. The use of this technology to connect rural or remote emergency physicians with their counterparts and other specialists offers many exciting opportunities to improve patient care and ease patient transfers.
The areas of the world where this technology has already had the most uptake and perhaps offers the greatest immediate potential are in large rural and sparsely populated areas. Geographically large countries with low population densities, such as Australia and Canada, as well as the more sparsely populated regions of the United States, are already implementing ED telemedicine applications.Reference Brebner, Brebner and Ruddick-Bracken 23 , Reference Westbrook, Coiera and Brear 26 , Reference Sharpe, Elcock, Aitken and Furyk 27 , Reference Herrington, Zardins and Hamilton 30 The combined benefits of improved patient care and potential reductions in expensive patient transfers appear to be particularly attractive and offer incentive for significant investment in these systems.Reference Herrington, Zardins and Hamilton 30
The goals of the telemedicine systems that have been studied vary widely depending on the characteristics of the health care system in which they are implemented. Some regions are evaluating applications of telemedicine to assist with the recruitment and retention of physicians by providing support in stressful clinical situations. The ability to replace or supplement physicians by using less expensive providers such as nurses or paramedics with telemedicine support may facilitate access to care in rural and remote areas. In a similar vein, treating more complicated patients in peripheral hospitals with telemedicine support might serve to decrease the necessity of transfers between hospitals and could relieve the strain of overcrowding in tertiary care hospitals. Furthermore, depending on the funding model of the health care system, increased activity in these sites has the potential to provide added revenue and, in doing so, support the development of those peripheral hospitals and retention of health care dollars in local communities.Reference Hicks, Boles and Hudson 35
With these differing goals in mind, an important task for future researchers will be to identify meaningful but measurable outcomes. Patient outcomes are difficult to quantify in observational studies because in many cases, it would appear that the patients chosen for telemedicine are sicker than patients who do not receive a consultation.
The potential advantages of telemedicine support in the ED are theoretically strong, supported by the success of telestroke networks worldwide.Reference Audebert and Schwamm 36 - Reference Deshpande, Khoja, McKibbon, Rizo and Jadad 38 However, a number of articles in this review identified concerns. They include peripheral physician reluctance to use these systems because of the perceived vulnerability to criticism from academic physicians,Reference Sharpe, Elcock, Aitken and Furyk 27 loss of skills in rural physicians because of reliance on telemedicine,Reference Sharpe, Elcock, Aitken and Furyk 27 and increased anxiety for hub physicians (who may not be comfortable treating patients at a distance and have reported feeling a sense of loss of control over the situation while they are treating a patient remotely).Reference Mueller, Potter, MacKinney and Ward 28 There are concerns about underutilization for a variety of reasons. These include a lack of comfort or training with the technology, concerns about billing for a consulting academic physician, and questions about which specialists should be consulted in different situations.Reference Mueller, Potter, MacKinney and Ward 28
OPPORTUNITIES
Implementation of systems for solely one form of medical consultation (for example, systems for ophthalmologicalReference Blackwell, Kelly and Lenton 39 , Reference Kulshrestha, Lewis, Williams and Axford 40 or dermatologicalReference Eminović, de Keizer and Wyatt 41 , Reference Scheinfeld, Fisher, Genis and Long 42 consultation) has been met with some success in some parts of the world. However, while specialized telemedicine supports for emergency physicians certainly exist and function well in some respects, ultimately, the appeal of telemedicine appears to lie not in the extremely specialized applications it may afford, but in its ability to support the urgent care of undifferentiated patients, who would not otherwise receive the same quality of care in a reasonable timeframe. Rural and remote emergency physicians will require a telemedicine system that gives them access to emergency medicine experts. These specialists will best be able to address the range of patients and the undifferentiated nature of their conditions in these types of environments.
LIMITATIONS
The variation in technologies used, implementation strategies, and pre-existing health systems, as well as the lack of objective outcomes in the trials reviewed, makes it inappropriate to compare or make any conclusions about the effectiveness of ED telemedicine.
Clear delineation of the requirements of a telemedicine system for emergency physicians, the barriers to implementation and use, and evidence of improved patient outcomes are important areas for future research.
CONCLUSIONS
This review suggests that telemedicine support for ED physicians is an application with significant potential. The field is still in its infancy, and there is still significant variation in how the technology is being applied. Future research is needed to explore the technological requirements of implementing the system in various clinical environments, the characteristics of successful ED telemedicine systems, and the outcome measures that should be used in studying this advancing technology.
Competing interests: The funding for this project came from a summer studentship grant from the Kingston Resuscitation Institute. The authors have no conflicts of interest.






