CASE REPORT
A 64-year-old female presented to the emergency department (ED) with a three-day history of worsening left eye floaters. The floaters had evolved from involvement of a small area of her central vision to the entire visual field of her left eye. She had associated eye irritation. There was no history of flashing lights, visual field loss, discharge, redness, diplopia, or headache. She denied any history of trauma. She had occasional floaters starting two years prior and was diagnosed with bilateral posterior vitreous detachments (PVD) and right eye retinal hemorrhage at that time. The patient had no history of eye surgery or other ocular disease. She did not require the use of glasses or contact lenses for visual correction. Past medical history was only significant for gout. She had no history of diabetes, hypertension, or dyslipidemia.
On physical examination, the patient presented with normal vital signs including blood pressure of 119/82 mm Hg. Visual acuity was 20/20 OD and 20/40 OS without the use of a pinhole. Pupils were equal and reactive to light with no relative afferent pupillary defect. There was no redness or conjunctivitis. Extraocular movements were full, and no visual field deficits were appreciated. Intraocular pressures were 15 mm Hg bilaterally, and there was no fluorescein uptake on slit lamp examination.
Point of care ultrasound of the left eye demonstrated a posterior chamber containing many echogenic opacities of varying size without acoustic shadowing (Figure 1). Movement of the eye along the long axis of the ultrasound probe revealed significant after-movement of the heterogeneous echogenic opacities within the vitreous humor, giving a “washing machine” appearance (Video 1). The scan was interpreted as vitreous hemorrhage (VH) without retinal detachment (RD). Accordingly, the patient was referred to the ophthalmology clinic. The ophthalmologist assessed the patient later that day. Visual acuity was 20/20 OD and 20/25 OS under ideal conditions using a pinhole to correct refractive error. Indirect ophthalmoscopy revealed asteroid hyalosis in the left eye. There was no evidence of VH or RD. No therapy was required, and subsequent follow-up was uneventful.
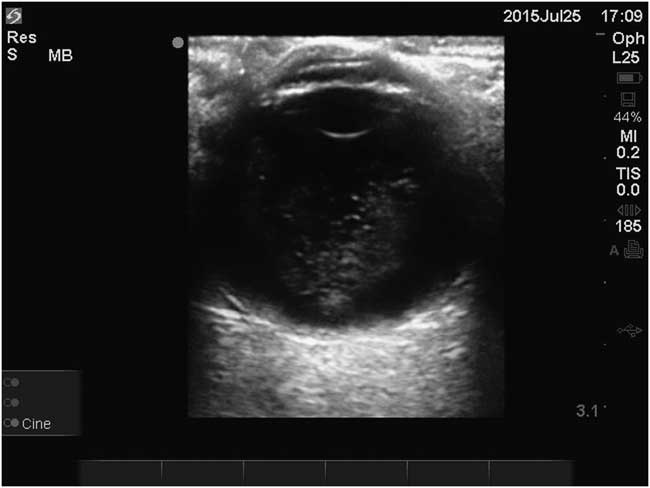
Figure 1 Transverse view of the left eye demonstrates echogenic opacities of varying size without acoustic shadowing in the vitreous humor due to asteroid hyalosis.
DISCUSSION
Ultrasound has been used for diagnosis in ophthalmology since the 1950s.Reference Chesney and Mohabir 1 More recently, point of care ocular ultrasound is finding a role in the ED for the diagnosis of time-sensitive, vision-threatening conditions such as RD.Reference Vrablik, Snead and Minnigan 2 Ocular ultrasound is performed by using a linear, high-frequency probe placed over a closed eyelid with copious amounts of gel (or a water balloon) used as an acoustic coupling medium in-between (Figure 2). The sonographer avoids placing pressure on the globe by bracing the scanning hand against the patient’s face (either the bridge of the nose or the zygomatic arch). Ocular presets are recommended, and normal anatomy is confirmed in the transverse plane with the patient’s eyes oriented forward. The proper plane is achieved when the lens and optic nerve are in the same view (Figure 3). Fan the transducer through the entire eye to visualize the entire globe. The patient is then asked to look left and right, allowing for a dynamic assessment of the posterior chamber in this plane. The same protocol is then repeated in a longitudinal plane (Figure 4). Comparison with the asymptomatic eye is recommended.

Figure 2 Proper probe position for ocular ultrasound in the transverse plane. Considerable gel is used to keep the probe off the eyelid while gently bracing the hand against the patient’s face.
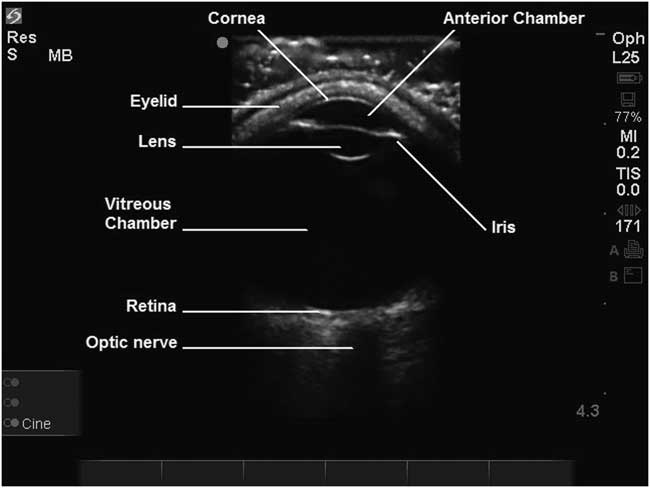
Figure 3 Normal ultrasound anatomy of the eye. In the correct plane, the lens and the optic nerve are both in view.

Figure 4 Proper probe position for ocular ultrasound in the longitudinal plane. Considerable gel is used to keep the probe off the eyelid while gently bracing the hand against the patient’s face.
RD and PVD both appear as a linear membrane in the posterior chamber that moves with ocular movements. RD is characterized by a thicker, more echogenic membrane typically attached to the optic nerve (Figure 5, Video 2), whereas PVD appears as a thinner, less echogenic, undulating membrane (Figure 6, Video 3).Reference Chesney and Mohabir 1 , Reference Shinar, Chan and Orlinsky 3 To visualize VH by ultrasound, the gain should be increased until echogenic material is seen in the posterior chamber. VH looks like multiple heterogeneous echogenic layers that distinctly “tumble” with ocular movement, earning the comparison to a washing machine (Figure 7, Video 4).Reference Chesney and Mohabir 1 , Reference Shinar, Chan and Orlinsky 3 As ocular ultrasound use becomes more prominent in the ED, it is important to understand when it may lead the operator astray. Accordingly, we report this case of asteroid hyalosis mimicking VH on ultrasound.
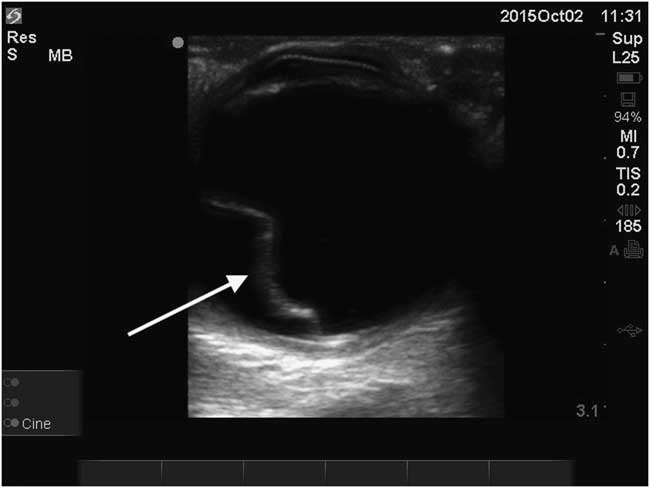
Figure 5 Ultrasound example of retinal detachment, characterized by a thick echogenic membrane in the vitreous chamber (arrow).
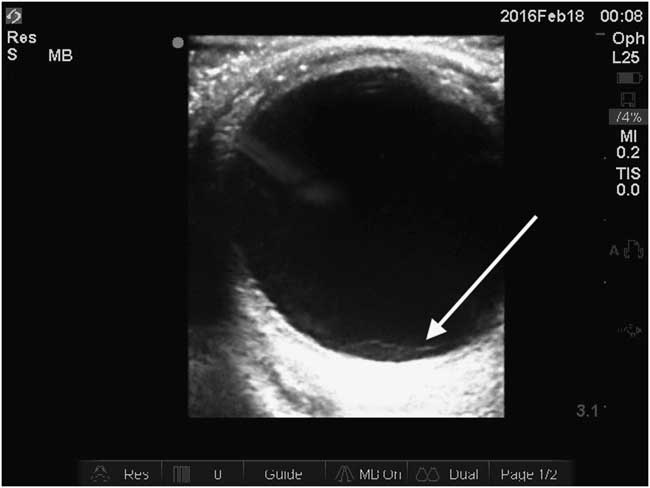
Figure 6 Ultrasound example of posterior vitreous detachment, characterized by a thin, poorly echogenic membrane in the vitreous chamber (arrow).
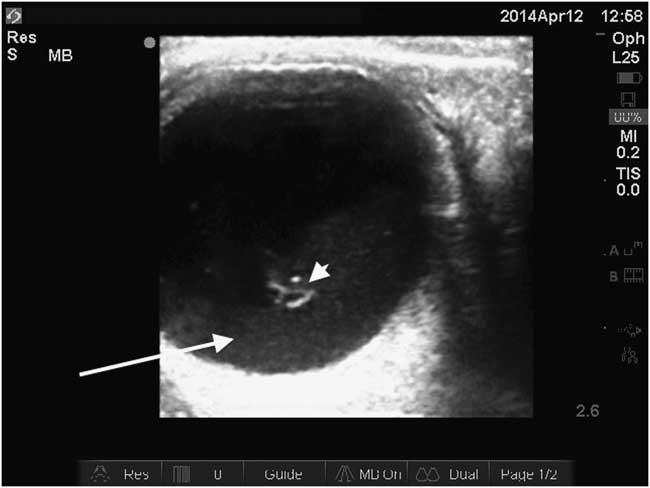
Figure 7 Ultrasound example of vitreous hemorrhage with echogenic blood layered posteriorly in the vitreous chamber (arrow). The overlying hyperechoic material is clotted blood (arrowhead).
Asteroid hyalosis is a degenerative condition of the vitreous associated with calcium phosphate and lipid deposits.Reference Heagley, Cantley and Pitelka 4 Large autopsy studies have found a prevalence of 0.83%–1.96%. It is associated with increased age, male gender, and PVD.Reference Fawzi, Vo and Kriwanek 5 , Reference Moss, Klein and Klein 6 Reported associations with hypertension, atherosclerosis, gout, and diabetes are controversial. Asteroid hyalosis is typically unilateral and asymptomatic, although there are case reports of floaters and decreased visual acuity.Reference Heagley, Cantley and Pitelka 4 , Reference McAlinden and Skiadaresi 7 Ophthalmoscopy reveals multiple yellow-white, iridescent opacifications of varied shape in the vitreous. Accordingly the condition was named for resembling “stars on a clear night.”Reference Yazar, Hanioglu and Karakoç 8 These particles move with eye movement and often obscure the retina. Asteroid hyalosis rarely requires treatment; vitrectomy is reserved for cases with significant vision loss without another etiology.Reference Kachewar and Kulkarni 10
Sonographically, there is considerable similarity between asteroid hyalosis and VH (Figure 1, Figure 7). Both result in posterior chamber echogenic opacities. The most striking similarity is the after-movement observed with ocular movement. As the eye ceases rotation, the vitreous continues to move causing the echogenicity from asteroid hyalosis and VH to swirl, resembling clothes tumbling in a washing machine (Video 1, Video 4).Reference Chesney and Mohabir 1 , Reference Shinar, Chan and Orlinsky 3 The described differences between asteroid hyalosis and VH are subtle and due to differences in echogenicity. Asteroid hyalosis echoes are usually more discrete echogenic opacities without posterior acoustic shadowing (Figure 1).Reference Kachewar and Kulkarni 10 VH echogenicity is described as heterogeneous echogenic layers, although significant hemorrhage can cause poorly-defined, hyperechoic clots (Figure 7).Reference Shinar, Chan and Orlinsky 3 As the sonographic similarities between asteroid hyalosis and VH are much more striking than the differences, asteroid hyalosis has considerable potential to be mistaken for VH.
CONCLUSION
As point of care ocular ultrasound is increasingly used by emergency physicians, awareness of possible ultrasound mimics, such as asteroid hyalosis, is important. Knowledge of asteroid hyalosis may be helpful for communication with specialist colleagues or interpretation of their consultations. However, it is of utmost importance to avoid the misdiagnosis of VH as asteroid hyalosis. Since asteroid hyalosis is a benign condition, it is important to be cautious and to manage these patients as presumptively having VH by seeking ophthalmologic assessment, especially if the patient is experiencing vision loss.
Competing Interest: None declared.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/doi:10.1017/cem.2016.358











