Introduction
Among adolescent girls and young women aged 15–24, 33 million in 61 countries are estimated to have an unmet need for voluntary family planning (FP) (MacQuarrie, Reference MacQuarrie2014). Those with an unmet need are sexually active women who do not wish to become pregnant but who are not using any method of contraception. Over the past several decades, unmet need has declined in many of these countries but only one in two married adolescent girls’ demand for FP (unmet need plus current use) has been satisfied. The youngest appear to be the most vulnerable, as 15- to 16-year-old married girls experience the greatest unmet need for FP (MacQuarrie, Reference MacQuarrie2014). Factors that prevent youth from accessing and using voluntary family planning and reproductive health (FP/RH) services have been documented extensively and include restrictive laws and policies; provider attitude, bias and judgement; inconvenient times, locations and fees; limited range of contraceptive method availability; perceptions of a lack of confidentiality; sociocultural pressures for early childbearing; fear of being seen; and embarrassment with procurement (Biddlecom et al., Reference Biddlecom, MunthalI, Singh and Woog2007b; Chandra-Mouli et al., Reference Chandra-Mouli, Mapella, John, Gibbs, Hanna, Kampatibek and Bloem2013, Kennedy et al., Reference Kennedy, Bulu, Harris, Humphreys, Malverus and Gray2013; Abajobir & Seme, Reference Abajobir and Seme2014; Abebe & Awoke, Reference Abebe and Awoke2014; Sulemana & Badasu, Reference Sulemana, Mumuni and Badasu2015; HIPs, 2015; Ayehu et al., Reference Ayehu, Kassaw and Hailu2016; Motuma et al., Reference Motuma, Syre, Egata and Kenay2016).
In a literature review of youth’s perceptions of barriers to accessing FP/RH services (Bender & Fulbright, Reference Bender and Fulbright2013), personal factors such as fear, embarrassment or insecurity were found to delay health-seeking behaviours and cause fear of ruined reputation. Lack of confidentiality at health centres was also a recurring barrier to FP/RH services access. In sub-Saharan Africa, the fear of being seen and lack of confidentiality have been shown to be barriers to FP/RH service use (Sulemana & Badasu, 2015; Ayehu et al., Reference Ayehu, Kassaw and Hailu2016; Nyblade et al., Reference Nyblade, Stockton, Nyato and Wamoyi2017).
Married young women and girls face unique barriers to accessing FP/RH services and are often neglected in programmes (Mekbib et al., Reference Mekbib, Erulkar and Belete2005; Bruce & Chong, Reference Bruce and Chong2006). Recently married girls and young women face intense social pressure to bear a child early in marriage (Rivera et al., Reference Rivera, Mello, Johnson and Chandra‐Mouli2001; Bruce & Chong, Reference Bruce and Chong2006). Even after the first birth, however, married youth still face barriers to accessing services. Because most have left school, married adolescents and young women in sub-Saharan Africa are often socially isolated and have restricted mobility, which creates barriers to obtaining care (Bruce & Chong, Reference Bruce and Chong2006; Biddlecom et al., Reference Biddlecom, Hessburg, Singh, Bankole and Darabi2007a). A qualitative study in Guatemala found that barriers preventing married young women aged 20–24 from accessing FP services included lack of knowledge about methods, fear of side-effects and infertility, beliefs that contraception is a sin, fear of social chastisement and husband’s opposition (Richardson et al., Reference Richardson, Allison, Gesink and Berry2016). In Uganda, a qualitative study of newly married adolescents found that even though couples communicated about timing of births, male opposition was a barrier to using family planning (Adams et al., Reference Adams, Salazar and Lundgren2013).
Access to voluntary contraceptive services is particularly important among married youth in Ethiopia where 40% of young women aged 20–24 were married by age 18 and 14% were married by age 15 (Central Statistical Agency & ICF, 2016a). Early age at marriage prevails in conservative areas, and when coupled with high rates of youth childbearing (55% of young women aged 20–24 have given birth; Central Statistical Agency & ICF, 2016a), Ethiopian youth are particularly vulnerable to maternal mortality and morbidity. In addition, despite the rise in voluntary use of modern contraceptive methods from 5% in 2000 to 37% in 2016 among married 15- to 24-year-olds, unmet need for family planning among this group remains substantial at 19%. Among 15- to 24-year-olds with a demand for family planning, unmet need is higher among those who are married (37%) than among those who have never been married (29%) (Central Statistical Agency & ICF, 2016b). Furthermore, nearly a quarter of pregnant 15- to 24-year-olds felt that their pregnancy was mistimed or unwanted (Central Statistical Agency & ICF, 2016a). Given this context, research on the barriers to accessing FP/RH services is needed and should be part of broader efforts to improve the health and agency of young women and girls, along with interventions aimed at delaying the age at marriage.
Stigma and FP/RH service utilization
Goffman (Reference Goffman1963) defined stigma as a characteristic or attribute of an individual that society rejects and discredits. Since then, different types of stigma have been described including: internalized stigma (the acceptance of society’s exclusionary views towards oneself); anticipated stigma (the belief that others will discriminate against oneself: Weiss, Reference Weiss2008; Quinn & Chaudoir, Reference Quinn and Chaudoir2009); and enacted stigma or discrimination (the experience of unfair treatment by others: Scambler & Hopkins, Reference Scambler and Hopkins1986). Stigma can prevent individuals from seeking help or health services and can lead to thoughts of suicide, depression or self-isolation from social settings.
Stigma has often been described in the fields of epilepsy (Scambler, Reference Scambler2004; Bautista et al., Reference Bautista, Shapovalov and Shoraka2015), HIV (Parker & Aggleton, Reference Parker and Aggleton2003; Sandelowski et al., Reference Sandelowski, Lambe and Barroso2004; Yebei et al., Reference Yebei, Fortenberry and Auyku2008; Jiménez et al., Reference Jiménez, Puig, Ramos, Morales, Asencio and Sala2010; Chambers et al., Reference Chambers, Rueda, Baker, Wilson, Deutsch and Raeifar2015), abortion (Norris et al., Reference Norris, Bessett, Steinberg, Kavanaugh, De Zordo and Becker2011; Cockrill et al., Reference Cockrill, Upadhyay, Turan and Greene Foster2013; Gelman et al., Reference Gelman, Rosenfeld, Nikolajski, Freedman, Steinberg and Borrero2017), mental health (Wahl, Reference Wahl1999; Corrigan, Reference Corrigan2004; King et al., Reference King, Dinos, Shaw, Watson, Stevens and Passetti2007), sexual violence (Coffey et al., Reference Coffey, Leitenberg, Henning, Turner and Bennett1996; Murray et al., Reference Murray, Augustinavicius, Kaysen, Rao, Murray and Wachter2018), hepatitis C (Butt et al., Reference Butt, Paterson and McGuinness2007; Lekas et al., Reference Lekas, Siegel and Leider2011) and obesity (Puhl & Huer, Reference Puhl and Heuer2010; Brewis et al., Reference Brewis, Trainer, Han and Wutich2017). The concept of stigma, however, has yet to be fully developed or applied to married girls and young women’s need for voluntary contraceptives and may be an important barrier to use. For example, a young married girl who wants to postpone her first birth may want to use a contraceptive method but anticipates negative attitudes (such as judgement from health providers) or discrimination (like verbal or physical abuse from husband) or feels shame for wanting to use contraception that prevents her from accessing contraceptive services.
Two recent qualitative studies in Tanzania (Nyblade et al., Reference Nyblade, Stockton, Nyato and Wamoyi2017) and Ghana (Hall et al., Reference Hall, Manu, Morhe, Challa, Loll and Dozier2015) looked at different dimensions of stigma and FP/RH, primarily among unmarried girls. In the Tanzanian study, a limited number of respondents had ever personally experienced the process of obtaining a contraceptive method. Therefore, the barriers identified to accessing services were related to perceptions of service delivery and anticipated stigma if they were to seek services, including: fear of lack of confidentiality, denial of services, excessive questioning, negative labelling or parental supervision at visit.
The Ghana study, on the other hand, identified enacted and internalized stigma associated with pregnancy and childbearing, among other themes, but not in relation to contraceptive methods. Hall et al. (Reference Hall, Manu, Morhe, Harris, Loll and Ela2017) went on to develop and validate an adolescent FP/RH stigma measure that included subscales for enacted and internalized stigma based on their qualitative findings. While their measures of enacted and internalized stigma included several items associated with contraceptives, most of the questions asked were about respondents’ beliefs and their perceptions of community members’ perceptions as opposed to respondents’ own internalization of FP/RH issues or experiences of discrimination.
Anticipated stigma (expectation of discrimination from others) has been shown to be a barrier to accessing services in the context of mental health (Iversen et al., Reference Iverson, van Staden, Hughes, Greenberg, Hotopf and Rona2011) and intimate partner violence (Overstreet & Quinn, Reference Overstreet and Quinn2013) but not family planning. Therefore, the current study measures and validates an anticipated stigma index associated with FP need, assesses anticipated stigma among both married FP users and married non-users, and explores its effect on unmet need after adjusting for other barriers to FP use.
Methods
Data
The study analysed data from a cross-sectional household survey in five Ethiopian regions: Amhara, Benishangul-Gumuz, Oromia, SNNP and Tigray. Data were collected from 15- to 24-year-old girls and young women between January and July 2016. The sample was designed to measure the effect of distance to a youth-friendly service (YFS) site on utilization of FP, HIV and maternal health services. The Regional Health Bureaus listed 247 YFS sites in rural areas. Five per cent of YFS sites and one non-YFS site were randomly selected as the sampling frame from each region using probability proportional to size. Fourteen YFS sites and five non-YFS sites were chosen across the five regions.
A stratified, two-stage cluster design was employed. Enumeration areas (EAs) were the primary sampling unit (PSUs) in the first stage. The EAs were stratified by distance from the YFS site (<5 km or 5 km to <10 km) and three EAs were selected from each stratum. One EA was also selected from within 5 km of each non-YFS site. Eligible households were randomly selected, and one eligible respondent per household was selected using a KISH grid (Kish, Reference Kish1949). A detailed description of the sampling strategy is available in the study report (Jain et al., Reference Jain, Ismail, Tobey and Erulkar2017). The total number of females interviewed was 1329 with a response rate of approximately 94%.
Questionnaires obtained information on a range of issues including social cohesion, autonomy, attitudes towards FP, fertility intentions, use of FP, maternal health and basic health services and awareness and use of services at YFS sites. Questionnaires were translated into multiple languages including Amharic, Tigrinya and Oromo. Informed consent was obtained from all respondents in the survey.
Variables
Dependent variable
The outcome variable was ‘unmet need for family planning’ calculated using the revised definition of unmet need (Bradley et al., Reference Bradley, Croft, Fishel and Westoff2012). The categories of need are: 1) met need=females who are currently using a contraceptive method; 2) no need=currently pregnant females who wanted their pregnancy at that time and non-pregnant females who would like to have a child in the next 2 years; and 3) unmet need=non-users of any method who reported that they do not want to have any more children, would like their next child in more than 2 years or were unsure of the timing, and currently pregnant women who reported that they did not want the pregnancy at all or wanted it later. Following the terminology used in the literature, total demand equals the sum of current contraceptive users (met need) plus those with an unmet need.
Anticipated stigma index
The main predictor variable was a composite index that captured anticipated stigma. The index was developed using a pool of fourteen questions that were developed based on preliminary findings from a qualitative study conducted with youth in Tanzania (Nyblade et al., Reference Nyblade, Stockton, Nyato and Wamoyi2017), in addition to the researchers’ knowledge of FP service barriers among sexually active Ethiopian youth. Respondents were asked to answer a series of attitudinal questions on a 4-point Likert scale with answers ranging from ‘strongly agree’ to ‘strongly disagree’. They were prompted with the following statement: ‘Suppose that you were planning to get services related to FP next week. Please keep this scenario in mind and tell me if you: strongly disagree, disagree, agree or strongly agree with the following statements.’ Principal component factor analysis was used to reduce the items. Items were considered for removal if their factor loading was less than 0.50 (Matsunaga, Reference Matsunaga2015). The reliability of the index was tested using Cronbach’s α with a cut-off of 0.60 (Loewenthal, Reference Loewenthal2001). The five items in the index were combined to form a composite score ranging from 0 to 5, which was then dichotomized into 0=no agreement across all five items and 1=agreement on at least one item.
Other independent variables
Several additional variables were considered, including distance of household from a YFS or non-YFS site to assess physical access to, and availability of, quality services, women’s participation in decision-making to assess empowerment, ownership of personal savings to assess financial autonomy and visiting a mosque/church in their leisure time to assess religiosity. The decision-making measure was developed based on four items and came from the question: Who makes decisions about (1) your health; (2) school attendance; (3) who you spend time with; and (4) about where you go?’ Each item was dichotomized into whether the respondent had any say in the decision (independently or jointly with someone else such as her husband or extended family member) or whether she had no say in the decision. A composite index was formed ranging from 0 to 4, where 4 indicates the respondent had a say in all four aspects of decision-making. This score was dichotomized into no/low (0 to 3) involvement and all (4) involvement.
Analysis
The sample was restricted to married youth with a demand for contraception, i.e. with a met or unmet need for FP. Respondents reporting no need for FP were excluded from the analysis because they were youth who were either pregnant and wanted the child at that time or who wanted to get pregnant in the next 2 years. Unmarried respondents were also excluded because the majority reported that they had not had sex.
Descriptive statistics were calculated for respondent characteristics. Bivariate models of all covariates against the outcome variable were conducted using Pearson’s χ 2 test for categorical variables and t-tests for continuous variables. Multivariate logistic regression was used, adjusting the association for age, parity, ever attended school, religion and region of residence. Variables that were statistically significant in the bivariate analysis were included in the multivariate model but in some instances non-significant variables were included if they had theoretical importance. All statistical analyses were conducted in Stata Version 13 (StataCorp, 2013).
Results
Respondents’ characteristics
The total number of married youth aged 15–24 years with a demand for contraception was 371: 56% (n=207) with a met need and 44% (n=164) with an unmet need. Most married youth were aged 20–24 (82%), had at least one child (83%) and had attended school (73%) (Table 1). Over half of the respondents were married before the age of 18 (58%, data not shown) and 21% were at least 10 years younger than their husband.
Table 1 Percentage distribution of married adolescent youth aged 15–24 years by characteristics (N=371)
a Proportions do not add up to 100% because of missing values.
Anticipated stigma index
Responses on each of the fourteen items were recoded as binary variables: 1 for agree and strongly agree and 0 otherwise. The percentage of respondents who agreed with each item in addition to the factor loadings are presented in Table 2. Two factors formed: 1) anticipated stigma, which included measures related to worry, fear and embarrassment; and 2) desire to be accompanied to a facility for FP services. The second factor was explored in the analysis but was excluded from the results because of the low α score and lack of significant relationships.
Table 2 Factor loadings for anticipated stigma and desire to be accompanied indices (N=371)
The factor loadings forming the indices are in bold.
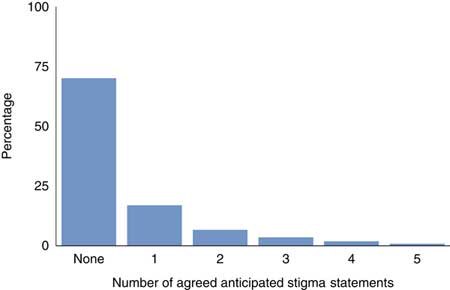
The percentage of respondents who agreed with the five items of the anticipated stigma index are presented in Fig. 1. Eight per cent of youth agreed that they would be embarrassed to discuss FP with a provider and 9% agreed that they would be embarrassed about wanting more FP information. Ten per cent agreed that they would worry if people in their community learned that they needed contraception while 14% agreed that they would worry if their parents learned of their FP needs. Twelve per cent feared being seen at the facility. Overall, 30% of respondents agreed with at least one of these five items.
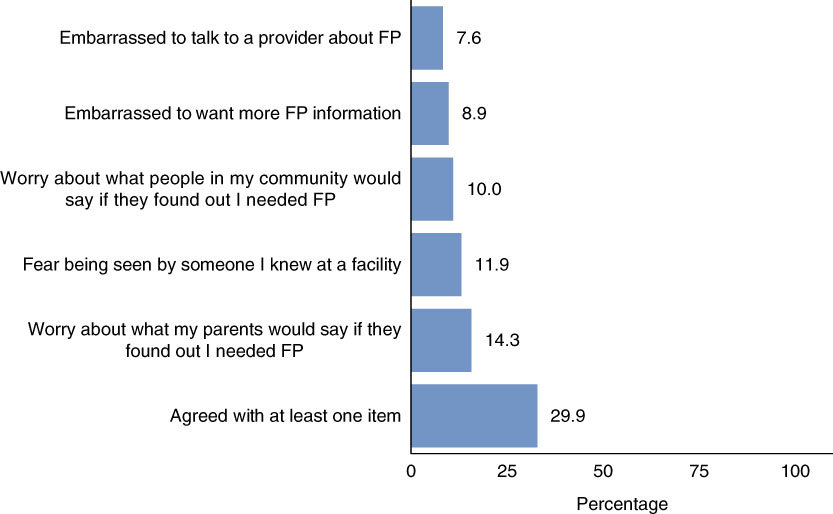
Figure 1 Agreement with anticipated stigma statements by 15- to 24-year-old married females.
Figure 2 shows the results of the composite score for the anticipated stigma index. Most respondents reported no anticipated stigma (70%). Agreement with one item was 17% and agreement across all five items was 1%.
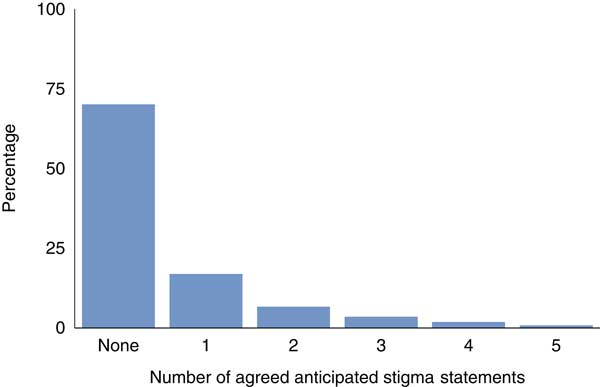
Figure 2 Percentage distribution of 15- to 24-year-old married females by number of agreed anticipated stigma statements.
To test criterion validity of the anticipated stigma index, the known-group validity method was used (Netemeyer et al., Reference Netemeyer, Bearden and Sharma2003) and differences in mean scores on the anticipated stigma index were compared among respondents who visited and did not visit a health facility for FP services in the 6 months preceding the survey. The mean score on the anticipated stigma index was 0.36 among respondents who sought FP services and 0.66 among those who did not 6 months preceding the survey (data not shown). The difference in these means was statistically significant with a p-value of 0.004.
Bivariate analysis
Table 3 presents the bivariate analysis of unmet need for FP by anticipated stigma index, distance from a YFS site, involvement in decision-making, own personal savings, time spent at mosque/church and respondent characteristics. Youth who agreed with the anticipated stigma statements were more likely to have an unmet need. Youth who lived less than 5 km from a YFS site, who had their own savings and who had spent time at a mosque or church were less likely to have an unmet need. Unmet need appeared to increase with number of living children and to decrease when youth marry later in life. Unmet need was also higher for youth who had never attended school.
Table 3 Bivariate analysis of unmet need for family planning (N=371)
*p≤0.05; **p≤0.01; ***p≤0.001.
Two known barriers to contraceptive use – knowledge of at least one FP method and where to obtain FP services – were excluded from the analysis because 100% of respondents could name at least one FP method and knew a place where they could get it. Among respondents with an unmet need, 45% had used a contraceptive method in the past, and of these past users, 34% intended to use a contraceptive method in the next 12 months (data not shown).
Multivariate analysis
Unadjusted and adjusted odds ratios (OR) for the effect of anticipated stigma on unmet need for FP are presented in Table 4. The unadjusted OR for the effect of anticipated stigma index on unmet need was 1.86 (95% CI: 1.19–2.91). The adjusted OR increased in magnitude to 1.97 and remained significant (95% CI: 1.16–3.36). Youth who lived less than 5 km from a non-YFS site were significantly more likely to have an unmet need for FP compared with those who lived less than 5 km from a YFS site (AOR: 2.11; 95% CI: 1.04–4.30) The lincom command was run to compare youth living between 5 and 10 km from a YFS site with youth living less than 5 km from a non-YFS site and found that youth living further away from a YFS site were less likely to have an unmet need. However, this relationship was not statistically significant.
Table 4 Unadjusted and adjusted Odds Ratios (ORs) of unmet need for family planning
Ref., reference category.
*p≤0.05; **p≤0.01; ***p≤0.001.
Significant associations were maintained in the adjusted logistic model for unmet need by education and religion. The Hosmer–Lemeshow goodness-of-fit test was applied and showed that this model fitted the data reasonably well.
Discussion
The results of this study show that among married female youth in Ethiopia, anticipated stigma is significantly associated with an unmet need for voluntary family planning. This effect remains significant after adjusting the association for other known barriers to FP use, including proximity to a YFS facility. The anticipated stigma measures include embarrassment discussing contraceptives with providers, worry about parental or other community members’ attitudes towards married youth who need FP and fear of being seen when accessing contraceptive services. These issues stem from broader social and community-level opinions of married girls’ use of contraceptives. In Ethiopia, where early marriage remains deeply rooted in tradition and pressures to demonstrate fertility are high, the ability to access FP/RH services and make decisions about ones’ own health is still limited, and the reproductive health of married girls and young women can suffer as a result (Shaw, Reference Shaw2009). It is therefore critical that efforts to increase access to FP/RH services are comprehensive, including interventions to delay the age at marriage and increase the autonomy of married girls and young women (Erulkar et al., Reference Erulkar, Medhin and Weissman2017).
The study results also show that youth who live close to a non-YFS site (<5 km) are significantly more likely to have an unmet need compared with youth who live close to a YFS site (<5 km). In Ethiopia, YFS sites have been scaled-up to over 300 health facilities across the country (Pathfinder International, 2012). Youth-friendly services aim to reduce stigma specifically through peer-to-peer comprehensive counselling on FP/RH and life skills for youth and peer educator-led awareness activities for parents, youth and community leaders (Pathfinder International, 2016). Creating YFS services also involves training providers and support staff to be non-judgemental, to be technically competent in adolescent-specific needs and to reduce stigma at facilities. While improving service quality and reducing provider bias and judgement towards youth’s access of FP services is important, it alone is not sufficient to increase use of services (Mmari & Magnani, Reference Mmari and Magnani2003).
Interventions that aim to increase demand for voluntary FP/RH services have also been met with varying degrees of success (Denno et al., Reference Denno, Hoopes and Chandra-Mouli2015). In Ethiopia, community-based programmes to delay age at marriage, support girls to stay in or re-enter school and provide economic incentives to keep girls in school have been successful (Erulkar & Muthengi, Reference Erulkar and Muthengi2009; Muthengi & Erulkar, Reference Muthengi and Erulkar2011; Erulkar et al., Reference Erulkar, Medhin and Weissman2017). Following the success of these programmes, holding community dialogues to change social norms about young people’s use of FP/RH services, in addition to changing norms about age at marriage and educational attainment, may be a promising intervention to reduce the barriers to contraceptive access caused by anticipated stigma. However, working on changing societal norms around married youth and FP will take time, and these findings suggest that interventions need to explore how to support and empower married youth to strategize effective ways of accessing services in an environment where societal/community norms may expect them not to use family planning.
This study also showed that among married youth with an unmet need, 45% had used a contraceptive method previously. Further analysis showed that 42% of previous FP users with an unmet need strongly agreed with the statement ‘my boyfriend/partner/husband would support me in my decision to get FP’ compared with 24% of never users with an unmet need, and this difference was statistically significant. This suggests that married youth who were previous contraceptive users were able to overcome family – specifically husband or partner – barriers to use services. In addition, previous FP users with an unmet need were more likely to agree with the anticipated stigma index, have personal savings and have ever attended school compared with never users. Furthermore, among the previous FP users with an unmet need, 34% reported that they intend to use a contraceptive method in the next 12 months while 66% said they intend to use in more than 2 years, were unsure of the timing or did not intend to use in the future. Future research should seek to understand why these past users with an unmet need do not intend to use in the future, especially for reasons other than to get pregnant, so that interventions can be designed to support them to resume FP use (Jain et al., Reference Jain, Obare, RamaRao and Askew2013).
There are several limitations to this study. The first is that since this was a cross-sectional survey, causality could not be determined, and the results need to be interpreted accordingly. This also limited the ability to test the predictive validity of the anticipated stigma index against future behaviours. Another limitation is that there may be a certain amount of respondent bias where respondents are under-reporting contraceptive use, and therefore over-reporting unmet need, due to the stigma associated with the behaviour. This could cause a potential overestimation of the relationship between anticipated stigma and unmet need. The findings are limited to married youth in Ethiopia and thus are not generalizable to other populations such as unmarried sexually active youth or to other country contexts.
Despite these limitations, the anticipated stigma index does appear to be a valid and reliable measure that could be replicated and tested in other contexts and among other populations. Longitudinal research could show how the anticipated stigma index influences future service use and contraceptive use behaviours. Another area of research that is noteworthy is to explore why and how FP users who reported anticipated stigma overcome barriers. This information would enable programmes to better design interventions that support married youth who experience stigma and are not using voluntary family planning.
Acknowledgments
The authors thank Lemi Negeri, who served as a research coordinator during this study. They also sincerely thank Mihira Karra, Erika Martin, Erika Houghtaling and Rabab Pettitt of USAID for their useful feedback on the manuscript. The manuscript benefited from the feedback at the Population Association of America meeting held in Chicago, Illinois, US, in April 2017, where it was presented as an oral presentation. They would also like to acknowledge and thank the research assistants and drivers who collected the data in Ethiopia, and are deeply grateful to the youths who participated in the study and shared their time and experiences.
Ethical Approval
Free and informed consent was obtained from all respondents. Younger girls provided their assent and informed consent was obtained from an adult guardian in the household. This study received ethical approval from the Population Council Institutional Review Board and the Ethiopian Public Health Institute. The authors assert that the study complies with the Helsinki Declaration of 1975, as revised in 2008.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding
The Evidence Project is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of cooperative agreement No. AIDOAA-A-13-00087. The contents of this manuscript are the sole responsibility of the Evidence Project and Population Council and do not necessarily reflect the views of USAID or the United States Government.