CLINICAL SCENARIO
A 43-year-old male, with a history of chronic back pain, presents to the emergency department (ED) with acute onset chronic pain. He states he “tweaked something” and has been debilitated by back pain, radiating down both his legs, for 24 hours. He has not had a bowel movement but denies noticing any “saddle anesthesia.” His clinical exam is limited by pain, and it is difficult to determine if he has objective weakness. His perineal sensation is intact, as is his sensation upon digital rectal examination. The patient has a post-void residual of 250 mL, but you are unsure how to interpret this value. As an emergency physician, when should you suspect, and how should you evaluate cauda equina syndrome?
KEY CLINICAL QUESTIONS
- 1
How common is cauda equina syndrome in the ED? Who is the “typical patient,” and what is the most likely cause?
The incidence of cauda equina syndrome ranges from 1:33,000 to 1:100,000 cases, with incidence peaking in the 4th decade of life. A common misconception is considering cauda equina syndrome a pathology of our geriatric patients, when in fact, it is our young patients who are most at risk following an inciting incident. Although a multitude of etiologies exist, disc herniation at the L4/L5 or L5/S1 level accounts for 50% of cases.Reference Long, Koyfman and Gottlieb1
- 2.
What is cauda equina syndrome, and why is early diagnosis so crucial?
Although many definitions exist in the literature, cauda equina syndrome can be best conceptualized into three main categories: suspected, incomplete, and retentive. Patients with cauda equina suspected may present with bilateral radiculopathy, while those with cauda equina incomplete will present with urinary difficulties, altered sensation in the perineum, decreased desire to void, and weak stream. Finally, those with cauda equina retention present with painless urinary retention, overflow incontinence, and loss of rectal tone.Reference Todd2 Given the worsening long-term prognosis as patients progress through each of these definitive categories, emergency physicians should strive to suspect and diagnose cauda equina syndrome early rather than when a patient has developed objective neurologic dysfunction. With early intervention, patients treated at the cauda equina incomplete stage have a high likelihood of regaining normal bowel, bladder, and sexual function. By comparison, those patients who have a delay to diagnosis, and progress to a state of cauda equina retention, may sustain permanent neurologic dysfunction.
- 3.
Can I rule out cauda equina syndrome clinically in the ED?
There are no clinical signs or symptoms that individually are sensitive nor specific enough to allow for the diagnosis of cauda equina syndrome. The diagnosis should be considered if the patient reports a combination of any of several of the following symptoms: new onset bilateral sciatica, reduced perineal sensation, urinary retention, loss of anal tone, erectile dysfunction, motor/sensory changes in lower extremities. Unfortunately, symptoms such as a change in perineal sensation may be subtle and missed on a cursory examination; while findings of decreased rectal tone lack inter-relater reliability.Reference Todd2 Saddle anesthesia, bowel incontinence, reduced anal tone, leg pain, urinary retention, urinary incontinence, and back pain all have weak GRADE evidence for the diagnosis of cauda equina syndrome.Reference Dionne, Adefolarin and Kunzelman3 As such, no element of patient history or physical examination yields adequate sensitivities or specificities for the diagnosis of cauda equina syndrome, and definitive imaging must be pursued if the diagnosis is suspected.
- 4.
What other point of care testing is useful in for this diagnosis?
Post-void residuals may serve as a helpful diagnostic adjunct in the work-up of cauda equina syndrome. Normal bladder emptying is often defined as a post-void residual volume of <50 mL in a young healthy person, while elderly patients may retain up to 100 mL of urine without evidence of sinister pathology. Using a post-void residual of 200 mL to risk stratify patients with suspected cauda equina syndrome demonstrated a sensitivity of 94%, with a negative predictive value of 98%.Reference Venkatesan, Nasto, Tsegaye and Grevitt4 Additional studies have reported improved odds ratios by using higher post-void residual volumes; however, this approach may compromise sensitivity for the diagnosis.
- 5.
Why is MRI the gold standard for this diagnosis?
MRI is the gold standard for the diagnosis of cauda equina syndrome. Similar sensitivities and specificities, of >80%, are reported for the use of a computed tomography-myelogram; however, MRI has several advantages, including accessibility in the ED. It also has the ability to differentiate cauda equina syndrome secondary to disc pathology from alternative pathologies, such as infection or neoplasm.Reference Long, Koyfman and Gottlieb1
- 6.
How urgently should I consult for surgical intervention with cauda equina syndrome?
Multiple retrospective studies have attempted to determine the optimal timing within which surgical intervention should occur (e.g., <24 hours, 24–48 hours, and >48 hours), but all have significant methodological shortcomings. Despite the lack of a clearly defined timeline from diagnosis to surgical decompression, it is well accepted that surgery should be expeditiously undertaken after the diagnosis of cauda equina syndrome has been made, typically within 24 hours of diagnosis. As such, the emergency physician should seek prompt consultation with a spinal surgeon for definitive management at the time of diagnosis.
SUMMARY/CONCLUSION
Cauda equina syndrome is a critical, but often elusive, diagnosis in the ED (Figure 1). No elements of patient history or physical examination have adequate sensitivity to rule out the diagnosis of cauda equina syndrome, and suspicion must prompt further work-up. Adjuncts, such as post-void residual of >200 mL may help to risk-stratify patients and expedite definitive imaging. Prompt spinal surgery consultation should be pursued at the time of diagnosis for definitive management.
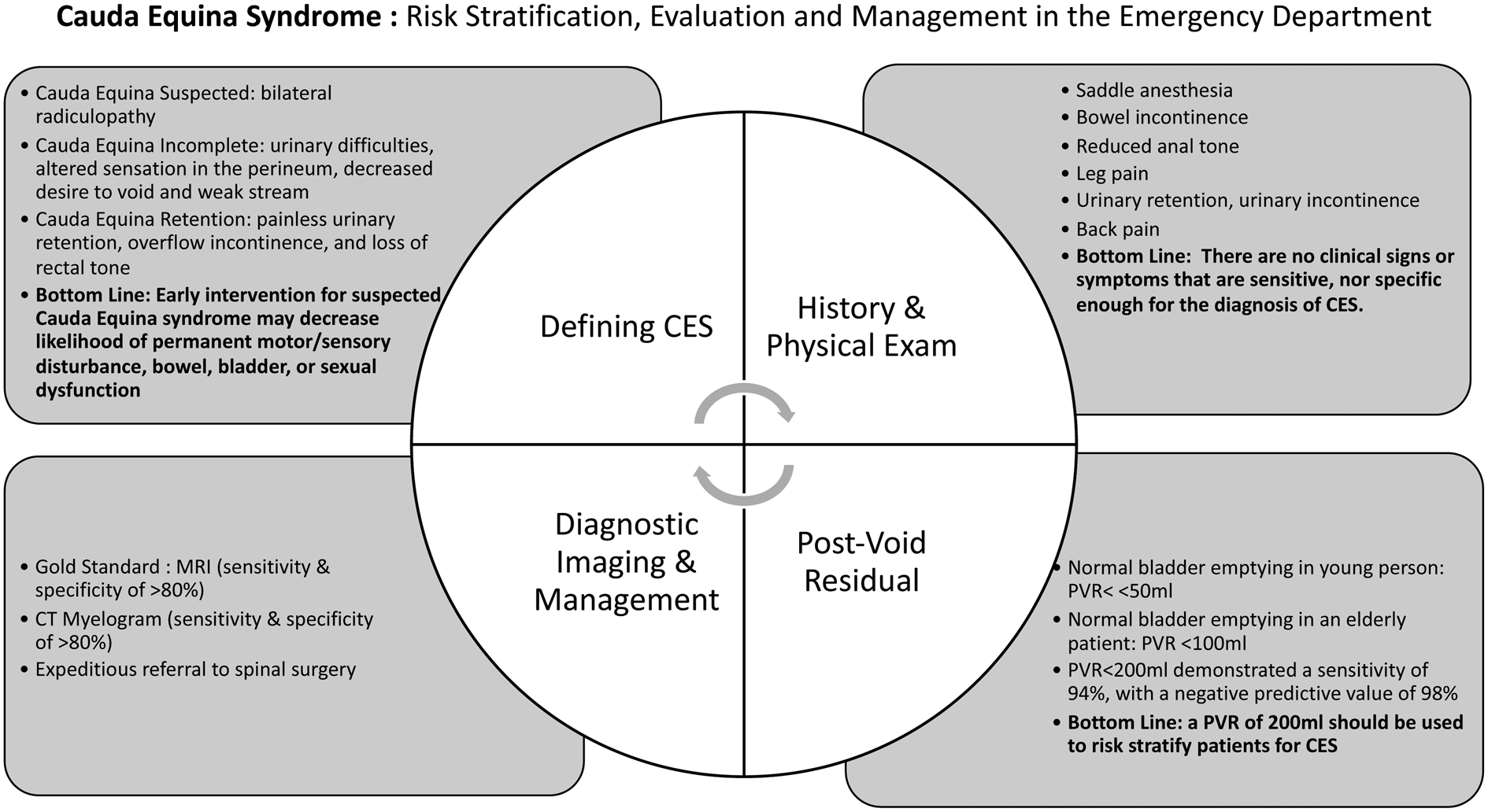
Figure 1. Cauda equine syndrome: risk stratification, evaluation, and management in the emergency department.