Introduction
Coronavirus disease 2019 (COVID-19) is a novel infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Wiersinga et al., Reference Wiersinga, Rhodes, Cheng, Peacock and Prescott2020). After the World Health Organization (WHO) declared COVID-19 a pandemic on March 2020, 81 658 440 confirmed cases were reported worldwide in December 2020, and 1 802 206 of those led to death (WHO, 2020a). In South Korea, 61 769 confirmed cases and 917 deaths were reported in December 2020, indicating a mortality rate of approximately 1.5% (Ministry of Health and Welfare, 2020).
Personal infection prevention activities, such as mask-wearing, washing hands and social distancing, are important to reduce SARS-CoV-2 infection risk (Doung-Ngern et al., Reference Doung-Ngern, Suphanchaimat, Panjangampatthana, Janekrongtham, Ruampoom, Daochaeng, Eungkanit, Pisitpayat, Srisong, Yasopa, Plernprom, Promduangsi, Kumphon, Suangtho, Watakulsin, Chaiya, Kripattanapong, Chantian, Bloss, Namwat and Limmathurotsakul2020; Shi et al., Reference Shi, Hu, Peng, Tang, Wang, Su, Luo, Wu, Zhang, Zhang, Anderson, Zhong, Qiu, Yang and Huang2021). Patients with mental illness are vulnerable to SARS-CoV-2 infection because of behavioural changes associated with cognitive deterioration (Yao et al., Reference Yao, Chen and Xu2020), especially without their caregivers. Some experts have proposed that patients with mental illness are at high risk of SARS-CoV-2 infection due to a lack of awareness of infection risk and a lack of commitment to personal prevention activities (Druss, Reference Druss2020; Shinn and Viron, Reference Shinn and Viron2020; Yao et al., Reference Yao, Chen and Xu2020).
Severe COVID-19 outcomes following SARS-CoV-2 infection are also a concern for patients with mental illness. Psychiatric symptoms are associated with health-risk behaviours such as smoking and drinking (Scott and Happell, Reference Scott and Happell2011; Bartlem et al., Reference Bartlem, Bowman, Bailey, Freund, Wye, Lecathelinais, McElwaine, Campbell, Gillham and Wiggers2015), explaining the higher prevalence of non-communicable diseases (NCDs) among patients with mental illness than in the general population (Himelhoch et al., Reference Himelhoch, Lehman, Kreyenbuhl, Daumit, Brown and Dixon2004; Walker et al., Reference Walker, McGee and Druss2015). The risk factors of severe COVID-19 identified to date are male sex, older age and severe medical conditions (Richardson et al., Reference Richardson, Hirsch, Narasimhan, Crawford, McGinn and Davidson2020; Williamson et al., Reference Williamson, Walker, Bhaskaran, Bacon, Bates, Morton, Curtis, Mehrkar, Evans, Inglesby, Cockburn, McDonald, MacKenna, Tomlinson, Douglas, Rentsch, Mathur, Wong, Grieve, Harrison, Forbes, Schultze, Croker, Parry, Hester, Harper, Perera, Evans, Smeeth and Goldacre2020; Zhou et al., Reference Zhou, Yu, Du, Fan, Liu, Liu, Xiang, Wang, Song, Gu, Guan, Wei, Li, Wu, Xu, Tu, Zhang, Chen and Cao2020). The high prevalence of NCDs and poor prognoses for subsequent medical conditions increase the risk of adverse outcomes following SARS-CoV-2 infection in patients with mental illness (Momen et al., Reference Momen, Plana-Ripoll, Agerbo, Benros, Børglum, Christensen, Dalsgaard, Degenhardt, Jonge, Debost, Fenger-Grøn, Gunn, Iburg, Kessing, Kessler, Laursen, Lim, Mors, Mortensen, Musliner, Nordentoft, Pedersen, Petersen, Ribe, Roest, Saha, Schork, Scott, Sievert, Sørensen, Terry, Stedman, Vestergaard, Vilhjalmsson, Werge, Weye, Whiteford, Prior and McGrath2020). While studies have reported that SARS-CoV-2 infection risk and severe clinical outcomes are high among patients with mental illness due to their clinical characteristics (Druss, Reference Druss2020; Yao et al., Reference Yao, Chen and Xu2020), there is a lack of quantitative research supporting this claim.
This study aimed to investigate whether SARS-CoV-2 infection risk and COVID-19-related death are higher among patients with mental illness than among those without a mental illness. We analysed the association between infection risk and mortality from SARS-CoV-2 and patients with mental illness, using data from a South Korean database.
Material and methods
Data collection and study participants
Data from the COVID-19 database of National Health Insurance Service (NHIS-COVID DB), which combines data from the Korea Disease Control and Prevention Agency (KDCA) and the National Health Insurance Service (NHIS) were used to analyse the association between infection risk and mortality from SARS-CoV-2 in patients with mental illness. The NHIS-COVID DB provides nationwide data on eligibility, insurance, medical examination results and treatment history of COVID-19 and control groups (National Health Insurance Service, 2020). The database includes comprehensive 5-year medical records of 8070 COVID-19 patients diagnosed between 1 January 2020 and 30 May 2020, and of those in the control group who did not have a history of being tested for COVID-19 during that time. The control group was 15 times (121 050 patients) the size of the COVID-19 group. Patients from the control group without a history of SARS-CoV-2 testing were selected using stratified sampling. To stratify factors, sex (male, female), age (0–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79 and ⩾80 years) and region of residence (Seoul, Gyeonggi-do, Daegu, Gyeongsangbuk-do, others) were considered, and random sampling was used within a single stratum (National Health Insurance Service, 2020). Since paediatric and adolescent patients with a mental illness exhibit characteristics different from those of adult patients, children aged 19 years and under were excluded. In total, 123 408 patients aged ⩾20 years from the NHIS-COVID DB were included (Fig. 1).
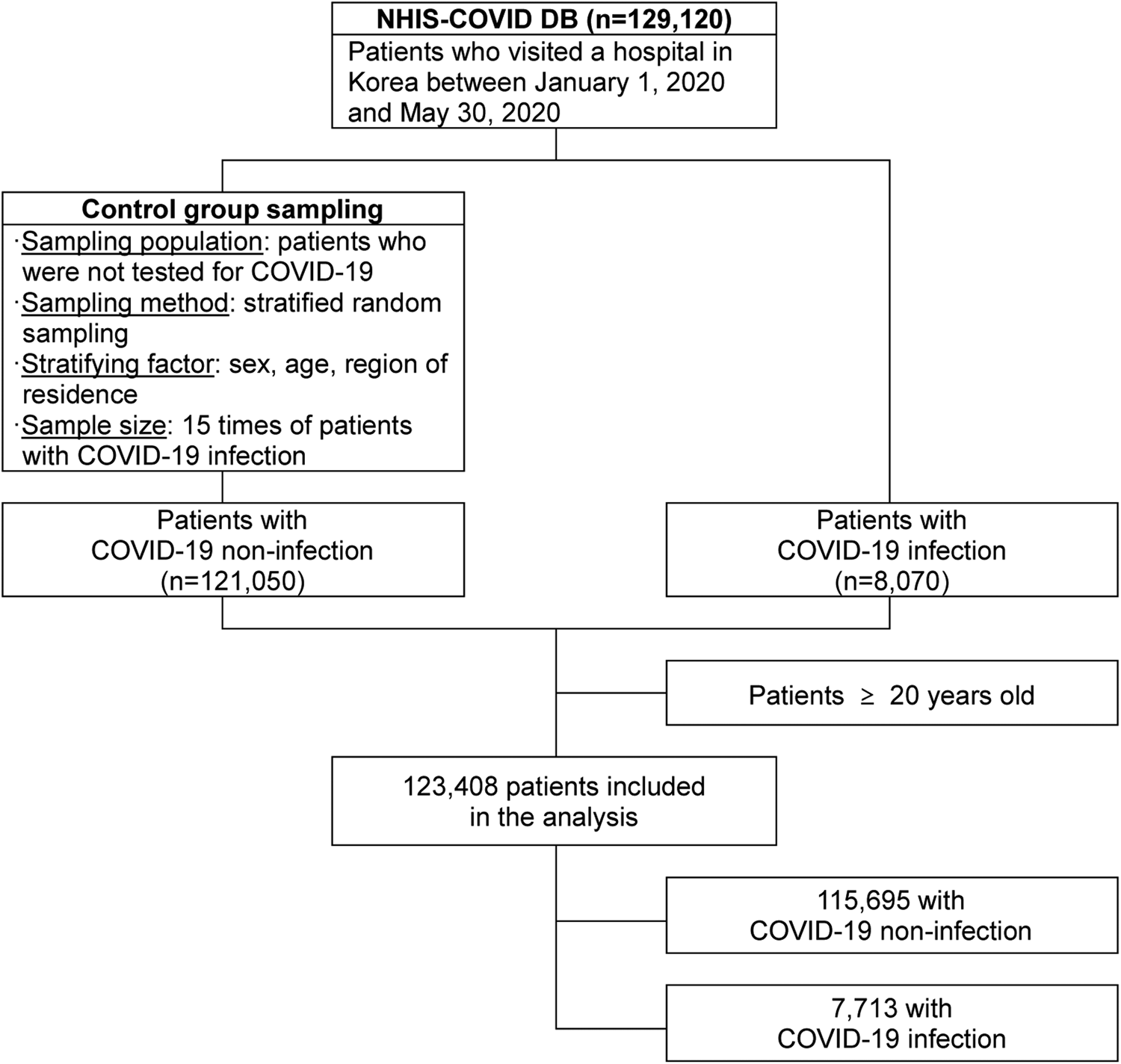
Fig. 1. Flow chart for patients included in the analysis
In this study, a patient with mental illness was defined as a patient diagnosed with a mental illness as the primary diagnosis in 2019. The International Statistical Classification of Diseases (ICD-10) code corresponding to a mental illness is ‘F00–F99 (mental and behavioural disorders)’. Patients who visited an outpatient clinic at least three times for the same main diagnosis or were admitted to a hospital at least once were considered to have a mental illness. Patients with schizophrenia (F20–29) and bipolar disorder (F30, F31, F38, F39) were classified as having a severe mental illness. These patients were further divided into depression disorder (F32, F33, F34), dementia (F00, F01, F02, F03), substance use disorder (SUD) (F10–19), and anxiety and obsessive-compulsive disorder (F40, F41, F42) groups according to the type of their mental illness.
Statistical analysis
We compared the characteristics of patients according to SARS-CoV-2 infection and COVID-19-related death using a χ2 test. Patient characteristics, current history, and type of mental illness, sex, age, region of residence, insurance cost and Charlson Comorbidity Index (CCI) scores were considered. Patients were categorised according to their age at 10-year intervals. For the region of residence, cities where a large number of confirmed cases had been reported, including Seoul, Daegu, Gyeonggi-do, Gyeongsang-buk-do and others, were considered. Since insurance costs are proportional to income in South Korea, insurance premiums were used as a marker of financial status. Medical aid recipients are low-income individuals who are exempt from health insurance payments. Patients who paid for health insurance were divided into the 1st (lowest), 2nd, 3rd, 4th and 5th (highest) quintiles according to their insurance costs. CCI scores represent the severity of comorbidities. Updated weights proposed by Quan et al. based on medical records from 2019 were applied to the scores (Quan et al., Reference Quan, Li, Couris, Fushimi, Graham, Hider, Januel and Sundararajan2011).
Logistic regression analysis was performed to investigate the risk of SARS-CoV-2 infection and COVID-19-related deaths in patients with mental illness. The primary outcome was the SARS-CoV-2 infection. The odds ratios (ORs) were calculated using logistic regression analysis to analyse the risk of COVID-19 according to the mental illness diagnosis and type. Additionally, a multivariate logistic regression model was created with insurance premiums and CCI scores as independent variables to adjust the ORs. Since the model was adjusted for sex, age and region of residence during the control group sampling, these variables were not included as confounding variables.
The secondary outcome was COVID-19-related death. A multivariate logistic regression model adjusted for sex, age, the region of residence and insurance premiums; CCI score was used to calculate the OR for COVID-19 in patients with mental illness. SAS 9.4 was used for statistical analyses with the level of statistical significance set to p-value <0.05.
Ethics statement
This study conformed to the Guidelines on De-identification of Personal Data of Korea and was approved by the Kyung Hee University's Institutional Review Board (IRB No. KHSIRB-20-301(EA)) as a review exemption study. As the study used de-identified data, the requirement for informed consent was waived by the board.
Results
Patient characteristics
To compare the risks of SARS-CoV-2 infection and COVID-19-related death according to patient characteristics, a χ 2 test was performed with sex, age, the region of residence, health insurance premium, CCI score and mental illness as the independent variables (Table 1). Uninfected people in the NHIS-COVID DB were stratified 15-fold and sampled such that their sex, age and region of residence distributions matched those of those infected with SARS-CoV-2. This allowed for the equalisation of the sex, age and region of residence distributions between the infected and uninfected groups. However, significant differences in SARS-CoV-2 infection were found according to health insurance premiums, CCI scores and mental illness. People with SARS-CoV-2 infection were higher in the low-income group, and non-infected people were higher in the high-income group. In the case of high CCI and people with mental illness, column percentages of people with SARS-CoV-2 infection were higher. A χ 2 test was used to assess the statistical significance of differences in COVID-19-related death rates according to sex, age, region of residence, health insurance premiums, CCI scores and mental illness (p < 0.001). As reported in Table 2, a χ 2 test was performed to examine the association between the type of mental illness and SARS-CoV-2 infection risk, as well as the association between the type of mental illness and COVID-19-related mortality. Severe mental illnesses (schizophrenia and bipolar disorder), dementia, anxiety, obsessive-compulsive disorder and SUDs were found to be significantly associated with SARS-CoV-2 infection. Severe mental illness, depression and dementia were all significantly associated with COVID-19-related mortality, and the rate of COVID-19-related death was higher among patients with these disorders than among those without.
Table 1. Patients baseline characteristics
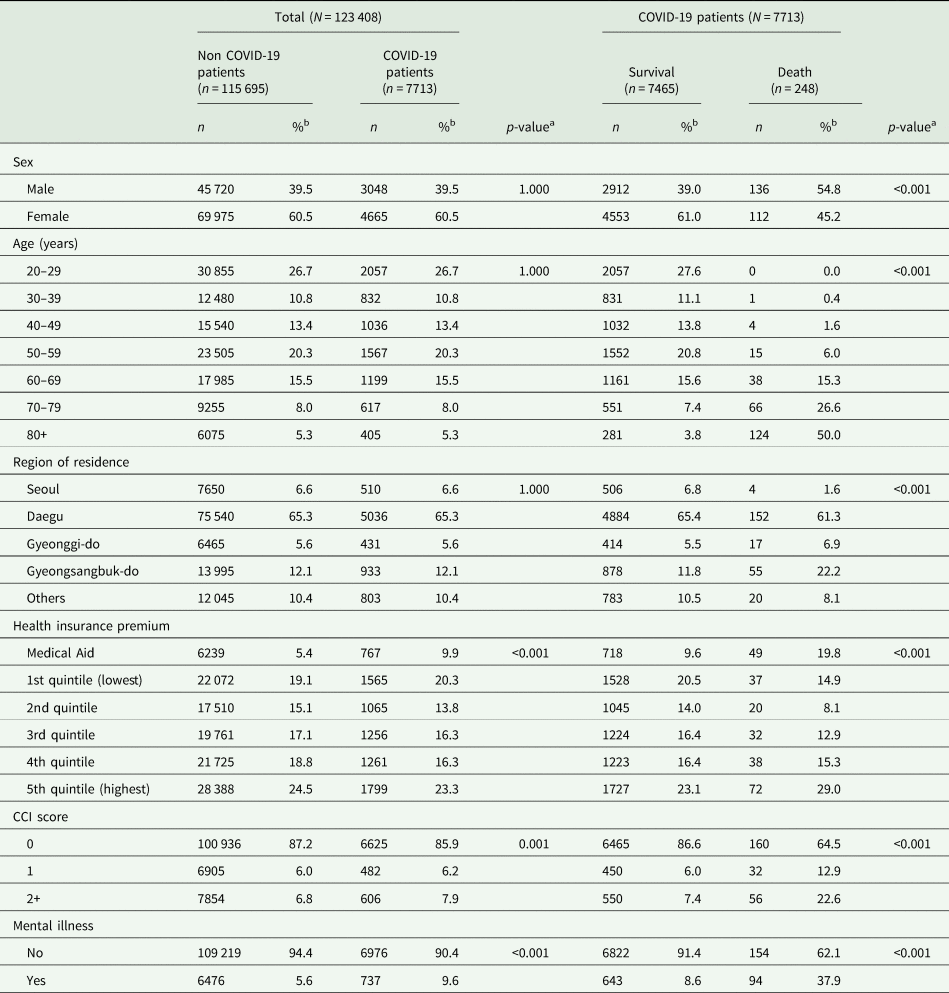
COVID-19, Coronavirus Disease 2019; CCI, Charlson Comorbidity Index, Mental illness (F00–F99).
a p-value for χ 2 test.
b % is column percentages
Table 2. Comparison of SARS-CoV-2 infection rate and COVID-19 mortality by types of mental illness
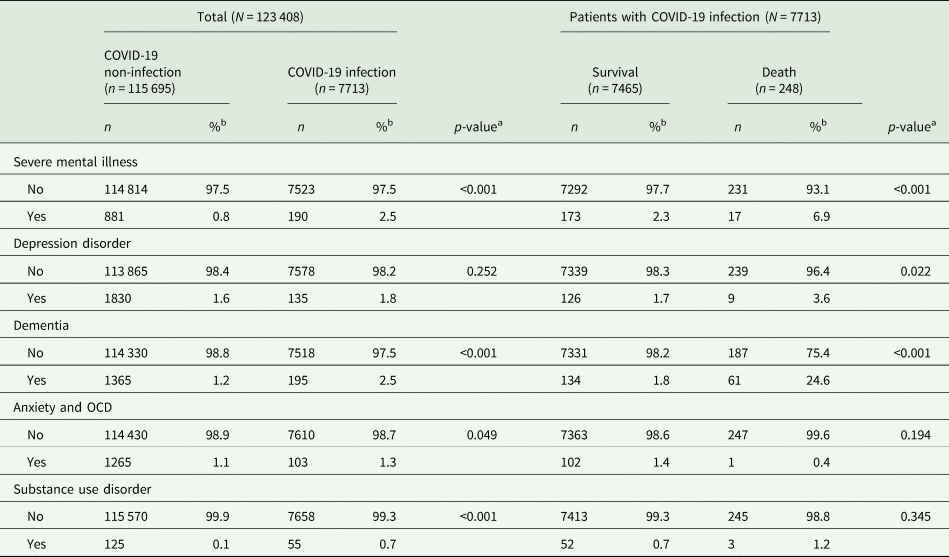
COVID-19, Coronavirus Disease 2019; OCD, Obsessive-Compulsive disorder.
Severe mental illness (F20-F29, F30, F31, F38, F39), Depression disorder (F32, F33, F34), Dementia (F00, F01, F02, F03), Anxiety and obsessive-compulsive disorder (F40, F41, F42), Substance use disorder (F10–F19).
a p-value for χ 2 test.
b % is column percentages.
Analysis for risk of COVID-19 infection and death by mental illness severity
Logistic regression analysis was performed to analyse the risks of SARS-CoV-2 infection and COVID-19-related deaths in patients with mental illness (Table 3). Statistical significance in the risk of SARS-CoV-2 infection was found according to health insurance premiums, CCI scores and mental illness. Medical aids were less likely to be infected by SARS-CoV-2 compared to those with health insurance, and SARS-CoV-2 infection risk increased as CCI scores increased. No statistically significant difference in the SARS-CoV-2 infection risk was found between patients with CCI scores of 0 and those with CCI scores of 1. The OR for SARS-CoV-2 infection was high (1.10) for patients with CCI scores of ⩾2 (95% CI 1.01–1.20, p-value = 0.032), showing a high risk of SARS-CoV-2 infection. The OR for SARS-CoV-2 infection in patients with mental illness was 1.58 (95% CI 1.45–1.71, p-value < 0.001). Thus, patients with mental illness were found to be at a high risk of SARS-CoV-2 infection.
Table 3. Odds ratio for risk of SARS-CoV-2 infection and COVID-19 death
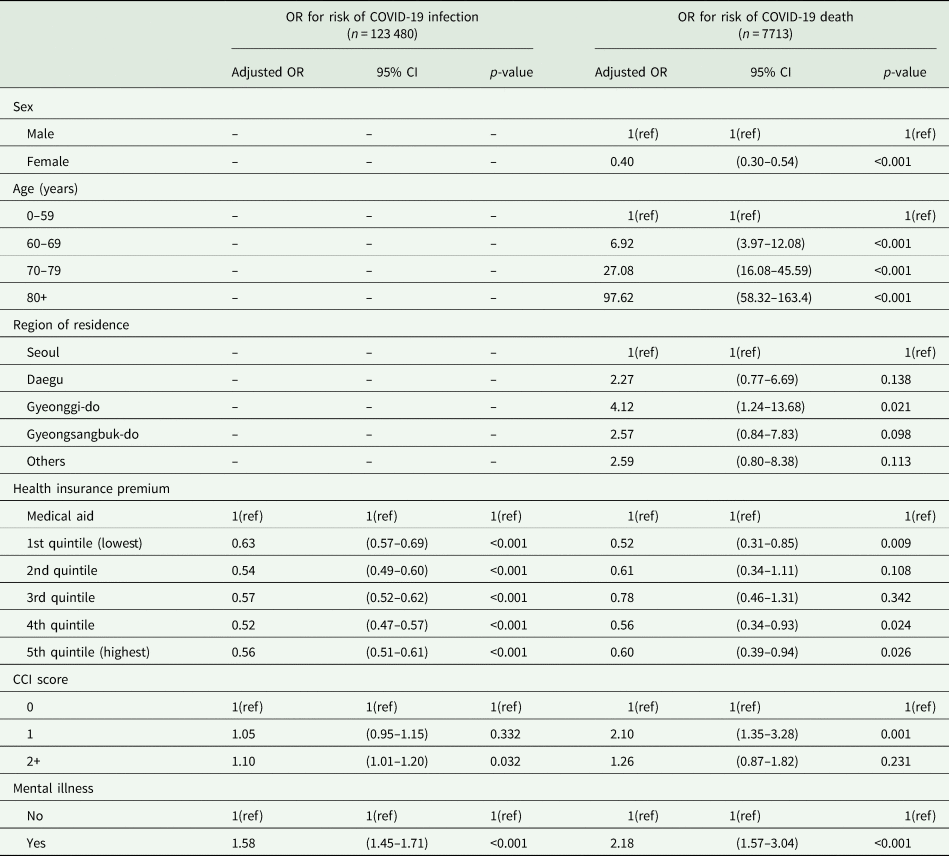
OR, Odds Ratio; CI, Confidence Interval; CCI, Charlson Comorbidity Index.
Mental illness (F00–F99).
Significant differences in COVID-19-related death rates were found according to sex, age, region of residence, health insurance premiums, CCI score and mental illness. The risk of COVID-19-related death was lower for women (OR 0.40, 95% CI 0.30–0.54, p-value < 0.001) and increased with age. A statistical difference in the risk of COVID-19-related death was found between Seoul and Gyeonggi-do (OR 4.12; 95% CI 1.24–13.68, p-value = 0.021). The risk of COVID-19-related death was higher in Gyeonggi-do than in Seoul. Among patients with health insurance, those in the 1st quintile (OR 0.52, 95% CI 0.31–0.85, p-value = 0.009), 4th quintile (OR 0.56, 95% CI 0.34–0.93, p-value = 0.024) and 5th quintile (OR 0.60, 95% CI 0.39–0.94, p-value = 0.026) showed significant differences in COVID-19-related mortality risk. The risk of COVID-19-related death was relatively low in patients with health insurance compared to those receiving medical aid. Patients with CCI scores of 1 (OR 2.10, 95% CI 1.35–3.28, p-value = 0.001) were at a higher risk of COVID-19 than those with CCI scores of 0. The OR for COVID-19-related death in patients with mental illness was high at 2.18 (95% CI 1.57–3.04, p-value < 0.001), showing that patients with mental illness had a higher risk of COVID-19-related death.
Based on the results presented in Table 3, the SARS-CoV2 infection and COVID-19-related death risks were further examined. An additional logistic regression analysis was performed to analyse the risks according to the type of mental illness (Fig. 2). A model for estimating the SARS-CoV-2 infection risk was adjusted for health insurance premiums and CCI scores and used to calculate the risk OR for each type of mental illness. Statistical significance in SARS-CoV-2 infection risk was found according to severe mental illness (OR 2.60, 95% CI 2.21–3.06, p-value < 0.001), dementia (OR 1.90, 95% CI 1.62–2.22, p-value < 0.001) and SUD (OR 4.98, 95% CI 3.60–6.88, p-value < 0.001). Patients with these disorders were at a higher COVID-19 infection risk than those without.
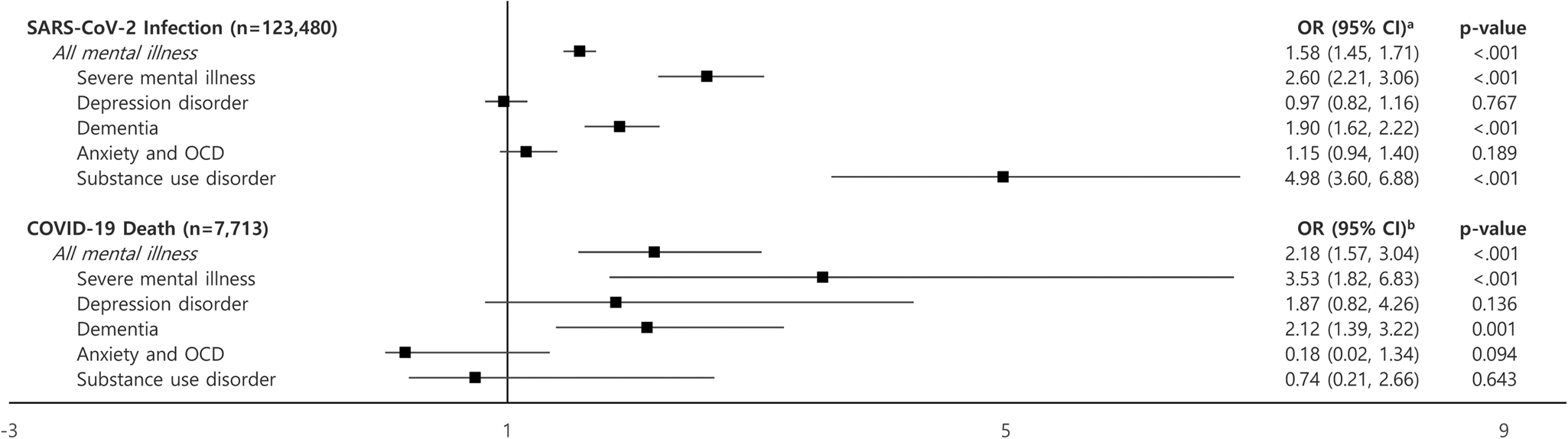
Fig. 2. Odds ratio for risk of SARS-CoV-2 infection and COVID-19 death by types of mental illness. aAdjusted for health insurance premium, Charlson Comorbidity Index score. bAdjusted for sex, age, region of residence, health insurance premium, Charlson Comorbidity Index score. COVID-19, coronavirus disease 2019; OCD, obsessive-compulsive disorder; OR, odds ratio; CI, confidence interval. Severe mental illness (F20–F29, F30, F31, F38, F39), depression disorder (F32, F33, F34), dementia (F00, F01, F02, F03), anxiety and obsessive-compulsive disorder (F40, F41, F42), substance use disorder (F10–F19).
A model for estimating the risk of COVID-19-related death was adjusted for sex, age, the region of residence, health insurance premiums and CCI scores, and was used to calculate the OR for each type of mental illness. Statistical significance in the risk of COVID-19-related death was found according to severe mental illness (OR 3.53, 95% CI 1.82–6.83, p-value = 0.009) and dementia (OR 2.12, 95% CI 1.39–3.22, p-value < 0.001). Patients with these mental illnesses were at a higher risk of dying from COVID-19 than those without.
Discussion
In this study, we analysed SARS-CoV-2 infection and COVID-19-related death risks in patients with mental illness. Our analysis showed a higher risk of SARS-CoV-2 infection and COVID-19-related death in patients with mental illness, as well as differences according to the type of mental illness. Patients with severe mental illness or dementia were at a higher risk of SARS-CoV-2 infection and COVID-19-related death than those without. Patients with SUD were at a higher risk of SARS-CoV-2 infection and COVID-19-related death than those without. No significant difference in COVID-19-related mortality risk was found between patients with and without SUD.
A previous study analysing a national dataset from the USA found that patients with mental illness were at high risk of SARS-CoV-2 infection and those that were infected had poor COVID-19 outcomes (Wang et al., Reference Wang, Xu and Volkow2021a). This study analysed SARS-CoV-2 infection risk in patients with attention deficit hyperactivity disorder, bipolar disorder, depression and schizophrenia, and found that SARS-CoV-2 infection risk was high for all mental illnesses (Wang et al., Reference Wang, Xu and Volkow2021a). Additionally, the study found that the rate of hospitalisation due to COVID-19 was higher in patients with mental illness than in those without (Wang et al., Reference Wang, Xu and Volkow2021a). These results were similar to those of the present study. On the other hand, studies analysing data from the Health Insurance Review and Assessment Service (HIRA) found no significant difference in SARS-CoV-2 infection risk in patients with mental illness, but observed that COVID-19 patients with a mental illness were at a higher risk of symptom severity and death (Lee et al., Reference Lee, Yang, Moon, Yoo, Ha, Kim, Park, Choi, Lee, Ahn, Kim, Koh and Yon2020; Jeon et al., Reference Jeon, Kwon, Park and Shin2021). Nevertheless, the reason why these studies did not observe a significantly high risk of SARS-CoV-2 infection in patients with mental illness may be attributed to the fact that the infection risk for SARS-CoV-2 was compared between those with and without mental illness. In our study, we obtained more accurate results by comparing patients who did not undergo the SARS-CoV-2 test.
The high risk of SARS-CoV-2 infection in patients with mental illness can be attributed to their living environment (Adhanom Ghebreyesus, Reference Adhanom Ghebreyesus2020). Patients with mental illness regularly visit a medical facility for outpatient treatment or reside in long-term care facilities. The WHO raised the need for infection prevention and control activities within long-term care facilities because of the high density of resident populations in these facilities (WHO, 2020b). Patients with mental illness may be especially susceptible to SARS-CoV-2 infection because they are protected from isolation during their socialisation therapy and come into close contact with staff members (Benson et al., Reference Benson, Öngür and Hsu2020).
The significant association between severe mental illnesses (schizophrenia, bipolar disorder) and SARS-CoV2 infection risk is explained by the cognitive deterioration and consequential behavioural changes that occur in individuals with these illnesses. Patients with a severe mental illness have lower levels of education and health literacy compared to the general population (Isohanni et al., Reference Isohanni, Jones, Järvelin, Nieminen, Rantakallio, Jokelainen, Croudace and Isohanni2001; Tempelaar et al., Reference Tempelaar, Termorshuizen, MacCabe, Boks and Kahn2017; Kim et al., Reference Kim, Park, Jhon, Kim, Lee, Kim, Kim, Shin and Yoon2019) and, thus, may lack COVID-19-related knowledge and prevention awareness. Muruganandam et al. conducted a questionnaire survey and interviews on COVID-19 symptoms and precautions among patients with severe mental illness who were clinically stable and found that these patients did not have sufficient COVID-19 awareness (Muruganandam et al., Reference Muruganandam, Neelamegam, Menon, Alexander and Chaturvedic2020). A study conducted in the UK found that the rate of SARS-CoV-2 infection was 38% (131/344) among older adults aged ⩾65 years or patients with dementia admitted to five London mental health NHS Trusts and reported that these groups were at a higher risk of infection than the general population (Livingston et al., Reference Livingston, Rostamipour, Gallagher, Kalafatis, Shastri, Huzzey, Liu, Sommerlad and Marston2020). Patients with dementia are at high risk of SARS-CoV-2 infection as they have difficulty maintaining a physical distance from others (Li, Reference Li2020) and their behaviour changes because of cognitive deterioration as their mental illness progresses. An American study examining COVID-19 diagnosis risk in patients with an SUD conjectured that the pharmacologic effects of drug abuse promote SARS-CoV-2 infection and increase the risk of side effects (Wang et al., Reference Wang, Kaelber, Xu and Volkow2021b). Patients with mental illness infected with SARS-CoV-2 were at a high risk of death because of their severe medical conditions and failure to receive appropriate, timely treatment. It is widely accepted that patients with mental illness have unhealthy lifestyles (Scott and Happell, Reference Scott and Happell2011; Bartlem et al., Reference Bartlem, Bowman, Bailey, Freund, Wye, Lecathelinais, McElwaine, Campbell, Gillham and Wiggers2015), which induces NCDs and increases the severity of SARS-CoV-2 symptoms due to complications (Hamer et al., Reference Hamer, Kivimaki, Gale and Batty2020). Furthermore, patients with mental illness fear the social stigma around a COVID-19-positive status as they do not perceive physical symptoms and pain well (Strauss et al., Reference Strauss, Spitzer and Muskin1990; Iancu et al., Reference Iancu, Strous, Poreh, Kotler and Chelben2005; Stubbs et al., Reference Stubbs, Thompson, Acaster, Vancampfort, Gaughran and Correll2015) and are sensitive to stress (Chang et al., Reference Chang, Strong, Pakpour, Griffiths and Lin2020). These characteristics of patients with mental illness cause them to postpone appropriate treatment, consequently increasing COVID-19-related mortality rates.
Patients with a severe mental illness are at a high risk of respiratory diseases such as pneumonia, which are not only caused by smoking but are also associated with antipsychotic medications (Dzahini et al., Reference Dzahini, Singh, Taylor and Haddad2018; Haga et al., Reference Haga, Ito, Sakashita, Iguchi, Ono and Tatsumi2018). Respiratory diseases are comorbidities that increase the risk of COVID-19-related death (Williamson et al., Reference Williamson, Walker, Bhaskaran, Bacon, Bates, Morton, Curtis, Mehrkar, Evans, Inglesby, Cockburn, McDonald, MacKenna, Tomlinson, Douglas, Rentsch, Mathur, Wong, Grieve, Harrison, Forbes, Schultze, Croker, Parry, Hester, Harper, Perera, Evans, Smeeth and Goldacre2020), and it may be that patients with severe mental illness are at risk of COVID-19-related death. In addition, the risk of COVID-19-related deaths in patients with underlying diseases such as cardiovascular disease (Kwenandar et al., Reference Kwenandar, Japar, Damay, Hariyanto, Tanaka, Lugito and Kurniawan2020), Parkinson's disease (Putri et al., Reference Putri, Hariyanto, Hananto, Christian, Situmeang and Kurniawan2021) and HIV (Hariyanto et al., Reference Hariyanto, Rosalind, Christian and Kurniawan2021) is high, which indicates that patients with mental illness with several comorbidities may have higher risk of mortality. Most patients with dementia are of advanced age and vulnerable to COVID-19-related deaths. In their systematic literature review, Hariyanto et al. observed high COVID-19 severity and mortality in patients with dementia and mentioned the importance of the medical management of these patients (Hariyanto et al., Reference Hariyanto, Putri, Arisa, Situmeang and Kurniawan2020).
For the reasons discussed above, patients with mental disorders should be prioritised for vaccination due to their high risk of SARS-CoV-2 infection and COVID-19-related deaths (Warren et al., Reference Warren, Kisely and Siskind2020; De Picker et al., Reference De Picker, Dias, Benros, Vai, Branchi, Benedetti, Borsini, Leza, Kärkkäinen, Männikkö, Pariante, Sönmez Güngör, Szczegielniak, Tamouza, van der Markt, Fusar-Poli, Beezhold and Leboyer2021). In addition, the patients’ caregivers should also be prioritised because of the high risk of external contact causing group infection within residential facilities for people with mental disorders (Halley and Mangurian, Reference Halley and Mangurian2021; Woodfield et al., Reference Woodfield, Pergam and Shah2021).
This study had several limitations. First, we defined patients with mental illness and CCI scores based on ICD-10 codes from the health insurance claims data. However, the sensitivity of diagnoses can vary across diseases because of the nature of administrative data (Wilchesky et al., Reference Wilchesky, Tamblyn and Huang2004). We tried to overcome this limitation by conservatively defining patients with mental illnesses. Second, while we investigated SARS-CoV-2 infection risk and COVID-19-related death rates after classifying mental illnesses based on major diagnosis codes, we could not account for the clinical severity of individual mental illnesses. Third, SARS-CoV-2 infection risks and COVID-19-related death rates were examined according to clinical characteristics and may have been overestimated as they were measured without separating the effect of the patients’ use of hospital services. As mentioned earlier, while patients with mental illness use hospital services, it is still necessary to measure SARS-CoV-2 infection risk and COVID-19-related death rates in community facilities. Further research on mass infection risk in long-term care facilities is needed. Despite these limitations, this study derived meaningful results regarding the risk of SARS-CoV-2 infection and COVID-19-related death using a national dataset from South Korea. We reasonably defined the control group and created a statistical model that considered the patient's financial status. We found that patients with mental illness were vulnerable to COVID-19 and presented evidence supporting the need to intervene specifically with this patient population.
In conclusion, patients with mental illness have a higher risk of SARS-CoV-2 infection and COVID-19-related death. Cognitive deterioration and living environments susceptible to SARS-CoV-2 infection increase infection rates, while severe medical conditions and delayed treatment increase COVID-19-related mortality in patients with mental illness. Patients with mental illness are a priority target for COVID-19 prevention and treatment, and it is important to plan prevention measures for this patient group.
Data
The datasets used during the current study are available from the national health insurance service on reasonable request.
Financial support
The author(s) received no financial support for the research, authorship and/or publication of this article.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.









