LEARNING OBJECTIVES
After reading this article you will be able to:
• recognise the importance of values, context, ways of working and purposes (such as clinical versus research) in deciding which classification systems should be used in mental health practice
• describe the strengths and weaknesses of the DSM and ICD compared with the dimensional unitary psychosis classification system
• demonstrate understanding of the clinical utility of combining categorical and dimensional systems and adding biopsychosocial aetiological information.
Before discussing the optimum classification for psychosis, it is necessary to briefly discuss the values involved, the contexts in which these suggestions are made, the purposes for which the classification will be used, and the historical background of neo-Kraepelinian and unitary psychosis classification. Reviews of psychosis classification usually omit much of this important information, meaning that their suggestions are made from the point of view of their own unstated values, purposes and contexts, assuming (often incorrectly) that they match those of the reader. This article is intended to be of benefit to clinically focused (as opposed to research focused) mental health professionals who are assumed to work in contexts similar to those described below.
Values and contexts
The role of values in the creation of psychiatric classification systems is increasingly recognised. In the DSM, the important ontological values of empiricism, hyponarrativity (with a converse emphasis on the nomothetic approach), individualism, naturalism, pragmatism and traditionalism were identified (Sadler Reference Sadler2005). The proposed classification outlined below will emphasise the values of empiricism and pragmatism, along with the nomothetic approach. The DSM diagnostic approach relies on the similarity between cases given the same diagnosis (nomothetic approach) instead of the unique attributes of each case, such as their life story (hyponarrativity). Hyponarrativity and individualism will be less emphasised, as we propose the inclusion of biopsychosocial contextual factors to give an understanding of how individual cases of psychosis are often related to broader contextual factors and encourage the classification to be used alongside an individualised formulation. Our focus on pragmatism recognises that diagnostic categories are used pragmatically in general medicine, as well as in psychiatry, for conditions that often do not exist as neat categories (i.e. entities that are clearly separate from each other and from healthy states), such as hypertension or connective tissue disorders (Huda Reference Huda2019). This article will discuss whether the traditional Kraepelinian classification should be discarded completely.
The perennial debate over whether to use dimensions or categories often omits the important contextual information of the situations in which they are used. Mental health problems can be represented either as categories or dimensions (Kraemer Reference Kraemer, Noda and O'Hara2004). Dimensions are preferable to researchers and those clinicians who see few patients for long appointments in non-urgent situations, whereas clinicians who work in urgent situations or see many patients for short periods, and researchers conducting studies to provide useful information for such clinicians, tend to prefer categories (Kraemer Reference Kraemer, Noda and O'Hara2004).
The contextual use of diagnosis in psychiatry based on the most common methods of practice in the UK has been discussed elsewhere (Huda Reference Huda2019). Clinical psychiatrists tend to have large case-loads in the hundreds and see patients for brief appointments often with weeks or months between appointments. This, combined with a tendency to see patients in emergencies, including at night and at the weekend, leads to favouring the use of categorical diagnostic classifications because of the economy of cognitive resources. Clinical practice often involves dichotomous decisions, such as whether to treat or not, which again favours categorical approaches (Kraemer Reference Kraemer, Noda and O'Hara2004).
Purpose of classification
Clinicians use classification because of its administrative and clinical utility (First Reference First, Rebello and Keeley2018). The clinical utility of diagnostic classifications has been defined as the extent to which they guide how clinical problems are conceptualised, allow colleagues to communicate effectively with one another about the nature of patients’ problems, aid the assessment of those problems and allow information to be extrapolated from research to individual patients to best guide clinical decision-making (First Reference First, Pincus and Levine2004). The clinically useful information attached to a diagnosis includes the associated clinical picture, aetiology (if known), prognosis, treatment response, complications, co-occurring conditions and differential diagnosis (First Reference First, Pincus and Levine2004; Huda Reference Huda2019). The research utility of classification includes being able to gain clinically useful information, as well as facilitating research hypotheses about biological, psychological or social correlates to discover the causes and mechanisms of patients’ problems (Kendell Reference Kendell and Jablensky2003). Diagnostic systems such as the DSM explicitly favour clinical utility (and implicitly in the context of the way most psychiatrists work) over research utility (McIntyre Reference McIntyre, Yager and Everett2021).
History of classification of psychosis
Psychosis came to be separated from delirium, dementia and neuroses during the 19th century (Berrios Reference Berrios1996). This was a period of flux in medical classifications of conditions and its extension into psychiatry (Berrios Reference Berrios and Beer1994). Earlier classification systems – such as symptoms being regarded as disease entities in their own right – were being discarded in favour of those in which symptoms and signs were correlated with causative anatomical lesions. In most cases of psychosis these lesions proved elusive, so other classification principles were suggested, such as covariance of symptoms and outcomes.
A belief that classifying subtypes of psychosis lacked validity and utility (a recurrent theme to this day) led to the emergence of unitary psychosis advocates in Germany in the 19th century (Berrios Reference Berrios and Beer1994). These proponents of the notion of unitary psychosis believed that symptomatic variations were related to differences between individual vulnerabilities and external factors (such as culture and life experiences), so did not reflect separate conditions and they often postulated a common biological or psychological cause. Some – such as Wilhelm Griesinger – regarded psychosis as a stage in progressive deterioration from mood disorder to psychosis then dementia, with dementia as an inevitable result (Berrios Reference Berrios1996). Their classification systems raised as many questions as they answered, such as when people's environments and triggering events change why do psychotic symptoms remain relatively constant between psychotic episodes (Berrios Reference Berrios and Beer1994)? Revivals of unitary psychosis concepts have occurred in the late 20th century for various reasons, such as failure of statistical methods to clearly separate psychosis constructs based on symptoms or evidence of shared genetic vulnerabilities (Berrios Reference Berrios and Beer1994).
The most well-known subtyping of psychosis was created by Emil Kraepelin based on observations of asylum patients, often the most severe cases. He separated psychosis into two types with overlapping symptom profiles but distinct courses (Berrios Reference Berrios and Beer1994, 1996). Psychosis with a remitting relapsing course but with good inter-episode function he called manic–depressive psychosis and psychosis with progressive deterioration was named dementia praecox. He believed that different prognoses reflected different disease pathways. He later admitted that this division was premature, and many cases fell into intermediate prognostic categories (Berrios Reference Berrios and Beer1994). Despite these misgivings, this division consequently formed the basis of the current neo-Kraepelinian diagnostic system of DSM-5 and ICD-11, in which bipolar I disorder (categorised among the mood disorders) and affective psychosis (labelled schizoaffective disorder and categorised among schizophrenia spectrum and other psychotic disorders) replace manic–depressive psychosis; and non-affective psychosis (labelled schizophrenia) replaces dementia praecox and the intermediate prognostic categories. Most of the research into psychosis that will be used as an evidence base for clinical decision-making – such as aetiology, prognosis and treatment response – is based on these, or related, categories.
Leonhard – who was important in the development of the distinction between unitary psychosis and bipolar (affective) disorder – suggested a psychosis with good prognosis called ‘cycloid psychosis’, a concept based on the work of Kleist (Leonhard Reference Leonhard1961) This was a ‘phasic’ (i.e. episodic) form of psychosis but it was distinguished from bipolar affective disorder by three dimensions of clinical features that can all be present to varying degrees in the same case: anxiety–elation, confusion–inhibition of thought and akinetic–hyperkinetic behaviour.
DSM/ICD classification of psychosis
In clinical practice, distinguishing between psychosis due to substance intoxication/withdrawal or secondary to general medical conditions, brief psychosis, episodic psychosis as part of a coexisting mood disorder, and chronic psychosis is essential. This is required not only because of the aetiological mechanisms, but also because of attendant differences in clinical management (Frances Reference Frances2016). A categorical diagnostic system captures these clinically useful differences better than the unitary psychosis model, which by its unitary nature will minimise any differences between different forms of psychosis.
Diagnosis in clinical practice usually involves matching the information obtained from assessing the patient and other data (such as informant history and investigations) to the closest matching diagnosis using a mixture of prototype recognition and attempts to confirm or deny the initial diagnostic hypothesis (Huda Reference Huda2019). These prototypes consist of central typical examples, with increasingly dissimilar examples away from this central archetype leading to overlapping borders with other prototypes (Parnas Reference Parnas2015).
Kraepelin himself noted overlapping symptom profiles between manic–depressive psychosis and dementia praecox (Berrios Reference Berrios1996). Modern research, with discriminant functional analysis of cross-sectional assessments of symptoms, has found no points of rarity between bipolar affective disorder type I (bipolar I disorder) and schizophrenia, but adding longitudinal data on illness course allowed some separation between the two (Jauhar Reference Jauhar, Krishnadas and Nour2018). Using machine learning analysis on data from a cohort of 214 patients, good accuracy rates (over 80%) of Present State Examination phenotypes distinguishing between later DSM-III diagnosis of affective psychosis and non-affective psychosis have been identified (Jauhar Reference Jauhar, Krishnadas and Nour2018). This indicates that despite some symptom overlap, it is often possible to distinguish bipolar disorder (and other affective psychotic conditions) from schizophrenia and related conditions, although there are cases that do not match either prototype. There is great symptomatic heterogeneity between cases given the same psychosis diagnosis, which may represent a challenge to the neo-Kraepelinian model.
DSM-IV and ICD-10 definitions of schizophrenia emphasise more easily assessed features, including delusions and hallucinations, which may result in many recurrent or chronic delusional and hallucinatory states being diagnosed as schizophrenia (Parnas Reference Parnas, Kendler and Parnas2012). The emphasis on easily assessed features continues in DSM-5 and ICD-11. This deviates from the European tradition of conceptualising the ‘core’ gestalt identity of schizophrenia as being the ‘hebephrenic’ subtype of disorganisation and negative symptoms (Parnas Reference Parnas, Kendler and Parnas2012). This expansion of the concept of schizophrenia to include all chronic recurrent non-affective psychoses loses the construct validity of the concept (Parnas Reference Parnas, Kendler and Parnas2012). It also increases disutility to patients, as many more are given the schizophrenia diagnosis – which continues to be heavily stigmatised – than is warranted (Crisp Reference Crisp, Gelder and Rix2000).
First-rank symptoms were used in clinical practice to differentiate schizophrenia from other psychotic disorders, but a systematic review of research estimated 58% sensitivity and 74.7% specificity for their use in this way (Soares-Weisser Reference Soares-Weiser, Maayan and Bergman2015) and they have lost this role in DSM-5 (American Psychiatric Association 2013) and ICD-11 (World Health Organization 2022). Phenotypic differences (but not clear distinctions) with prognostic significance include greater frequency of negative symptoms (Strauss Reference Strauss and Cohen2017) and cognitive impairment (Green Reference Green, Horan and Lee2019) in schizophrenia compared with other psychotic disorders, including bipolar I disorder. Jaspers regarded primary delusions (representative of the patient's attempt to convey to others their radically changed personal experience of reality) as the hallmark of schizophrenia (Jaspers Reference Jaspers, Hoenig and Hamilton1913). Profound disturbances of self-experience, known as disorders of self, have been empirically demonstrated to be more associated with the schizophrenia spectrum disorder (including non-psychotic schizotypal disorder) than with other mental health conditions, including other psychotic conditions (Parnas Reference Parnas and Henriksen2014), but these are rarely assessed in clinical practice and have little demonstrated prognostic value in isolation.
There is prognostic utility in differentiating schizophrenia from affective psychosis as there is a lower chance of recovery compared with affective psychosis (30.3% v. 84.6%) (Lally Reference Lally, Ajnakina and Stubbs2017). There is treatment utility in neo-Kraepelinian categories, given differential responses to mood stabilisers between schizophrenia and bipolar disorder, but some treatments, such as atypical antipsychotics, are useful in both. Identifying psychotic symptoms secondary to biological causes such as general medical conditions (e.g. delirium or hypothyroidism), head injuries, substance misuse and dementias has obvious aetiological, prognostic and treatment utility (David Reference David, Fleminger and Kopelman2009). These require to be classified separately from psychosis for which no clear biological cause is identified. These are often referred to as ‘organic’ psychosis, but the contrasting term ‘functional’ psychosis for when no such obvious cause is found is misleading as it implies no biological factors are involved in their aetiology.
Genetic factors and heritability
Two reviews of genetic factors include details of similarities and differences between schizophrenia and bipolar disorder (Legge Reference Legge, Santoro and Periyasamy2021; O'Connell Reference O'Connell and Coombes2021). Both are highly heritable conditions (h 2 ≃ 0.8) – but still involve important interactions with environmental factors – with much higher degrees of genetic correlation between each other (r g = 0.68−0.7) than other conditions, such as depression (r g = 0.34−0.36). Genome-wide association studies show that some single nucleotide polymorphisms increase the risk (individually to a fractional degree) for both conditions, but some only increase the risk for schizophrenia or bipolar disorder. Copy number variants are rarer, increase risk significantly if present and are usually associated with schizophrenia, but one also increases the risk for bipolar disorder. The evidence from genetic research so far indicates largely shared genetic factors between schizophrenia and bipolar disorder.
Heritability in this context is the estimated proportion of difference in risk of developing the condition between different individuals that is attributed to genetic factors, everything else being equal (such as exposure to environmental factors, including childhood trauma). It is different from the population attribution fraction, which identifies what proportion of cases of a condition are due at least in part to a particular risk factor. As an example, some people have higher genetic vulnerability for lung cancer but widespread cigarette smoking would be a greater influence on rates of lung cancer in a population than this genetic vulnerability. This means that high heritability does not necessarily mean that most cases of psychosis in the community are due to genetics, as environmental factors may be a more common cause of the condition.
The majority of genetic factors thought to be involved have not been demonstrated to exist (‘missing heritability’) and explanations for this include that the genes involved are still to be discovered or that either unidentified gene–gene interactions (epistasis) or environmental effects on genes (epigenetics) will be discovered to explain this missing heritability (Harrison Reference Harrison2015). Given that heritability is an estimate based on assumptions, it may be that the contribution of genetics has been overestimated and requires ongoing review.
Non-genetic biopsychosocial factors
An umbrella review identified several non-genetic biopsychosocial factors at least suggestively associated with increased risk for psychosis (Radua Reference Radua, Ramella-Cravaro and Ioannidis2018). These included ethnic minority/immigration status (especially second- and later-generation Black Caribbean ethnicity in England), lower premorbid IQ, minor physical anomalies, presence of toxoplasma IgG antibodies, trait anhedonia, childhood social withdrawal, urbanicity and childhood trauma. Risk factors were studied in both affective and non-affective psychosis.
A contemporary unitary psychosis model: the ‘extended psychosis phenotype’
DSM/ICD diagnostic categories can describe phenomenological prototypes that fit some (but not all) patients with psychosis well. They convey useful clinical information on prognosis and treatment despite being symptomatically heterogeneous with overlapping clinical features. Schizophrenia has been associated with some phenomenological differences, such as disorders of self. Cases of psychosis are aetiologically heterogeneous, so carry little certain information in their categories as to cause or mechanisms for each case except where a clear biological cause has been identified and named, such as psychosis caused by substances.
Given the high degree of overlapping aetiological factors and symptoms between different DSM/ICD psychosis diagnoses as outlined above, there has been renewed interest in the unitary psychosis concept, for which van Os & Reininghaus have prosed an elegant extended psychosis phenotype model (van Os Reference van Os and Reininghaus2016).
They define psychosis in this model as the presence of psychotic symptoms such as delusions and hallucinations and the model is based on their review of the research evidence, which is summarised as follows:
• psychotic symptoms are present in many psychiatric conditions, including anxiety and mild depression, not just in those regarded as psychotic disorders
• there are no valid boundaries between different diagnostic constructs of psychosis, such as those based on symptomatic differences
• there are similarities between subclinical psychotic experiences in the community and psychotic symptoms in people described as mentally ill
• symptom dimensions have shown superior prognostic ability compared with diagnoses (at the expense of cognitive economy)
• risk factors and cognitive deficits overlap between different diagnostic constructs of psychosis.
Psychosis is argued to be ideally described using dimensions of symptoms (specifically depression, mania, positive symptoms, disorganisation and negative symptoms), with particular patterns of symptom dimensions corresponding to DSM/ICD diagnosis. This unitary psychosis model extends from subclinical psychotic experiences to severe psychosis and is transdiagnostic across many psychiatric conditions where psychotic symptoms are present (van Os Reference van Os and Reininghaus2016).
This extended psychosis phenotype version of the unitary psychosis model proposes two complementary pathways of severity resulting from gene–environment interactions (van Os Reference van Os and Reininghaus2016). The first involves mood, anxiety and psychotic symptoms, which are greater in the presence of increased socio-environmental risk and are associated with poorer functioning. The second is a network of anxiety and mood symptoms that is increasingly activated by socio-environmental stressors leading to increased recruitment of affective and psychotic symptoms. This universal aetiological model (which risk factors can be plugged into) allows testable hypotheses to be researched. Although five dimensions seems an optimum number to represent psychosis symptoms, the nature and definition of these dimensions (such as whether to drop cognitive symptoms for mania) may not achieve a good fit in samples of patients with psychosis other than the ones they were generated from (van der Gaag Reference van der Gaag, Cuijpers and Hoffman2006). This may suggest that there is currently no valid universal dimensional model of psychosis.
Clinical and research utility of unitary psychosis models
Many cases of psychosis do not easily fit the neo-Kraepelinian phenotype of DSM/ICD in the early episodes of psychosis, as the patient's presenting phenotype may vary before ‘settling down’ into a final pattern (Heslin Reference Heslin, Lomas and Lappin2015). A unitary psychosis model has been recommended for early intervention in psychosis (EIP) services, partly because of this diagnostic instability but also for research utility reasons to allow research into the causes and mechanisms of psychosis (McGorry Reference McGorry, Killackey and Yung2008). Yet, the latter reason ignores that for most EIP teams (and for clinicians as a whole) clinical utility is far more important than research utility. Unfortunately, there are multiple clinical utility problems with this system, especially for psychiatrists.
Most research has been undertaken using the DSM, so if using unitary psychosis models one must make further degrees of inference to apply the research evidence for treatment and prognosis to the individual in the clinic. If cases are just defined by cross-sectional symptom dimensions, then this system does not easily distinguish between the important forms of psychosis described above (Frances Reference Frances2016). For example, psychotic symptoms caused by hallucinogenic drug intoxication may score similarly on symptom dimension ratings to symptoms due to a relapse of recurrent psychosis. Furthermore, there is a problem insomuch as an individual with recurrent psychosis who is currently well may be difficult to separate on cross-sectional symptom dimensional ratings from someone with no mental health problems or mild symptoms only. The aetiology, prognosis and management of these different situations are likely to be very different. The unitary psychosis model therefore still requires the use of DSM/ICD categories for dementias, substance-induced psychosis and so forth. The unitary psychosis model is then used when no obvious biological cause is found and to differentiate people with psychosis from those without mental health problems or an absence of psychotic symptoms. The unitary psychosis model applied in clinical practice may not indicate the differential responses to some treatments that bipolar disorder and schizophrenia do.
Another problem is that the stated phenomenological continuity between subclinical psychotic experiences and psychotic symptoms may be due to methodological errors in community surveys using blunt instruments (such as questionnaires) that generate false positives or interviews by clinically inexperienced raters that fail to identify key phenomenological differences apparent to experienced clinicians, such as preoccupation, functional impact and distress (David Reference David2010). The claim of phenomenological continuity across psychotic disorders is challenged by empirical evidence that disorders of self are significantly more common in schizophrenia spectrum conditions than in other psychotic conditions (Parnas Reference Parnas and Henriksen2014).
There may well be two broad types of psychosis (David Reference David2010) – excluding those cases with clearly identified biological causes – the first continuous with subclinical psychotic experiences and the second better described by neo-Kraepelinian diagnosis (until a superior classification is possible). The analogy of height may be useful – for most people, height lies on a continuum reflecting gene–environment interactions, but there are also people with extremes of height due to conditions such as achondroplasia. Further developments in our neuroscientific knowledge may help us identify cases of psychosis with newly discovered potential biological aetiology, such as psychosis linked to N-methyl-d-aspartate (NMDA) receptor antibodies and other autoimmune disorders (Pollak Reference Pollak, Lennox and Müller2020).
Summary
The unitary psychosis model describes some cases of psychosis well, represents cross-sectional symptom heterogeneity and makes clear that psychotic symptoms can occur in many conditions not regarded as psychotic. It is likely to have research utility, as many risk factors are shared across psychotic disorders. Its claim to be a universal model of psychosis is challenged by the poor quality of evidence for phenomenological continuity between subclinical psychotic experiences and psychotic illness and by phenomenological distinctions between psychotic disorders such as disorders of self in schizophrenia spectrum disorders. It does not adequately differentiate clinically important forms of psychosis such as psychosis with a clear biological cause; nor does it indicate important differences in response to medication between bipolar disorder and schizophrenia. There is no single valid dimensional representation of psychosis. There is also a paucity of directly relevant clinical research for psychiatrists using this model.
A new protocol for the classification of psychosis
Given that both DSM/ICD and unitary psychosis classifications seem to work well in describing different groups of patients, with DSM/ICD having greater clinical utility in those it describes well, we propose a diagnostic hierarchy to determine which should be applied (Fig. 1).
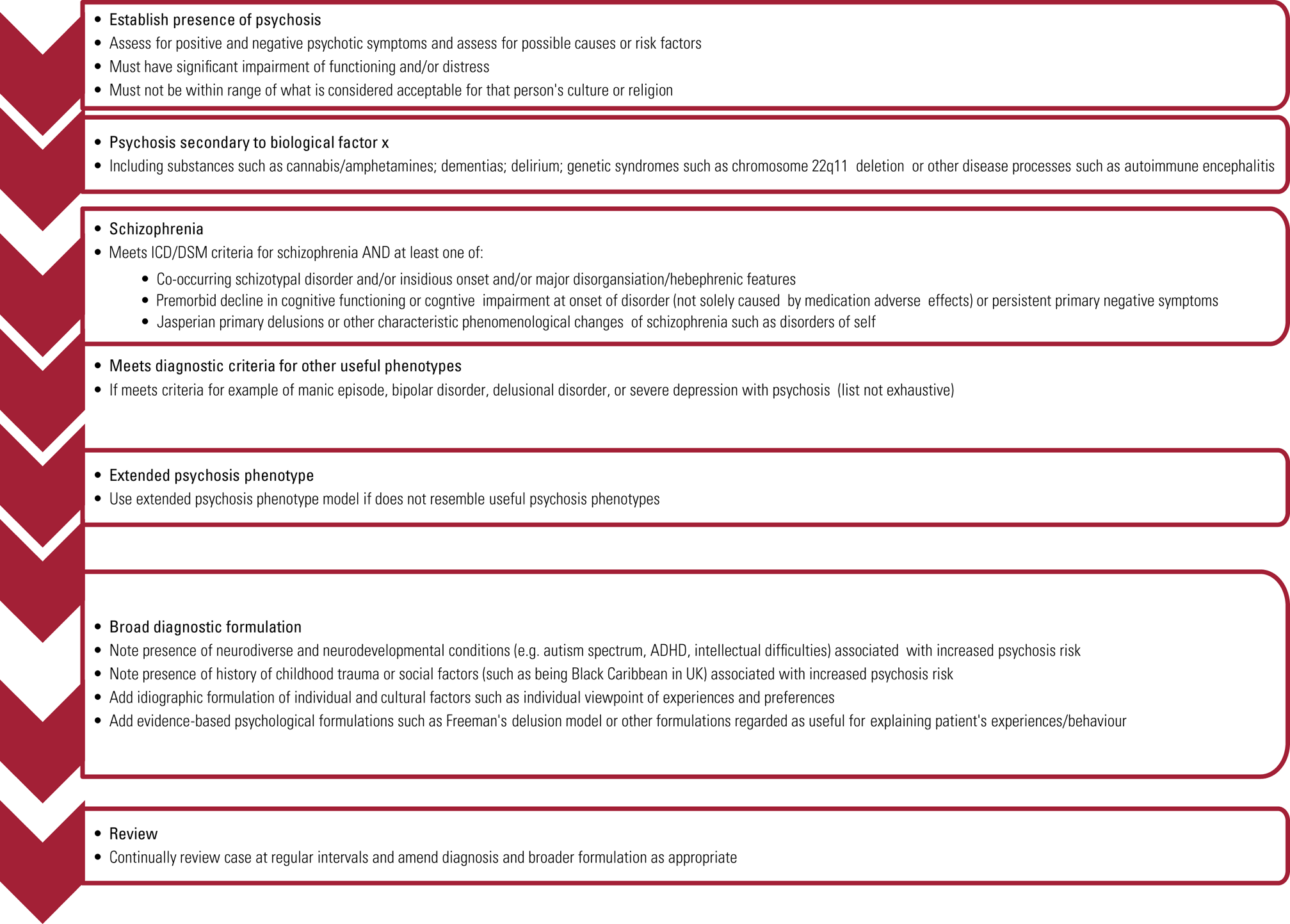
FIG 1 A diagnostic protocol for use in the diagnosis of psychosis.
During the initial stages of presentation to services, clinical focus should be on recognition and identification of the presence of positive, disorganised and negative psychotic symptoms. These features, viewed in the context of the individual's religious and cultural background, are critical in the diagnosis of psychosis. Subsequently, the clinician should be vigilant for, and investigate as indicated, any medical conditions, psychoactive substance use (David Reference David, Fleminger and Kopelman2009) or genetic alterations – such as copy number variants (Kirov Reference Kirov, Rees and Walters2015) identified as strongly associated causes of psychosis.
A diagnosis of schizophrenia should only be used for people who meet both the current diagnostic criteria and phenomenological features associated with schizophrenia (such as primary delusions or disorders of self), or primary negative symptoms, or clinically significant cognitive impairment that developed during the prodrome or onset of psychosis. This identifies individuals with either a phenomenologically distinct subtype of psychosis or those at higher risk (but no certainty) of worse outcomes (there is no assumption that disorders of self are associated with a worse prognosis).
If the patient's presentation is not well described by a DSM/ICD diagnosis, then a diagnosis of non-specific psychosis using the unitary psychosis extended phenotype model is used instead. All cases of psychosis should have symptom dimensional ratings as described in DSM-5 and ICD-11, as well as information on the course – such as first episode or recurrent – to improve descriptive and prognostic information.
The next step is to identify any co-occurring conditions that are important to consider in relation to clinical management and may benefit from additional interventions; examples may include (but are not limited to) substance use, post-traumatic stress disorder, cyclothymia, mild to moderate depression and complex trauma.
Finally, biopsychosocial risk factors associated with the development of psychosis (Radua Reference Radua, Ramella-Cravaro and Ioannidis2018) should be listed, such as childhood trauma or being Black Caribbean in the UK. This increased risk for Black Caribbean people in the UK does not appear to be based on genetic factors and there is increasing interest in socioeconomic factors that might explain this increased risk (Tortelli Reference Tortelli, Errazuriz and Croudace2015), which strongly indicates an environmental risk factor causing psychosis in this ethnic group. Neurodiverse conditions such as autism spectrum disorder (De Giorgi Reference De Giorgi, De Crescenzo and D'Alò2019) or attention-deficit hyperactivity disorder (ADHD) (Nourredine Reference Nourredine, Gerring and Fourneret2021) are associated with an increased risk of psychosis, possibly due to an overlap of genetic risk factors between autism spectrum disorder, ADHD, schizophrenia, bipolar disorder and depression (Cross-Disorder Group of the Psychiatric Genomics Consortium 2013). Identification of factors associated with increased risk improves the conceptualisation of how cases of psychosis arise both for the individual and aggregated at the community level, indicating how biopsychosocial factors lead to psychosis.
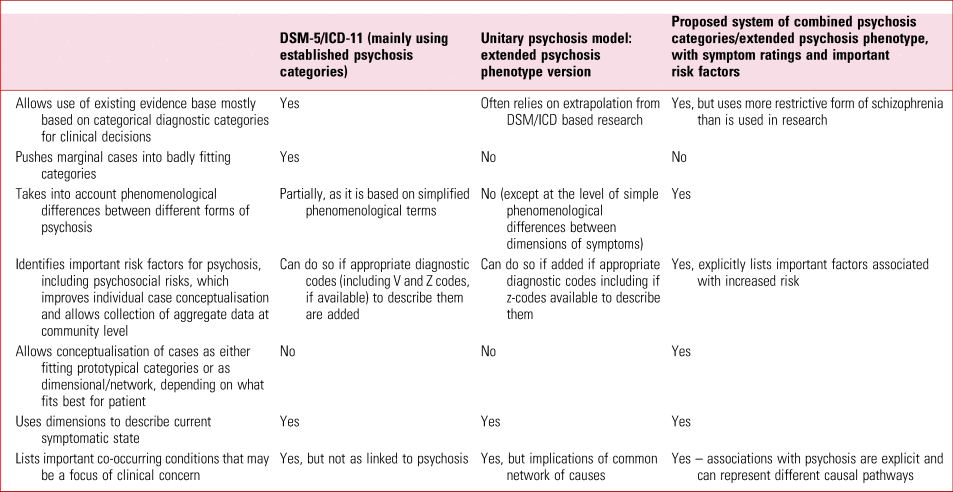
A comparison of the proposed system with that of the DSM/ICD system and the extended psychosis phenotype model can be found in Table 1.
TABLE 1 Comparison of classification systems for psychosis
This diagnostic formulation should be accompanied by an idiographic formulation to complement the nomothetic nature of diagnosis and to compensate for the hyponarrativity of diagnostic systems such as DSM/ICD (Sadler Reference Sadler2005). This can include the patient's and carer's perspectives, cultural information relevant to their case, their goals for treatment and their understanding of their current predicament, including narrative elements and the patient's strengths (IGDA Workgroup 2003). Formulations using psychological models can also be incorporated where they can be demonstrated to improve understanding and targets for intervention; evidence-based models specific to psychosis, such as Freeman's cognitive model of delusions (Freeman Reference Freeman2016), are to be preferred to more generic psychological models.
Conclusions
The role of classification in mental illness remains complex. However, in clinical practice it can assist in conceptualising the patient's problems, facilitate communication between professionals about these problems, aid in the assessment process and enable extrapolation of clinically useful information from research to the patient (such as aetiology, prognosis and treatment). To improve the clinical utility of classification in psychosis, it could be argued that clinicians may be wise to avoid exclusively using either neo-Kraepelinian categories that do not fit some patients or a unitary psychosis model that relies on unsafe assumptions and loses clinically useful information. The use of such conceptual frameworks exclusively, and the limitations that they impose, may bring more challenges to clinical practice than they resolve. It may be better to use either system as best fits the individual patient. The diagnosis of schizophrenia should be restricted only to those with characteristic phenomenological changes, or those who show primary negative symptoms or significant cognitive impairment. Finally, the importance of detailing relevant co-occurring conditions should be noted, along with the exploration of known risk factors, including psychosocial risk factors, and the addition of idiographic information and psychological formulation to improve case conceptualisation in a biopsychosocial framework.
Author contributions
This article is based on a blog written by J.P. with some minor suggestions by S.H.; S.H. expanded the blog into an article, which has been revised with suggestions by J.P.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
A.S.H. is author of book referenced in this article discussing and defending the medical model including the use of categorical diagnosis.
MCQs
Select the single best option for each question stem
1 As regards the nature and purpose of diagnosis:
a the prime purpose of diagnosis in clinical practice is to create scientifically accurate categories for researchers
b the practicality of a particular classification type in situations of limited clinical time or in emergencies is irrelevant
c since all patients are unique then classification should not be used
d DSM and ICD diagnostic classifications assume that all mental health problems exist in neat categories
e diagnosis can be combined with idiographic and other relevant information about the individual to give a broader formulation.
2 The neo-Kraepelinian DSM and ICD diagnostic constructs for psychosis:
a are based on Kraepelin's division of psychosis into two diseases based on differing outcomes that he believed in until his dying day
b have clinical utility, for example in prognosis and predicting response to medications
c have no phenomenological or prognostic differences across the different diagnostic constructs
d are based on clear-cut biological differences between the different diagnostic constructs
e are not associated with stigmatising attitudes.
3 The unitary psychosis model:
a is compatible with the finding that psychotic symptoms occur in mental health problems of various types and severity that are not traditionally regarded as psychosis
b only came into being in the late 20th century after disenchantment with the failure to find specific causes and mechanisms for the DSM/ICD categories of psychosis
c can easily describe all clinically relevant cases of psychosis, such as substance intoxication syndromes and psychotic symptoms secondary to general medical conditions
d uses dimensional ratings of psychosis that cannot be matched to equivalent DSM/ICD categories
e has a consistent dimensional model with the number and nature of dimensions consistent across all studies.
4 Comparing the unitary and neo-Kraepelinian models of psychosis:
a there are more studies with directly relevant clinical information (such as for prognosis and treatment) using the unitary psychosis model than DSM/ICD categories
b unitary psychosis models have superior clinical utility to the neo-Kraepelinian model for all cases of clinical psychosis
c a unitary psychosis model using dimensions may be more useful for researchers trying to investigate causes of psychotic symptoms than DSM/ICD categories without dimensional symptom ratings
d adopting the unitary psychosis model means never having to use any DSM/ICD categories for any patient presenting with psychotic symptoms
e the DSM/ICD schizophrenia category without dimensional ratings describes symptomatic heterogeneity of cases better than a unitary psychosis model using dimensional ratings.
5 In terms of aetiology of psychosis:
a the DSM/ICD diagnostic categories are associated with aetiological factors unique to them
b van Os & Reininghaus's unitary psychosis model provides unitary psychosis model provides comprehensive aetiological information for each case through its dimensional rating system
c the increased risk of psychosis for Black Caribbean people in the UK is likely due to genetic factors
d psychosocial factors are irrelevant to the risk of developing psychosis
e multiple biopsychosocial factors have been demonstrated to increase risk for developing psychosis and should be included in diagnostic formulations.
MCQ answers
1 e 2 b 3 a 4 c 5 e








eLetters
No eLetters have been published for this article.