Introduction
Countries having stronger primary care generally have healthier people (Starsfield et al., Reference Starsfield, Shi and Macinko2005). Though health policies and practices are different worldwide, family medicine constitutes the basic element of health services. A strong primary care enables a cheaper healthcare service that is more easily accessible and with better satisfaction (Kringos et al., Reference Kringos, Boerma, Bourgueil, Cartier, Dedeu, Hasvold, Hutchinson, Lember, Oleszczyk, Rotar Pavlic, Svab, Tedeschi, Wilm, Wilson, Windak, Van der Zee and Groenewegen2013). Research has shown that family doctors can deliver solutions for more than 90% of the problems of their patients without referral (Grumbach et al., Reference Grumbach, Selby and Damberg1999; Ustu and Ugurlu, Reference Ustu and Ugurlu2015).
In Turkey, following pilot schemes, family medicine has begun to be applied throughout the country since 2010 (Akman, Reference Akman2014). The determinants of medical service quality in Turkey have been affected positively with the family practice system (Hone et al., Reference Hone, Gurol-Urganci, Millett, Basaran, Akdag and Atun2017). A significant decrease in the mortality rate of mothers and babies under five attracts notice, which is attributed to health reforms, including Family Medicine, that have been implemented (Jelamschi and De Ver Dye, Reference Jelamschi and De Ver Dye2009; Turkish Ministry of Health, 2012-2014).
While there is a remarkable improvement in health outcomes, an increased number of visits to Emergency Departments (EDs) have come to the forefront as one of the most important problems in the Turkish healthcare system (Ulker et al., Reference Ulker, Taskin, Yardimci, Hocagil and Hocagil2017). The best example of this situation is that there are more visits to EDs annually than the total population of Turkey. The data of the Republic of Turkey, Ministry of Health, reports that there were 100 081 171 visits to the EDs in 2013 (Bektemur et al., Reference Bektemur, Osmanbeyoglu and Cander2015). For comparison, in the United States overall, there are 42 ED visits per 100 persons annually (Dyrda, Reference Dyrda2016) and ED attendance was more than 400 per 1000 persons in the United Kingdom in 2015 (Baker, Reference Baker2017).
There may be many explanations for high rates of ED admissions in Turkey, for example absence of an obligatory referral system is one of them. A referral system is obligatory in half of the European countries and self-referrals are subject to financial implications in some countries (Kringos et al., Reference Kringos, Boerma, Bourgueil, Cartier, Dedeu, Hasvold, Hutchinson, Lember, Oleszczyk, Rotar Pavlic, Svab, Tedeschi, Wilm, Wilson, Windak, Van der Zee and Groenewegen2013). In seven European countries, including Turkey, self-referral is free.
The triage system gives priority to patients according to the urgency of the situation. In the red zone, patients should be quickly treated while in the green zone patients can wait for a longer time, who often suffer from illnesses that could be solved in family medicine offices (Durand et al., Reference Durand, Gentile, Gerbeaux, Alazia, Kiegel and Luigi2011). To get a more efficient emergency service, non-urgent cases could be evaluated by family physicians. In the United Kingdom, for example, redirection of patients from the green zone to GPs after a preliminary examination in triage is an effort towards a solution of the problem (Bentley et al., Reference Bianco, Pileggi and Angelillo2017).
In the present study, the aim was to identify the reasons why patients with minor complaints choose EDs as a first contact of care, instead of primary care, and whether dissatisfaction with primary care services influences their decisions.
Methods
Participants
The study was designed as a descriptive study. In total, 840 patients who were admitted to the Bursa Yuksek Ihtisas Training and Research Hospital ED in July 2015, who undertook consultation in the green zone and who were recorded as outpatients participated in the study. In the same period, 22 538 patients in total were consulted in the green zone. The patients involved in the study (n=840) consisted of 0.37% of these patients. A family medicine residency trainee working in the ED of the hospital in that period, in out of office hours, invited every eligible patient he examined to participate in the study. During the study, he was the single trainee working in the green zone of the hospital. The criteria for involvement in the study were patients over 18 years old, outpatients applying to the green zone, Turkish citizenship and voluntary involvement acceptance. Patients who had not visited their primary care doctor in the last 12 months were excluded from the study. A written informed consent was obtained from the participants.
Materials
This research used a questionnaire in order to identify socio-demographic characteristics. In addition to this, the EUROPEP (Patients Evaluate General/Family Practice) scale was used which measured the satisfaction of patients with the primary care services. Validation of the scale was obtained by Akturk et al. (Reference Akturk, Dagdeviren, Sahin, Ozer, Yaman, Goktaş, Filiz, Topsever, Organer, Aydin, Yaris and Maras2002). EUROPEP is a scale prepared by EQUIP (European Working Party on Quality in General Practice) that is used to evaluate family doctors and family health centers in more than 20 European countries. The scale is a self-completed survey and consists of five dimensions and 23 questions. These are doctor–patient relationship (questions 1–6), medical care (questions 7–11), information and support (questions 12–15), health service organization (questions 16–17) and accessibility (questions 18–23). Patients were asked to answer questions on a five-point scale ranging from 1=poor to 5=excellent, and all the items were scored in the same direction (Vedsted et al., Reference Vedsted, Sokolowski and Heje2008).
Statistical analysis
Categorical data were presented with frequency and related percentage values while continuous data were expressed as median (minimum: maximum). The relationship between patient satisfaction and the frequency of visits to EDs was evaluated by Mann–Whitney test. The correlation between the frequency of visits to the family doctor and EDs was evaluated by Spearman correlation coefficient. Patient mean satisfaction scores were divided into four groups according to quartiles and percentile values were calculated. Evaluation of the data was done using IBM SPSS 20.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0, IBM Corp., Armonk, NY) Statistical significance was set at P<0.05.
Results
In total, 53 patients who were either visitors or who recently moved to the city and their family doctors were outside of Bursa were not included in the study; 179 patients who had not visited their family doctor in the last 12 months were also excluded. In total, 608 patients were invited into the study and 535 agreed to participate in the study (response rate was 87.9%); 26 patients who could not fill out the EUROPEP questionnaire were excluded from the research (Figure1). Data analysis was therefore performed with the results of 509 participants (Table 1).
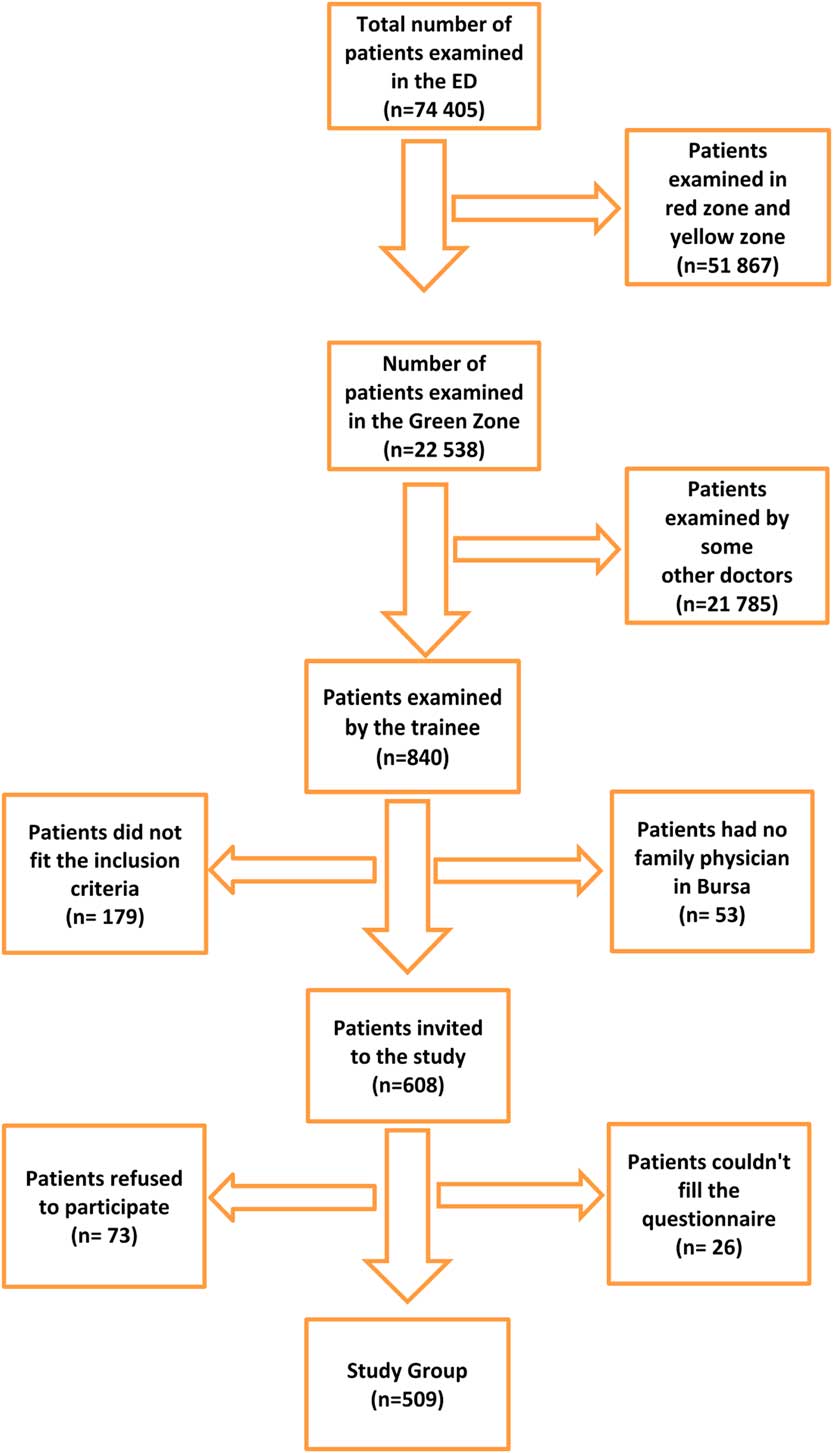
Figure 1 Patient inclusion flowchart
Table 1 Socio-demographic features of the patients
Of the total patients, 319 (71.7%) stated that their complication started within the previous three days. Overall, 446 (87.8%) of the patients’ first contact of care was in EDs (Table 2). The most frequently seen complaints leading to an ED visit were excessive pain (20.4%), perceived urgency (14.5%) and that EDs were available 24 h a day (13.2%) (Table 3). When patients’ primary complaints were examined: 175 patients (34.4%) had flu-like symptoms (fever and fatigue), 73 patients (14.3%) had chronic pain, 49 patients (9.6%) had dyspeptic complaints, 37 patients (7.3%) had migraine headache, 31 patients (6.1%) were referred to the EDs due to sore throat, 28 patients (5.5%) for skin problems and 116 patients (22.8%) for other complaints.
Table 2 Characteristics of complaints of the patients
Table 3 The reason why patients prefer emergency services
Analysis of the EUROPEP scale revealed that satisfaction with the family practice unit was 68.1%. The most satisfactory situation according to the patients was that their family doctor listens to them and performs a physical examination (76.8%). On the other hand, the most dissatisfactory situation for patients was that doctors (29.1%) and family medicine clinics (43.4%) cannot be reached by phone (Table 4).
Table 4 Patient satisfaction with family physicians
Satisfied patient corresponds to ones who marked the item as good or very good. Not satisfied patient corresponds to ones who marked the item as ‘bad’ and ‘very bad’.
Total response rate to the EUROPEP questions was 93.16%. And, the response rates for items varied between 98.82 and 74.07% (Table 5 and Figure 2). The item ‘making you feel you had time during consultation’ had the highest response rate (98.82), whereas the item ‘keeping your records and data confidential’ had the lowest response rate (74.07%).
Table 5 The number of participants who did not answer any particular question
When the patients were divided into quartile groups according to their average satisfaction scores, there was no statistically significant difference between the groups in terms of the frequency of ED visits in the last 12 months (P=0.09). It was found that there was a weak positive correlation between visits of patients to family doctors and to EDs (P<0.001; r=0.29). The internal reliability coefficient on the EUROPEP scale was 0.97 as a Cronbach’s α value (Figure 2).
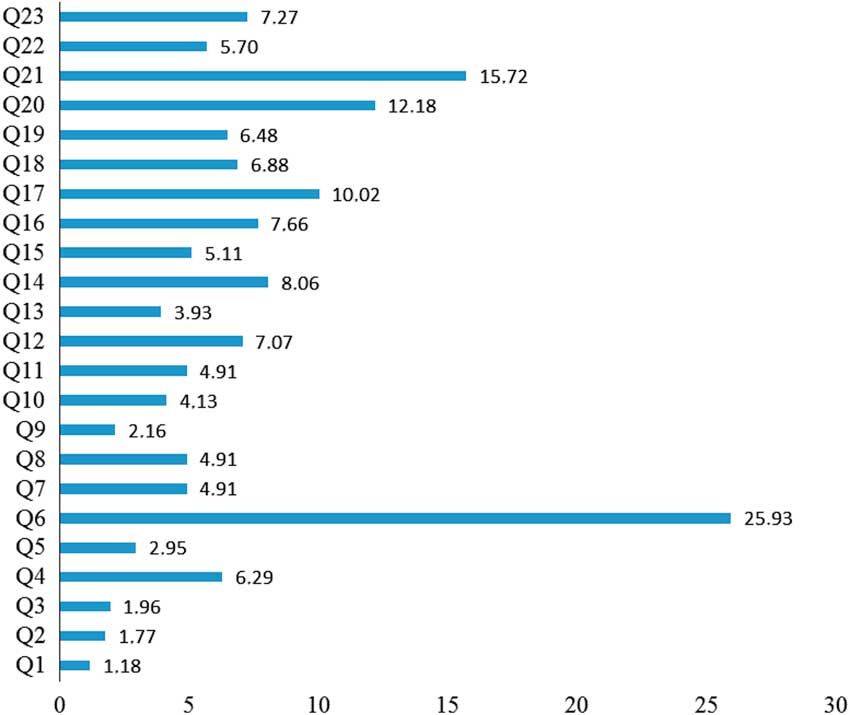
Figure 2 Distribution of unanswered questions. Q1: Making you feel you had time during consultation; Q2: Interest in your personal situation; Q3: Making it easy for you to tell him or her about your problem; Q4: Involving you in decisions about your medical care; Q5: Listening to you; Q6: Keeping your records and data confidential; Q7: Quick relief of your symptoms;Q8. Helping you to feel well so that you can perform your normal daily activities; Q9: Thoroughness; Q10: Physical examination; Q11: Offering services for preventing diseases (eg, screening and immunizations); Q12: Explaining the purpose of tests and treatments; Q13: Telling you what you wanted to know about your symptoms and/or illness; Q14: Helping you deal with emotional problems related to your health status; Q15: Helping understand the importance of following his or her advice; Q16: Knowing what s/he had done or told you during contacts; Q17: Preparing you for what to expect from specialist or hospital care; Q18: The helpfulness of the practice staff (other than the doctor); Q19: Getting an appointment to suit you; Q20: Getting through to the practice on the telephone; Q21: Being able to speak to the general practitioner on the telephone; Q22: Waiting time in the waiting room; Q23: Providing quick services for urgent health problems
Discussion
According to the results of this study, of the patients examined in the green zone, the main reasons for admission to EDs were feeling pain, the perception of urgency and that family doctor services were closed outside working hours. The large majority of the patients (71.7%) stated that their symptoms started within the last three days. In the absence of a referral system, easy accessibility to hospitals was the main reason why patients bypassed family doctors and came to EDs.
The duration of patient complaints was longer than that found in other studies. It was found that visits to EDs within the first 24 h of complications were 77% (Bianco et al., Reference Bostan and Havvatoglu2003; Durand et al., Reference Durand, Gentile, Gerbeaux, Alazia, Kiegel and Luigi2011). In a study performed in Turkey, the rate of visiting within the first 24 h was 73% (Akturk et al., Reference Akturk, Dagdeviren, Sahin, Ozer, Yaman, Goktaş, Filiz, Topsever, Organer, Aydin, Yaris and Maras2002). In the current study, we found that visits within 24 h of complications occurring were 32.1% and within the first three days of complications was 71.7%. These results show that especially acute cases prefer EDs. As previous studies included not only the green zone but the whole EDs, the percentage of visits within the first 24 h was higher. In this study, only those patients who were examined in the green zone were included. In the green zone, patients were at a lower risk of a life threatening condition. The cases were mostly composed of patients with flu-like symptoms, chronic pain and dyspeptic complaints. Patients can be educated how to manage these symptoms by increasing their health literacy.
It was reported that 72% of the ED applicants thought that their complications were medium or highly serious and 59% of them stated that their complications required immediate attention and treatment (Lucas and Sanford, Reference Lucas and Sanford1998). In another study investigating the reason why patients choose EDs, 85.8% of the patients came because of ‘pain’ and 60.5% of the patients were admitted to EDs thinking that their problem should be managed urgently (Durand et al., Reference Durand, Gentile, Gerbeaux, Alazia, Kiegel and Luigi2011). Similarly, in other studies patients reported that they came to EDs because they perceived urgent need (Shah and Shah, Reference Shah and Shah1994; Lucas and Sanford, Reference Lucas and Sanford1998; Bianco et al., Reference Bostan and Havvatoglu2003). Beland et al. showed that patients living near to the ED visit those departments more frequently and real emergency cases come to those departments from long distances (Beland et al., Reference Beland, Lemay and Boucher1998). In the present study, the reasons for visiting EDs were ‘feeling so much pain’ (backache, headache, migraine patients, pain due to trauma and pain due to infection) 20.4%, ‘thinking it is an emergency situation’ 14.5%, ‘EDs are open also outside work hours’ 13.2%, ‘fast examination and treatment at EDs’ 8.6%, ‘better intervention’ 4.3%, ‘near home’ 3.1% and ‘the opportunity for analysis and tests’ 2.4%. The present study is an example of what will happen with a self-referral system. In a self-referral system, hospital admissions originating from expectations (eg, faster and better service) were as much as admissions directed by serious symptoms.
In this study, the rate of admission to EDs as the first point of application was determined as 87.8%, which was because of the free self-referral system in Turkey. There are few countries in Europe that use a no-referral system. A referral system helps to triage patients in primary care, which is known as ‘gate keeping’ in healthcare facilities. If self-referral application persists, then we should educate people for better use of the system. Apart from this, 9% of patient family physicians who were outside of the Bursa province may have contributed to this increase. In one study, it was reported that family physicians were not eager to deal with guest patients (Akman, Reference Akman2014). If so, it would not be surprising that the patients referred themselves to hospitals. Guest patients were an extra burden on the ED, which must be solved by registering the patients as soon as possible when they move. Another reason for excessive ED applications was shown to be that family physicians could not be reached outside of working hours, similar to the results obtained in previous studies (Huntley et al., Reference Huntley, Lasserson, Wye, Morris, Checkland, England, Salibury and Purdy2014). Only EDs have healthcare workers where patients can receive health services outside of working hours. The 24-h primary care topic has been discussed extensively, but a sufficient number of qualified healthcare workers are needed for such an application.
In the current study, patient satisfaction with family doctors was lower when compared with previous studies performed at primary care facilities, but comparisons should be made with caution since patient profiles were different. In a previous study, patient satisfaction with primary care services was found to be 88.3% in Turkey (Akturk et al., Reference Akturk, Atesoglu and Ciftci2015). In the study of Mete et al., which was performed in Malatya, 80.7% of the participants stated that they were satisfied/very satisfied with the family medicine system (Mete et al., Reference Mete, Pehlivan, Tekin, Nacar, Unver and Baran2015). In the study, Bostan et al. performed in Gumushane, the general satisfaction level was 87.5% (Bostan and Havvatoglu, Reference Carrière2014). In the current study, satisfaction of the patients with their family doctors was 68.1%. They mostly suffered from lack of accessibility to their primary care office, either for visiting or by telephone contact. Inaccessibility is the predominant problem not only for the participants in the present study but is a common health problem for almost every country. Of course, it can be reinforced by increasing the number of qualified healthcare workers. But, to what extent? It is not possible to have a doctor on every block at every time. However, for example, efforts to improve health literacy in the public may help people to better benefit from health facilities. Family physicians should focus on this issue and should try to educate patients on health.
Many studies show that frequent users of EDs are also frequent visitors to family doctors (Ovens and Chan, Reference Ovens and Chan2001; Benjamin et al., 2002; Chan and Ovens, Reference Chan and Ovens2002; Carrière, Reference Chan and Ovens2004). This situation could be explained by people having many co-morbid diseases. Additionally, it was found that frequent users of EDs have a high risk of chronic diseases and a high mortality rate (Sun et al., Reference Sun, Burstin and Brennan2003; Hunt et al., Reference Hunt, Weber, Showstack, Colby and Callaham2006). In the present study, a relationship between the frequency of family doctor visits and the frequency of ED visits was found. Family physicians should carefully evaluate the history of frequent hospital/primary healthcare visits in terms of co-morbidities. For example, frequent visits due to throat infection may be associated with new onset diabetes mellitus. Similarly, infections that do not heal in an average time interval can be a sign of cancer or diabetes mellitus.
Limitations of the study
It would have been better to have a control group in the present study, since the EUROPEP questionnaire has no cut-off value and so classification of a person as satisfied or not satisfied was problematic. Instead of personal satisfaction, evaluation of general satisfaction was subject to discussion in the present study. It would have been better to compare satisfaction obtained from patients admitted to EDs with those who were not admitted as a case control study.
In conclusion, this study is the first to evaluate satisfaction with family doctors of patients visiting EDs using the EUROPEP scale. In this sampling, about one-third of the participants were not satisfied with their family practice services but satisfaction was not associated with frequent ED visits. In total, 9% of the patients invited to participate were not registered with a family physician working in the city and this puts extra burden on EDs. In the case of migration, family medicine records should be rapidly transferred to the new location. Frequent admissions should be carefully evaluated in terms of serious co-morbidities. Trials to improve public health literacy can be suggested to reduce non-urgent visits, especially in countries where self-referral is free.
Acknowledgments
The authors thank Mrs. Nazli Demirci (Philologist) for her contribution to the study.
Financial Support
None.
Conflicts of Interest
None.
Ethical Standard
The Ethics Committee of the Bursa Yuksek Ihtisas Training and Research Hospital approved the study.












