Introduction
Self-reported psychotic experiences such as hearing voices, experiencing paranoid thoughts, are common in the general population. These experiences have been conceptualised as existing on a continuum with psychotic illness (Linscott and van Os, Reference Linscott and Van Os2013), although this has been challenged (Parnas and Henriksen, Reference Parnas and Henriksen2016). Psychotic experiences are distinct from clinically detectable attenuated psychotic symptoms reported by help-seeking individuals (Fusar-Poli et al., Reference Fusar-Poli, Raballo and Parnas2016). Self-reported psychotic experiences in non-psychotic psychiatric disorders could be an indicator of greater illness severity or poorer healthcare outcomes compared with experiencing the same disorders without psychotic experiences. Nonetheless, although there exists a large literature on general population co-occurrence of psychotic experiences with other psychiatric disorders, including depression (Koyanagi et al., Reference Koyanagi, Oh, Stickley, Haro and Devylder2016), anxiety (Kelleher et al., Reference Kelleher, Devlin, Wigman, Kehoe, Murtagh, Fitzpatrick and Cannon2014), post-traumatic stress disorder (PTSD) (Kilcommons et al., Reference Kilcommons, Morrison, Knight and Lobban2008), and personality disorders (Newton-Howes et al., Reference Newton-Howes, Tyrer, North and Yang2008), there has been more limited examination of the implications of this comorbidity for public mental health. In particular, co-occurrence of psychotic experiences with non-psychotic psychiatric disorders could indicate greater psychopathological symptom burden, worse overall prognosis in terms of later use of health services, worse longer term functioning, or specific implications for physical health (Sharifi et al., Reference Sharifi, Eaton, Wu, Roth, Burchett and Mojtabai2015; Scott et al., Reference Scott, Saha, Lim, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Benjet, Bromet, Bruffaerts and Caldas-De-Almeida2018; Oh et al., Reference Oh, Waldman, Stickley, Devylder and Koyanagi2019), or suicide (Kelleher et al., Reference Kelleher, Lynch, Harley and Et2012). People with psychotic experiences present more frequently to specialist mental health services than the general population (Kobayashi et al., Reference Kobayashi, Nemoto, Murakami, Kashima and Mizuno2011; Murphy et al., Reference Murphy, Shevlin, Houston and Adamson2012; DeVylder et al., Reference Devylder, Oh, Corcoran and Lukens2014b), however information on use of psychological treatment for common mental disorders (CMDs) is more limited (Perez et al., Reference Perez, Russo, Stochl, Clarke, Martin, Jassi, French, Fowler and Jones2018). Psychiatric symptoms reported in general population surveys are also associated with worse physical health and functioning (Phelan et al., Reference Phelan, Stradins and Morrison2001; Moreno et al., Reference Moreno, Nuevo, Chatterji, Verdes, Arango and Ayuso-Mateos2013) and health-related quality of life (Alonso et al., Reference Alonso, Saha, Lim, Aguilar-Gaxiola, Al-Hamzawi, Benjet, Bromet, Degenhardt, De Girolamo and Esan2018). However, although the possible relevance of psychotic experiences for physical health has been examined in large-scale epidemiological data (Saha et al., Reference Saha, Scott, Varghese and Mcgrath2011; Moreno et al., Reference Moreno, Nuevo, Chatterji, Verdes, Arango and Ayuso-Mateos2013), the effect of psychotic experiences concurrent with non-psychotic psychiatric disorders on physical functioning has received a limited amount of attention.
We therefore aim (1) to describe the distribution of self-reported psychotic experiences co-occurring with a range of non-psychotic psychiatric disorders, and (2) to examine the association of these comorbid psychotic experiences with outcomes of public health importance: use of secondary mental healthcare, use of psychological treatment for CMDs, lifetime suicide attempts, and poor self-rated health.
Methods
Sample details
This study linked a cross-sectional community health survey with a mental healthcare provider database. The South East London Community Health Study, SELCoH (Hatch et al., Reference Hatch, Frissa, Verdecchia, Stewart, Fear, Reichenberg, Morgan, Kankulu, Clark and Gazard2011), is a representative household survey whose first wave (SELCoH-1) took place in 2008–2010. The survey used random household sampling to identify a representative sample of adults aged 16–90 years living in Lambeth and Southwark. Sampling was clustered by household, with all adults living in selected households invited to participate. Full details of the study, its sampling methods, and representativeness are described elsewhere (Hatch et al., Reference Hatch, Frissa, Verdecchia, Stewart, Fear, Reichenberg, Morgan, Kankulu, Clark and Gazard2011). Among 1698 participants surveyed, 86% gave permission for linkage to specialist mental health records, where those records were available. Data on participants were linked to electronic health record data on use of mental health services both before and after SELCoH-1 interview (described further in the ‘Outcomes’ section). Data from SELCoH phase 2, a survey performed in 2012–2013 and based on the same sample, were used to ascertain which participants had subsequently left the catchment area or died (Hatch et al., Reference Hatch, Gazard, Williams, Frissa, Goodwin, Hotopf and Team2016).
Measurements
Psychotic experiences
The Psychosis Screening Questionnaire (PSQ) (Bebbington and Nayani, Reference Bebbington and Nayani1995) was used to assess psychotic experiences. This is a five-item self-report questionnaire which evaluates different psychotic experiences domains experienced in the previous year. These comprise: hypomania, strange experiences, paranoia, hallucinations, and thought disorder. Each domain contains an initial ‘probe’ item followed by secondary questions. Because the current study was focused on common psychiatric disorders co-occurring with non-affective psychotic experiences, responses to the hypomania item were not examined. Individuals were considered to have psychotic experiences if they endorsed one or more secondary items in the four remaining domains. The PSQ displays good correspondence with psychosis items on the Schedules for Clinical Assessment in Neuropsychiatry (Bebbington and Nayani, Reference Bebbington and Nayani1995), and has seen frequent use in population studies (Bebbington et al., Reference Bebbington, Bhugra, Brugha, Singleton, Farrell, Jenkins, Lewis and Meltzer2004).
Non-psychotic psychiatric disorders
CMDs were assessed by the Revised Clinical Interview Schedule (CIS-R) (Lewis et al., Reference Lewis, Pelosi, Araya and Dunn1992), giving a score out of 49 for symptoms occurring within the previous 4 weeks. In line with previous studies (Hatch et al., Reference Hatch, Gazard, Williams, Frissa, Goodwin, Hotopf and Team2016), we categorised scores into groups for scores of 0–11 (no CMD), 12–18 (mild/moderate symptoms of CMD), and over 18 (severe symptoms of CMD). Diagnoses of depressive episode and anxiety disorder were derived through a standard ICD-10 based algorithm. The anxiety disorder category included those with derived diagnoses of generalised anxiety disorder, obsessive-compulsive disorder, mixed anxiety and depression, specific phobia, social phobia, agoraphobia, generalised anxiety disorder, and panic disorder. Post-traumatic stress symptoms in the past month were assessed using the PC-PTSD (Prins et al., Reference Prins, Ouimette, Kimerling, Camerond, Hugelshofer, Shaw-Hegwer, Thrailkill, Gusman and Sheikh2003), a screening tool for PTSD designed for primary care use, which is based on the diagnostic criteria for PTSD in DSM-V. We used a cut-off point of 3 or more to define probable PTSD, which has been shown to have high specificity (0.88) and acceptable sensitivity (0.76) (Cameron and Gusman, Reference Cameron and Gusman2003). Personality dysfunction (PD) was assessed using the Standardised Assessment of Personality-Abbreviated Scale (SAPAS), a rapid screen for personality disorder, which has demonstrated good psychometric properties (Moran et al., Reference Moran, Leese, Lee, Thornicroft and Mann2003) and clinical utility (Bock et al., Reference Bock, Bukh, Vinberg, Gether and Kessing2010; Bukh et al., Reference Bukh, Bock, Vinberg, Gether and Kessing2010; Germans et al., Reference Germans, Van Heck and Hodiamont2012). The SAPAS consists of eight questions, corresponding to descriptive statements about the person's usual behaviour, currently. Binary responses are summed to derive an overall score, for which a cut-off of 4 was used, which has showed satisfactory positive predictive value in community settings (Moran et al., Reference Moran, Leese, Lee, Thornicroft and Mann2003).
Covariates
SELCoH-1 collected sociodemographic, environmental and health information. Ethnicity was operationalised as a five-category variable comprising white, black African, black Caribbean, Asian, and other groups. Marital status was categorised into single, married/cohabiting, divorced/separated, and widowed. Drug use information was ascertained by self-report of use of any illicit drug (cannabis, crack, cocaine, ecstasy, LSD, and heroin) in the previous year. Alcohol use patterns in the past year were measured using the AUDIT scale (Saunders et al., Reference Saunders, Aasland, Babor, De La Fuente and Grant1993), using a cut-off of 8 to identify hazardous alcohol use, in line with previous studies.
Outcomes
Two indicators of mental health service use were used: specialist mental health service use, and use of psychological treatment for CMDs. Specialist mental health service use was ascertained using data from the National Institute of Health Research Biomedical Research Centre at the Maudsley's Clinical Record Interactive Search (CRIS) (Stewart et al., Reference Stewart, Soremekun, Perera, Broadbent, Callard, Denis, Hotopf, Thornicroft and Lovestone2009) system. The South London and Maudsley NHS Foundation Trust (SLaM) is the sole provider of public mental healthcare in the two boroughs of South London that were surveyed in SELCoH-1, covering a catchment population of approximately 620 000. The Trust has used a single electronic health record across all clinical services known as the electronic Patient Journey System (ePJS) since 2006. The CRIS system extracts de-identified clinical data from ePJS including structured fields for ICD-10 diagnoses, treatments and admissions to hospital. The Improving Access to Psychological Treatment (IAPT) programme is a national network of services providing psychological treatment for CMDs, spanning primary and secondary care. For this study, linkage of SELCoH-1 data was also carried out to IAPT-CRIS, an electronic system extracting de-identified clinical data from IAPTUS, the electronic system used by professionals providing IAPT-based treatment, which includes structured fields for ICD-10 diagnoses, treatments, and outcome.
Linkage of SELCoH-1 to CRIS and IAPT-CRIS was carried out by an independent Clinical Data Linkage Service (CDLS), and used personal identifiers (name, date of birth, NHS number, postcode, and gender) to probabilistically link survey data with matching electronic health records (Centre, 2015). Data on SELCoH-1 participants who had consented to record linkage were then scrutinised in CRIS and IAPT-CRIS for date of referral. This linked information was used to derive two binary variables for any specialist mental health service use (from CRIS), and any use of psychological treatment (from IAPT-CRIS), and two variables for survival analysis, for time to contact with specialist mental health services (from CRIS), and time to use of psychological treatment (from IAPT-CRIS). Referral information for this study was available from 1st April 1999 to 15th May 2017 for specialist mental health service use, and from 1st January 2008 until 31st November 2018 for use of psychological treatment.
Physical functioning was measured in SELCOH-1 using the physical component of the SF-12 (Ware and Kosinski, Reference Ware and Kosinski2001), a 12 item scale capturing limitation in daily activities for physical health reasons in the previous 4 weeks. Poor physical functioning was a binary indicator based on the lowest quartile of the physical component score on the SF-12 (Das-Munshi et al., Reference Das-Munshi, Goldberg, Bebbington, Bhugra, Brugha, Dewey, Jenkins, Stewart and Prince2008). Finally, lifetime suicide attempt was evaluated using a self-report item in SELCoH-1.
Ethical approval
The SELCoH-1 study received approval from the King's College London research ethics committee, reference CREC/07/08-152. The CRIS data resource received ethical approval as an anonymised data set for secondary analyses from Oxfordshire REC C, reference 08/H0606/71+5.
Comorbidity
Non-psychotic psychiatric disorders were defined by dichotomising scales as described above. For each possible combination of psychotic experiences and non-psychotic psychiatric disorder, a four-level categorical variable was created, reflecting those with neither psychotic experiences nor disorder, disorder without psychotic experiences, psychotic experiences without disorder, and psychotic experiences and disorder. For example, the PTSD-psychotic experiences comorbidity variable had the following levels: (a) neither psychotic experiences nor PTSD, (b) PTSD only, (c) psychotic experiences only, and (d) both psychotic experiences and PTSD.
Analyses
All analyses were carried out in STATA 14 (StataCorp, 2014), and took account of survey design, household clustering, and non-response within households. Frequencies and prevalence of psychotic experiences were described within each non-psychotic psychiatric disorder, outcome, and all covariates. Frequencies and prevalence of each outcome were described for participants with each non-psychotic psychiatric disorder and concurrent psychotic experiences.
Binary outcomes for logistic regression modelling were: specialist mental health service use, use of psychological treatment, lifetime history of suicide attempt, and lowest-quartile of the SF-12 physical component score.
Logistic regressions were estimated for each pairing of non-psychotic psychiatric disorder and outcome. For each non-psychotic psychiatric disorder, we estimated odds ratios (ORs) for the association between that disorder and the outcome, the association of psychotic experiences with the outcome, and the additive interaction between the two, calculating the interaction contrast ratio (ICR, also referred to as the relative excess risk due to interaction) describing the extent of departure of the relationship between psychotic experiences and each non-psychotic psychiatric disorder from an additive relationship, and a likelihood ratio test to assess statistical evidence for departure of the relationship from additivity (a small p value indicating evidence of interaction). All models included age as continuous variable, gender, and ethnicity as a priori confounders. Marital status, drug use, and hazardous alcohol use were evaluated as potential confounders, and not included models as adjusted estimates did not change by greater 10% of the crude value, on inclusion of any of these variables (Greenland et al., Reference Greenland, Daniel and Pearce2016). Based on this approach, final models were adjusted for age, gender, and ethnic group.
Survival analysis
We also took information on all referrals to specialist mental health services, and to psychological treatment for CMDs occurring subsequently to the survey interview (Bhavsar et al., Reference Bhavsar, Maccabe, Hatch, Hotopf, Boydell and Mcguire2017), in order to test the association between experiencing non-psychotic psychiatric disorder with concurrent psychotic experiences and time to specialist mental health service use, and time to use of psychological treatment. After assessing proportionality of hazards with a statistical test based on Schoenfeld residuals, survey-weighted Cox regression analyses were conducted, evaluating the association of concurrent psychotic experiences on time to secondary mental healthcare use, adjusting for age, gender, and ethnic group. As for logistic regressions described, we estimated ICRs and likelihood ratio tests for interaction on the additive scale.
Results
Psychotic experiences were reported by 19.7% of the study population. Table 1 shows the socio-demographic and clinical associations of psychotic experiences. Psychotic experiences were less frequently reported in older participants, similarly distributed by sex, but more frequently reported by those who identified as black Caribbean or black African than other ethnic groups. Psychotic experiences were most common among single people, and least common among married/cohabiting respondents. There was a noticeably higher prevalence of psychotic experiences with increasing symptoms. Similarly, psychotic experiences were reported more frequently in those experiencing every non-psychotic psychiatric disorder that was included in this study. Psychotic experiences were reported around a quarter of those with any use of psychological treatment for CMDs (25.4%), and nearly two-fifths of those with specialist mental health service use (38.1%), and 34.3% of those with relatively poor physical functioning. More than two-fifths of those reporting a lifetime history of suicide attempts (42.7%) reported psychotic experiences.
Table 1. Non-psychotic psychiatric disorders, sociodemographic characteristics and outcomes by psychotic experiences (PE) status
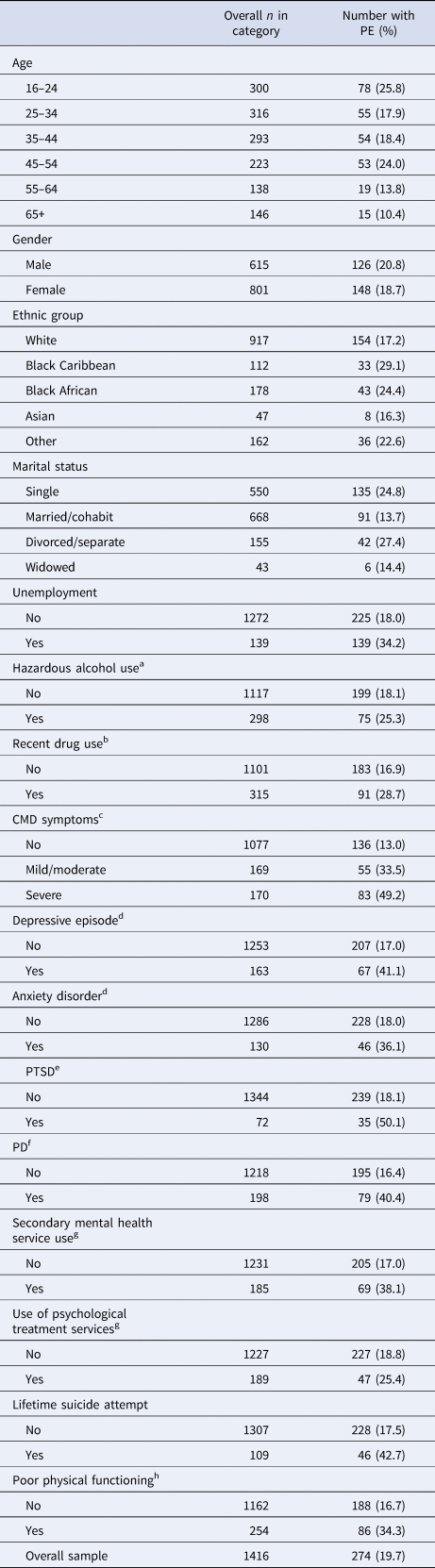
Percentages are weighted for survey design and non-response within households.
a Defined as scoring 8 or above on the AUDIT.
b Use of any of the following in the previous year: cannabis, cocaine, crack, opiates, amphetamines, ecstasy, and LSD.
c Based on scores on the Clinical Interview Schedule-Revised (CIS-R).
d Derived from items on the CIS-R.
e Derived from the PC-PTSD with a cut-off of 3.
f Derived from the SAPAS.
g Based on linkage to databases for specialist mental health records including secondary mental health services and use of psychological treatment services.
h Binary indicator based on the lowest quartile of the physical component score on the SF-12.
Table 2 describes, for each non-psychotic psychiatric disorder, how the concurrent presence of psychotic experiences was associated with specialist mental health service use, use of psychological treatment, lifetime suicide attempt, and poor physical functioning. With the exception of the association of anxiety disorder with use of psychological treatment, all outcomes were more common in those with non-psychotic psychiatric disorders with concurrent psychotic experiences compared to those without. Among participants reporting psychiatric disorders with concurrent psychotic experiences, proportions with specialist mental health service use ranged from 14% among those reporting mild/moderate symptoms of CMD with psychotic experiences, to 57.6% among those reporting PTSD with psychotic experiences. Use of psychological treatment among those with psychiatric disorders concurrent with psychotic experiences ranged from 11.7% among those with mild/moderate symptoms of CMD and psychotic experiences to 41.9% among those with PTSD and psychotic experiences. The proportion reporting lifetime suicide attempt among those with concurrent psychiatric disorders with psychotic experiences ranged from 17.6% among those reporting mild/moderate symptoms of CMD with psychotic experiences, to 42.8% in those with PTSD with psychotic experiences. The proportion of those experiencing poor physical functioning ranged from 29.6% of those with mild/moderate symptoms of CMD with psychotic experiences to 67.4% of those with depressive episode and psychotic experiences.
Table 2. Frequencies and proportions for analysed outcomes for each PE-comorbidity
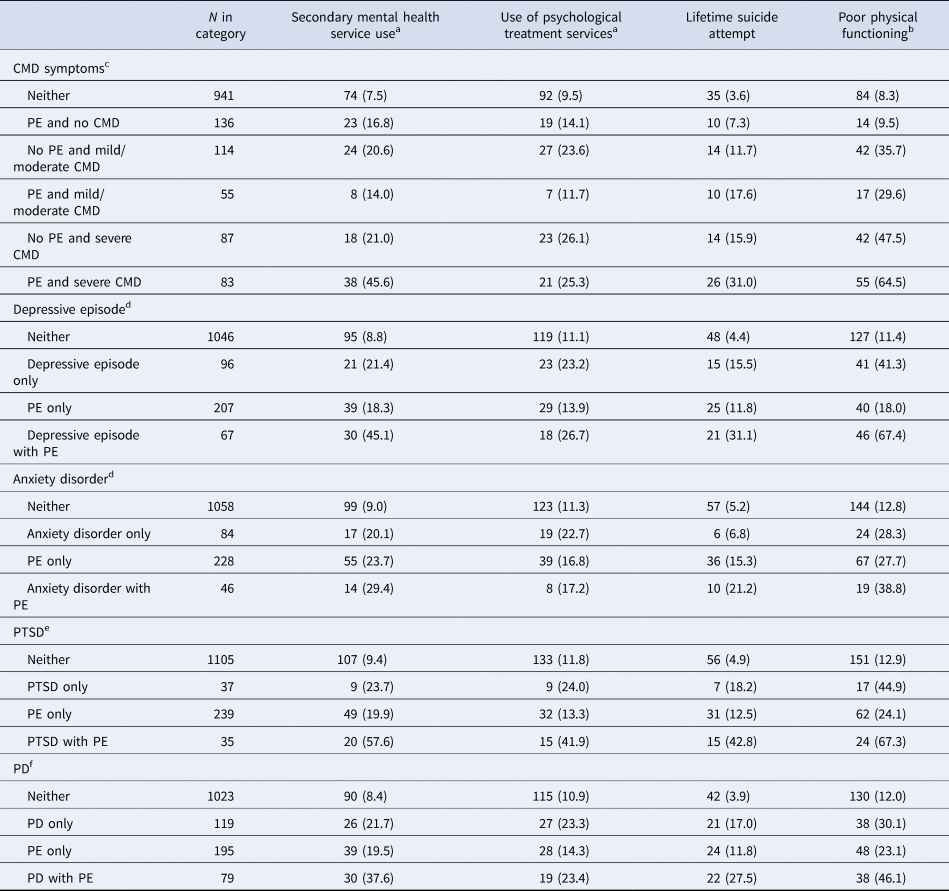
a Based on linkage to databases for specialist mental health records including secondary mental health services and use of psychological treatment services.
b Binary indicator based on the lowest quartile of the physical component score on the SF-12.
c Based on scores on the Clinical Interview Schedule-Revised (CIS-R).
d Derived from items on the CIS-R.
e Derived from the PC-PTSD with a cut-off of 3.
f Derived from the SAPAS.
Table 3 displays adjusted associations of each non-psychotic psychiatric disorder with specialist mental health service use, use of psychological treatment, lifetime suicide attempt and poor physical functioning. All comparisons are made to the group without psychotic experiences and each non-psychotic psychiatric disorder. The associations of concurrent psychotic experiences with secondary mental health service use ranged from ORs of 2.24 [95% confidence interval (CI) 1.04–4.83] for mild/moderate symptoms of CMD with psychotic experiences to 2.91(95% CI 1.37–6.19) for PD with psychotic experiences. Associations of psychiatric disorders with psychotic experiences and psychological treatment ranged from an OR of 1.24 (95% CI 0.56–2.73) in those with mild/moderate symptoms of CMD with psychotic experiences to 5.46 (95% CI 2.64–11.31) in those with psychotic experiences and PTSD. Associations with lifetime suicide attempt ranged from an OR of 5.42 (95% CI 2.50–11.77) among those with psychotic experiences with anxiety disorder to 17.83 (95% CI 8.13–39.09) in those with psychotic experiences with PTSD. Associations of concurrent psychotic experiences with poor physical functioning ranged from an OR of 6.63 (95% CI 3.40–12.94) for psychotic experiences with anxiety disorder to 23.54 (95% CI 11.07–50.08) for psychotic experiences with PTSD. Statistical evidence for interaction was found (p = 0.01) between psychotic experiences and CMD on specialist mental health service use with negative interaction between psychotic experiences and mild/moderate CMD (ICR: −2.65, 95% CI −5.24 to −0.07), and positive interaction between psychotic experiences and severe CMD (ICR: 6.09, 95% CI 0.53–11.64). Interaction between psychotic experiences and CMD displayed a similar pattern for use of psychological treatment, however there was insufficient statistical evidence of interaction (p = 0.0532). There was evidence of generally positive interaction on the additive scale between psychotic experiences and CMD for both lifetime suicide attempts and poor physical functioning. ICR point estimates suggested positive interaction for psychotic experiences with depressive episode for all outcomes, although statistical evidence was insufficient. We found indication of negative interaction between psychotic experiences and anxiety disorder on specialist mental health service use, and on use of psychological treatment, but not for lifetime suicide attempts and poor physical functioning. Large ICRs were observed for the interaction between psychotic experiences and PTSD for all outcomes, although all p values were greater than 0.05.
Table 3. Estimates for the association (ORs and 95% CIs) of psychotic experiences (PE) concurrent with other mental disorders on public mental health, estimated from survey-weighted logistic regression models with additive interaction terms

All estimates are adjusted for age, gender, and ethnic group.
a Based on linkage to databases for specialist mental health records including secondary mental health services and use of psychological treatment services.
b CMD symptoms based on categorisation of CIS-R score into three groups: 0–11 (no CMD), 12–18 (mild/moderate CMD), and over 18 (severe CMD).
c ICR: interaction contrast ratio, quantifying interaction on the additive scale.
d Derived from items on the CIS-R.
e Derived from the PC-PTSD with a cut-off of 3.
f Derived from the SAPAS.
g Binary indicator based on the lowest quartile of the physical component score on the SF-12.
Table 4 shows the results of survival analysis of the association between non-psychotic psychiatric disorders with concurrent psychotic experiences and subsequent use of specialist mental health services, based on additive interaction terms. Compared to those without those symptoms, statistical associations were found for psychotic experiences concurrent with severe CMD and with depressive episode, PTSD, and PD, but not for mild/moderate CMD, or anxiety disorder. Estimates indicated a nearly four-fold increase in the rate of mental health service use for concurrent psychotic experiences with PTSD compared to those without psychotic symptoms or PTSD [hazard ratio (HR) 3.81, 95% CI 2.11–6.87], a 2.5-fold such increase in those with psychotic experiences concurrent with severe CMD (compared to those with neither symptoms of CMD nor psychotic experiences, HR 2.59, 95% CI 1.52–4.40), more than a two-fold increase in those with depressive episode concurrent with psychotic experiences (HR 2.29, 95% CI 1.33–3.94) compared to those without psychotic experiences or depressive episode, and a nearly two-fold such increase in those with psychotic experiences concurrent with PD (compared to those without psychotic experiences or PD, HR 1.03, 3.24).
Table 4. Prospective associations (HRs) and 95% CIs, for PE concurrent with CMDs and the rate of psychological treatment and the rate of contact with mental health services

All estimates are adjusted for age, gender, and ethnic group.
a CMD symptoms based on categorisation of CIS-R score into three groups: 0–11 (no CMD), 12–18 (mild/moderate CMD), and over 18 (severe CMD).
b ICR: interaction contrast ratio, quantifying interaction on the additive scale.
c Derived from items on the CIS-R.
d Derived from the PC-PTSD with a cut-off of 3.
e Derived from the SAPAS.
f Based on linkage to databases for specialist mental health records including secondary mental health services and use of psychological treatment services.
Compared to those without those symptoms, statistical associations with time to use of psychological treatment were found for psychotic experiences concurrent with severe symptoms of CMD, depressive episode, PTSD, and PD. Estimates indicated a nearly three-fold increase in the rate of use of psychological treatment among those reporting PD with psychotic experiences, compared to those without these symptoms (HR 2.88, 95% CI 1.11–7.43), a nearly seven-fold increase in those reporting PTSD with psychotic experiences compared to those without (HR 6.80, 95% CI 3.18–14.54), a nearly six-fold increase among those reporting psychotic experiences concurrent with depressive episode (HR 5.90, 95% CI 3.11–11.18), and a similar increase among those reporting psychotic experiences concurrent with severe symptoms of CMD (HR 6.30, 95% CI 3.43–1.59). Inspection of ICR suggested statistical evidence of negative interaction on the additive scale between psychotic experiences and anxiety disorder on use of psychological treatment (ICR: −3.17, 95% CI −6.35 to 0.01, p = 0.014).
Discussion
Summary of findings
Consistent with previous literature (Linscott and van Os, Reference Linscott and Van Os2013), this investigation of a representative urban community sample found psychotic experiences to be common (19.7%), and strongly associated with non-psychotic psychiatric disorders. We found that for each non-psychotic disorder, the presence of psychotic experiences greatly increased the odds of specialist mental health service use, psychological treatment for CMDs, lifetime suicide attempts, and impairment of physical functioning. In general, ICRs suggested positive synergy between psychotic experiences and non-psychotic psychiatric symptoms on public mental health need, with the exception of mild/moderate CMD and anxiety disorders.
The prevalence of psychotic experiences identified in this study falls within the highest decile of the distribution of previous prevalence reports based on meta-analysis (Linscott and van Os, Reference Linscott and Van Os2013), and is considerably higher than the national prevalence of psychotic experiences based on a national survey of psychiatric morbidity carried out in 2007 (Koyanagi et al., Reference Koyanagi, Stickley and Haro2015). This is consistent with the greater prevalence of socioeconomic disadvantage, adversity, and substance use in densely populated urban areas compared to the rest of the population (Morgan et al., Reference Morgan, Reininghaus, Reichenberg, Frissa, Hotopf and Hatch2014).
Previous literature
Frequent comorbidity between psychotic experiences and other psychopathology, including depression (Ohayon and Schatzberg, Reference Ohayon and Schatzberg2002), and anxiety (Wigman et al., Reference Wigman, Van Nierop, Vollebergh, Lieb, Beesdo-Baum, Wittchen and Van Os2012), has been established in previous clinical and epidemiological studies. For example, in an analysis of four American general population datasets (DeVylder et al., Reference Devylder, Burnette and Yang2014a), psychotic experiences were markers of a greater number of psychiatric symptoms. A number of studies have also found psychotic experiences to be associated with adverse public health outcomes, including suicidal behaviours (Bromet et al., Reference Bromet, Nock, Saha, Lim, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Borges, Bruffaerts and Degenhardt2017), functional impairment, and disability (Kelleher et al., Reference Kelleher, Wigman, Harley, O'hanlon, Coughlan, Rawdon, Murphy, Power, Higgins and Cannon2015; Navarro-Mateu et al., Reference Navarro-Mateu, Alonso, Lim, Saha, Aguilar-Gaxiola, Al-Hamzawi, Andrade, Bromet, Bruffaerts and Chatterji2017; Oh et al., Reference Oh, Koyanagi, Kelleher and Devylder2018). For example, in a non-representative sample of 212 adolescents (Kelleher et al., Reference Kelleher, Wigman, Harley, O'hanlon, Coughlan, Rawdon, Murphy, Power, Higgins and Cannon2015), meeting criteria for an Axis I psychiatric diagnosis and endorsing psychotic experiences was associated with worse functioning compared to those with a diagnosis not endorsing psychotic experiences. Based on a cross-national sample of nearly 200 000 adults, Koyanagi et al. (Reference Koyanagi, Oh, Stickley, Haro and Devylder2016) found greater functional impairments in those with coexisting depressive episode and psychotic experiences, compared to those with depressive episode alone. In contrast to our study, they did not find association between reporting concurrent psychotic experiences and poor physical functioning.
However, few studies have examined the public mental health impact of intersection between psychotic experiences and non-psychotic psychiatric disorders, which is important based on the frequent overlap of psychotic experiences with other psychopathology. Kelleher et al. (Reference Kelleher, Devlin, Wigman, Kehoe, Murtagh, Fitzpatrick and Cannon2014) examined the prevalence of previous suicide attempts among Irish adolescents with psychiatric symptoms, comparing those reporting psychotic experiences to those not reporting psychotic experiences. Examining affective, behavioural and anxiety disorders, suicide attempts were associated with reporting concurrent psychotic experiences compared to experiencing these disorders without psychotic experiences. This study ascertained clinical diagnoses, in a relatively small group of help-seeking adolescents. In the general population based World Mental Health surveys, psychotic experiences were prospectively associated with attempted suicide (Bromet et al., Reference Bromet, Nock, Saha, Lim, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Borges, Bruffaerts and Degenhardt2017), but investigators did not aim to examine the effect of psychotic experiences concurrent with other psychiatric symptoms or disorders on the outcome. In contrast to previous studies, we examine the influence of a comprehensive range of psychiatric disorders comorbid with psychotic experiences on outcomes of broad public mental health importance.
Studies on risk factors for psychotic experiences have typically adjusted for other psychopathology as potential confounding variables, that is, as common causes of both exposure and outcome, rather than assessing their implications in combination. For example, McGrath et al. (Reference Mcgrath, Saha, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bromet, Bruffaerts, Caldas De Almeida, Cardoso, De Girolamo, Fayyad, Florescu, Gureje, Haro, Kawakami, Koenen, Kovess-Masfety, Lee, Lepine, Mclaughlin, Medina-Mora, Navarro-Mateu, Ojagbemi, Posada-Villa, Sampson, Scott, Tachimori, Have, Kendler and Kessler2017) examined the prospective relationship between traumatic experiences and psychotic experiences in the World Mental Health Surveys, finding increasingly strong associations between traumatic experiences, and increasing number of traumatic experiences, and subsequent psychotic experiences, after adjusting for PTSD and a range of other psychiatric disorders. By assessing additive interaction between psychotic experiences and non-psychotic psychiatric disorders, we were able to compare the association between symptom comorbidities with psychotic experiences on public mental health outcomes, giving an indication of the possible importance of psychotic experiences in a clinical context with other, commonly occurring psychiatric symptoms.
Limitations
We were able to assess the interaction between non-psychotic psychiatric disorders with comorbid psychotic experiences for a range of mental disorders (including temporally prospective specialist mental health service use and use of psychological treatment), and good statistical evidence was found for our main comparisons. Nevertheless, our inferences could have been affected by chance – some association estimates were based on small numbers of participants. Models were identically specified for each outcome, aiding comparison. However, some confounders could have applied to certain outcomes more strongly than others. We had no information on timings, frequency or intensity of psychotic experiences. Measurement accuracy may have been influenced by the simultaneous assessment of psychopathology in the same survey assessment, e.g. depressed mood may have influenced the accuracy of psychotic experiences assessment, and vice versa. Confounding by unknown, unmeasured, or poorly measured/misreported characteristics is possible. Responders to health surveys tend to be healthier than the general population (Keyes et al., Reference Keyes, Rutherford, Popham, Martins and Gray2018), and so the true prevalence of mental health service use for comorbid psychotic experiences in the general population may be greater than that estimated here, although our analysis incorporated non-response weights which probably limited bias in estimates. Given the cross-sectional ascertainment of concurrent psychotic experiences, we were unable to identify or examine the temporal direction of associations between psychotic experiences and non-psychotic psychiatric disorders, although bi-directional relationships between psychotic experiences and other psychiatric disorders are evident in previous literature (McGrath et al., Reference Mcgrath, Saha, Al-Hamzawi, Andrade, Benjet, Bromet, Browne, Caldas De Almeida, Chiu and Demyttenaere2016). We were also unable to analyse direction of causal association between psychotic experiences and suicide attempt, or impairment of physical functioning. Although our characterisation of non-psychotic psychiatric disorders was not based on clinical interviews, we were able to derive ICD-10 diagnoses from the rating of psychiatric symptoms, based on accepted algorithms.
Explanations
Our findings underline the importance of taking account of non-psychotic psychopathology when assessing the impact of psychotic experiences on mental health (Bhavsar et al., Reference Bhavsar, Mcguire, Maccabe, Oliver and Fusar-Poli2018). The influence of psychotic experiences on help-seeking behaviour could be dependent on the other psychiatric symptoms that are experienced. For example, it is possible that psychotic experiences themselves are less severe in those with mild/moderate CMD compared to those with severe CMD, or that psychotic experiences raise the threshold at which individuals with mild/moderate CMD or anxiety seek help for mental disorders.
Frequent overlap between psychotic experiences and non-psychotic psychiatric disorders observed in the current study is consistent with a general psychopathological factor underlying psychiatric disorders, proposed by Caspi and supported by genetic, neuroimaging, and psychometric evidence (Klaassen et al., Reference Klaassen, Heins, Luteijn, Van Der Gaag and Van Beveren2013; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev and Poulton2014; Frangou, Reference Frangou2014). This continuity may also account for the occurrence of mood dysregulation during the development of psychosis, prior to onset of positive psychotic symptoms (Mishara and Fusar-Poli, Reference Mishara and Fusar-Poli2013). Our results support the possibility that psychotic experiences are non-specific markers of overall psychopathology, and indicate that psychotic experiences may be a relevant predictor of greater symptom burden, in line with current understanding of psychosis as a more burdensome psychiatric disorder in its own right. Given the strong associations of psychotic experiences concurrent with non-psychotic psychiatric disorders with service use and suicide attempts measured in this study, it is possible that concurrent psychotic experiences explain some of the public mental health need attributable to common psychiatric disorders in the general population.
The presence of psychotic experiences in a clinical presentation may be a marker of greater subsequent mental health need (Bhavsar et al., Reference Bhavsar, Maccabe, Hatch, Hotopf, Boydell and Mcguire2017), and our results indicate that this may also be true in the context of co-occurring non-psychotic psychiatric symptoms. Psychotic experiences could identify a higher risk group for population-based interventions to improve public mental health. The design of services could reflect the importance of psychotic experiences for the prognosis of CMDs, and symptoms of CMDs for the prognosis of psychotic conditions. Psychotic experiences could be a useful, relatively easy to measure indicator of later mental health need, which could be incorporated into prognostic tools for mental health service use at a population level, to guide commissioning of future services.
Acknowledgement
This paper represents independent research part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Financial support
This work was supported by a Wellcome Trust Clinical Research Training Fellowship, grant number 101681/Z/13/Z, awarded to Vishal Bhavsar. This work was also supported by the Economic and Social Research Council (Grant number RES-177-25-0015).
Conflict of interest
Funding declared: PFP has received grants funds from Lundbeck and honoraria fees from Lundbeck and Menarini. MH is principal investigator of RADAR-CNS, a private public pre-competitive consortium on remote sensing in depression, multiple sclerosis and epilepsy which includes research funding from five pharmaceutical companies (Janssen, MSD, UCB Biogen and Lundbeck).
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









