Introduction
Caesarean section rates have increased in many parts of the world (Betran et al., Reference Betran, Ye, Moller, Zhang, Gulmezoglu and Torloni2016), including the UK where around 30% of all births now occur by caesarean (Information Services Division Scotland, 2019; NHS Digital, 2019; Welsh Government, 2020). This has resulted in increasing numbers of pregnant women with a history of previous caesarean. Policy in many high-income countries supports giving such women a choice between planning another caesarean, known as an elective repeat caesarean section (ERCS) or planning a vaginal birth, known as a planned vaginal birth after previous caesarean (VBAC), provided they have no contraindications to VBAC. This contrasts with the general obstetric population in most high-income settings, where the majority of caesareans are performed because they are recommended for various obstetric or medical reasons. Clinical guidelines (American College of Obstetricians & Gynecologists, 2019; National Institute for Health & Clinical Excellence, 2011; Royal College of Obstetricians and Gynaecologists, 2015; The Royal Australian & New Zealand College of Obstetricians & Gynaecologists, 2015) advocate counselling women about the risks and benefits of planned VBAC compared to ERCS to help them make an informed decision about this choice. However, several significant limitations have been highlighted with the existing evidence (Guise et al., Reference Guise, Eden, Emeis, Denman, Marshall, Fu and McDonagh2010). These include uncertainty around whether women who would not have been advised to plan a VBAC due to obstetric/medical reasons were included in the ERCS group. There also remains a lack of evidence about certain outcomes, including the effect of planned mode of birth after previous caesarean on women's mental health.
Concerns have been raised that caesarean section may adversely affect women's mental health by, for example, restricting perceived control over birth, violating expectations about childbirth, disrupting physiological hormonal processes and leading to a more painful and difficult postnatal recovery (Buckley, Reference Buckley2015; Lobel & DeLuca, Reference Lobel and DeLuca2007). However, studies examining the association between mode of birth and women's mental health have reported mixed findings (Ayers, Bond, Bertullies, & Wijma, Reference Ayers, Bond, Bertullies and Wijma2016; Carter, Frampton, & Mulder, Reference Carter, Frampton and Mulder2006; Kendell, Chalmers, & Platz, Reference Kendell, Chalmers and Platz1987; Valdimarsdottir, Hultman, Harlow, Cnattingius, & Sparen, Reference Valdimarsdottir, Hultman, Harlow, Cnattingius and Sparen2009). This may partly reflect limitations with the existing studies, with many comprising small non-population-based studies that have focused on the effect of actual mode of birth without differentiating between planned and emergency caesarean despite the very different contexts in which these two types of caesarean are performed. Most previous studies have also not considered potential effects on mental health problems besides postnatal depression. Also, to our knowledge, only one small study of under 300 women (Law et al., Reference Law, Pang, Chung, Lao, Lee, Leung and Lau2010) conducted in a single hospital has to date specifically investigated the effect of planned mode of birth after previous caesarean on women's mental health, reporting no significant effects. Studies conducted in the general obstetric population may not be applicable to the situation of birth after previous caesarean as they are more prone to confounding by indication, where adverse outcomes may be a consequence of the underlying causes that led to the need for the caesarean. Furthermore, as certain serious birth-related complications such as uterine rupture, which may adversely affect women's mental health, predominately only occur or are increased following a planned VBAC (Fitzpatrick et al., Reference Fitzpatrick, Kurinczuk, Alfirevic, Spark, Brocklehurst and Knight2012; Fitzpatrick, Kurinczuk, Bhattacharya, & Quigley, Reference Fitzpatrick, Kurinczuk, Bhattacharya and Quigley2019), planned VBAC compared to ERCS may actually be associated with poorer subsequent maternal mental health.
Apart from providing further information to counsel women, the potential profound impact of maternal mental health problems on the woman, her infant and other family members (Slomian, Honvo, Emonts, Reginster, & Bruyere, Reference Slomian, Honvo, Emonts, Reginster and Bruyere2019), makes it important to better understand the aetiology and triggers for such problems to help identify potential targets for intervention. The aim of this study was to investigate the association between planned mode of birth after previous caesarean section and women's use of psychotropic medication in the first year postpartum as an indication of their subsequent risk of having treated mental health problems, among women giving birth to a singleton at term and considered clinically eligible to plan a VBAC.
Methods
Study design and data sources
A population-based cohort study was conducted using Scottish national datasets (online Supplementary Table S1) linked using exact matching of the community health index number, a unique person identifier used in Scotland. Online Supplementary Table S2 details the data sources, codes and database fields used.
Study population
All women with one or more previous caesareans who gave birth to a term (37–41 completed weeks gestation) singleton in Scotland, UK, between 1st January 2010 and 31st December 2015 were identified. Births to women not considered clinically eligible to plan a VBAC based on UK guidelines (National Institute for Health and Clinical Excellence, 2011; Royal College of Obstetricians and Gynaecologists, 2015) were excluded (online Supplementary Table S2). Births to women who had an antepartum stillbirth were also excluded as vaginal birth is usually recommended in this situation (Royal College of Obstetricians and Gynaecologists, 2010). To identify incident events of psychotropic drug use, women dispensed any of the primary outcome medications in the year before they gave birth were excluded. Women migrating to Scotland less than 1 year before they gave birth were also excluded to ensure information on history of psychotropic medication for at least 1 year before birth. Additional exclusions included stillbirths missing information about whether they occurred antenatally or during labour or birth, births missing information on mode of birth or gestational age at birth, births by non-elective caesarean section missing information about duration of labour, and births to women whose number of previous caesarean sections was greater than their recorded parity (online Supplementary Fig. S1). Each woman was followed up from the date they gave birth until the outcome of interest, date of emigration, death or 1 year after they gave birth, whichever came first.
Exposures
The primary exposure of interest was planned mode of birth after previous caesarean, with planned VBAC (birth vaginally or by non-elective caesarean with a duration of labour of ⩾1 h) compared to ERCS (birth by elective caesarean, defined by the Information Services Division Scotland as a caesarean performed during the day with both the patient and staff fully prepared).
Analysis was also performed according to whether planned VBAC was attempted with or without labour induction compared to ERCS, and was conducted according to actual mode of birth after previous caesarean, defined as follows: women recorded as having a vaginal birth were classified as having a VBAC; women recorded as having a non-elective caesarean with a duration of labour of ⩾1 h were classified as having an in-labour non-elective repeat caesarean and women recorded as having an elective caesarean were classified as having an ERCS.
Outcomes
The primary outcome was time to first dispensed prescription for any psychotropic medication within the first year postpartum, including medicines in any of the following ‘legacy’ British National Formulary (BNF) sections (Information Services Division Scotland, 2018): 4.3 ‘Antidepressant drugs’, used to treat a range of affective symptomatology including depressive disorders, anxiety disorders and mixed symptomatology; 4.1.1 ‘Hypnotics’, used to treat insomnia; 4.1.2 ‘Anxiolytics’, used to treat anxiety and 4.2 ‘Drugs used in psychoses and related disorders’.
Secondary outcomes included time to first dispensed prescription within the first year postpartum for specific categories of psychotropic medications, analysing antidepressants (BNF 4.3), hypnotics and/or anxiolytics (BNF 4.1.1 and/or 4.1.2) and drugs used in psychoses and related disorders (BNF 4.2) as three separate outcomes. We also examined at least two consecutive prescriptions for an antidepressant, where the first antidepressant was dispensed within the first year postpartum followed by at least one additional prescription for an antidepressant within 91 days of the first. Most antidepressants were dispensed over monthly intervals. A 91 day cut-off was used to allow for women decreasing their dosage for a period, using stored medication or late collection of a repeat prescription.
In the absence of data about the reason for prescribing, we attempted to exclude drugs likely to have been prescribed for indications other than mental health problems by excluding tricyclic antidepressants prescribed at a lower dose than the recommended BNF level for the treatment of depression (online Supplementary Table S2), as lower doses may be prescribed for other reasons such as chronic pain.
Statistical analysis
To investigate the association between the exposures and each outcome, Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). All models were adjusted for year of delivery to account for any temporal changes. Models were then adjusted in a hierarchical fashion for potential confounders determined a priori: model A adjusted for socio-demographic factors; model B additionally adjusted for maternal medical and pregnancy-related factors. Confounders were determined a priori based on pre-existing hypotheses or evidence on what factors are thought to potentially confound the relationship between the exposure and outcome in question (Field, Reference Field2018; Ghaedrahmati, Kazemi, Kheirabadi, Ebrahimi, & Bahrami, Reference Ghaedrahmati, Kazemi, Kheirabadi, Ebrahimi and Bahrami2017; Gregory et al., Reference Gregory, Korst, Fridman, Shihady, Broussard, Fink and Burnes Bolton2008; Guise et al., Reference Guise, Eden, Emeis, Denman, Marshall, Fu and McDonagh2010; O'Hara & McCabe, Reference O'Hara and McCabe2013), with a conceptual framework of how the factors might influence the relationship between planned mode of birth after previous caesarean and the outcomes considered outlined in online Supplementary Fig. S2. Breastfeeding may be on the causal pathway in that the exposures are associated with a woman's likelihood of breastfeeding (Fitzpatrick et al., Reference Fitzpatrick, Kurinczuk, Bhattacharya and Quigley2019), and breastfeeding may in turn influence a woman's likelihood of being dispensed psychotropic medication (Borra, Iacovou, & Sevilla, Reference Borra, Iacovou and Sevilla2015; Tripathi & Majumder, Reference Tripathi and Majumder2010). As we were interested in the effects of the exposures that were not mediated through breastfeeding an additional analysis was performed adjusting for whether the mother breastfed (exclusively or mixed) around 6–8 weeks postpartum (model C). We also examined if there was evidence of effect modification between the exposures and any breastfeeding at 6–8 weeks postpartum, in addition to investigating the number of prior caesareans and any prior vaginal birth as potential effect modifiers of the relationship between the primary exposure and outcomes. Effect modification was investigated by the addition of interaction terms to the full regression models. Adjustments were only performed when there was a minimum of 5–9 outcome events per coefficient in the model (Vittinghoff & McCulloch, Reference Vittinghoff and McCulloch2007).
Fractional polynomials were used to examine whether continuous covariates showed evidence of departure from linearity. A total of 24.7% of the study population has missing data on one or more of the covariates included in the fully adjusted models (see footnotes of Table 1 for more details). Multiple imputation using a recently developed extension to the chained equations approach was used (Bartlett, Seaman, White, & Carpenter, Reference Bartlett, Seaman, White and Carpenter2014) to impute partially observed covariates when there appeared from the complete case analysis to be evidence of non-linear covariate effects. Otherwise, the normal chained equations method was used to impute partially observed covariates including the event indicator and Nelson–Aalen estimator of the cumulative hazard in the imputation models (White, Royston, & Wood, Reference White, Royston and Wood2009) in addition to all covariates, and performing 30 imputations. None of the exposures of interest, but one or more of the covariates in some models appeared to violate the proportional hazards assumption assessed using Schoenfeld residuals and log–log plots in the complete case analysis. We decided not to model these covariates as time-varying covariates as this was not found to result in material differences to the exposure estimates. Robust standard errors were used to account for the lack of independence in the data of women who had more than one eligible birth in the study period.
Table 1. Characteristics of study cohort by planned mode of birth after previous caesarean section
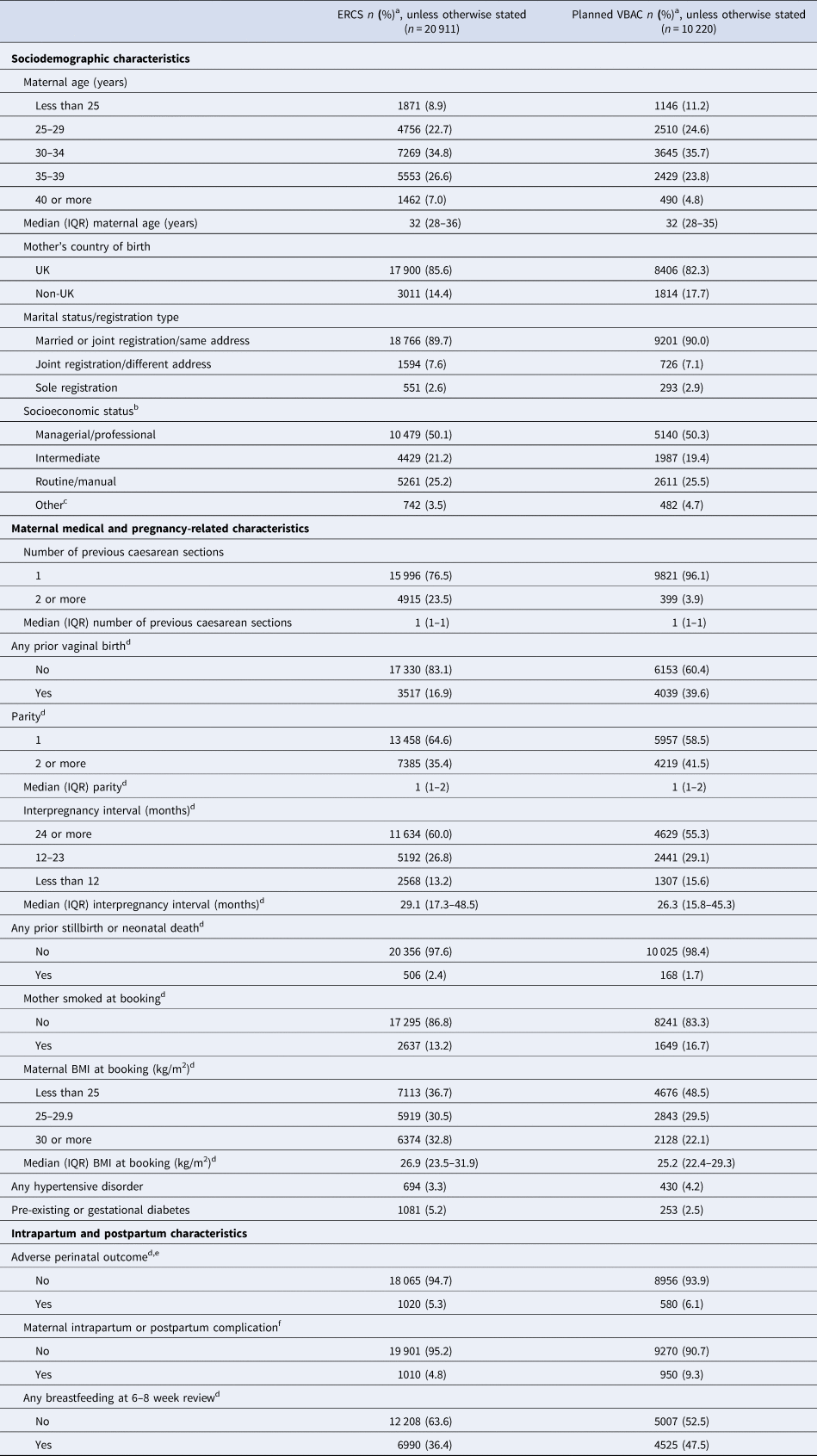
BMI, body mass index; ERCS, elective repeat caesarean section; IQR, interquartile range; NS-SEC, National Statistics Socio-Economic Classification; VBAC, vaginal birth after previous caesarean.
a Percentage of those with complete data.
b Socioeconomic status of mother for sole registered birth or highest of mother's or father's socioeconomic status for births registered inside marriage or jointly registered by both parents outside marriage. Socioeconomic status defined by NS-SEC based on occupation and employment status.
c Other includes never worked/long-term unemployed, student, not stated or not classifiable.
d Missing data: any prior vaginal birth 92 (0.30%); parity 112 (0.36%); interpregnancy interval 3360 (10.8%); any prior stillbirth or neonatal death 76 (0.24%); maternal smoking status 1309 (4.20%); maternal BMI 2078 (6.68%); adverse perinatal outcome 2510 (8.77%); any breastfeeding at 6–8 week review 2401 (7.71%).
e Adverse perinatal outcome includes intrapartum stillbirth or neonatal death, admission to a neonatal unit, resuscitation with drugs and/or intubation or an Apgar score <7 at 5 min.
f Intrapartum or postpartum complication includes uterine rupture, peripartum hysterectomy, blood transfusion, puerperal sepsis, other puerperal infection, surgical injury (damage to bowel, bladder or ureter requiring surgical repair), third- or fourth-degree perineal tear or overnight readmission to hospital within 42 days of birth.
A number of sensitivity analyses were conducted. First, a complete case analysis for each outcome studied. Second, given the potential of the way we defined planned mode of birth to misclassify women who planned ERCS but went into labour before their scheduled caesarean date, analyses were repeated restricted to births at ⩾39 weeks gestation. Since 2004, this is the gestation recommended by UK guidelines to perform an ERCS (National Institute for Health & Clinical Excellence, 2011; Royal College of Obstetricians & Gynaecologists, 2015). Third, analyses were repeated confined to women without a history of being dispensed any of the primary outcome medications in the 2 years before they gave birth. As the prescription information was only available from 2009, only eligible women who gave birth between 1st January 2011 and 31st December 2015 and did not migrate to Scotland less than 2 years before they gave birth were included in this analysis. Fourth, E-values were calculated to quantify the minimum strength of association that an unmeasured confounder would need with both the primary exposure and a given outcome to fully explain any observed associations between the primary exposure and outcomes conditional on the measured covariates (VanderWeele & Ding, Reference VanderWeele and Ding2017). All analyses were conducted in StataMP version 14 or 16.
Ethical approval
The study did not require ethics committee approval as it involved secondary analysis of anonymised data. However, approval for the study was obtained from the Public Benefit and Privacy Panel for Health and Social Care Scotland (application number 1516-0196).
Results
A total of 31 131 singleton term births to women with one or more previous caesareans met the study eligibility criteria (online Supplementary Fig. S1). Overall, 32.8% (10 220) of the women had a planned VBAC and 67.2% (20 911) had an ERCS. The ERCS rate increased over the study period from 64.5% in 2010 to 71.9% in 2015. Women who had a planned VBAC were more likely than those who had an ERCS to be younger, born outside the UK and have a lower socio-economic status (Table 1). They were also more likely to have had just one prior caesarean section, one or more previous vaginal births, a shorter inter-pregnancy interval, be smokers at booking for pregnancy care, have a hypertensive disorder, experienced an adverse perinatal outcome or maternal intrapartum or postpartum complication and have breastfed at 6–8 weeks postpartum. They were less likely than those who had an ERCS to have experienced a prior stillbirth or neonatal death, be overweight or obese or to have diabetes.
Less than 1% of the study population was lost to follow-up because of emigration or death, with these women contributing person-years up to the date of loss. During 29 097 person-years of follow-up, 3585 (11.5%) of the study population were dispensed at least one prescription for any psychotropic medication. Antidepressants were the most common type of psychotropic medication dispensed, with 9.9% of women dispensed an antidepressant, 2.9% dispensed a hypnotic and/or anxiolytic and 0.20% dispensed an antipsychotic and/or related drug. Crude rates of first dispensed prescription for any psychotropic medication, an antidepressant and at least two consecutive antidepressants peaked around month 2 to 3 following childbirth, whereas crude rates of first dispensed prescription for a hypnotic and/or anxiolytic or an antipsychotic and/or related drug remained fairly constant over the follow-up period (online Supplementary Fig. S3).
Outcomes according to planned mode of birth are shown in Table 2 and Fig. 1a. Having only adjusted for year of delivery, women who planned a VBAC had a significantly lower risk than those giving birth by ERCS of being dispensed any psychotropic medication (HR 0.80, 95% CI 0.75–0.87) and all categories of psychotropic medication (antidepressant: HR 0.78, 95% CI 0.72–0.85; at least two consecutive antidepressants: HR 0.76, 95% CI 0.69–0.83 and hypnotic and/or anxiolytic 0.85, 95% 0.74–0.99) except for antipsychotic and/or related drugs (HR 1.54, 95% CI 0.94–2.52). Adjustment for socio-economic factors and maternal medical and pregnancy-related factors had little material effect on the effect estimates. Adjusting for any breastfeeding at 6–8 weeks postpartum slightly attenuated all the effect estimates, but the risk of being dispensed any psychotropic medication [adjusted HR (aHR) 0.85, 95% CI 0.78–0.92], an antidepressant (aHR 0.83, 95% CI 0.76–0.90) and at least two consecutive antidepressants (aHR 0.83, 95% CI 0.75–0.91) remained significantly lower in women who planned a VBAC compared to giving birth by ERCS.
Table 2. Outcomes following planned VBAC compared to ERCS

BMI, body mass index;CI, confidence interval; ERCS, elective repeat caesarean section; HR, hazard ratio; NC, not calculated because of low number of events; VBAC, vaginal birth after previous caesarean.
a Base model adjusted for year of delivery only.
b Model A adjusted for year of delivery and socio-demographic factors (maternal age, mother's country of birth, marital status and socio-economic status).
c Model B adjusted for variables in model A and additionally adjusted for maternal medical and pregnancy-related factors (number of previous caesarean sections, any prior vaginal birth, inter-pregnancy interval, any prior stillbirth or neonatal death, maternal smoking status at booking, maternal BMI at booking, hypertensive disorder and diabetes).
d Model C, adjusted for variables in model B and additionally adjusted for any breastfeeding at 6–8 weeks postpartum.
Bold text indicates statistically significant findings at the 5% level.

Fig. 1. Outcomes following (a) planned VBAC compared to ERCS, (b) planned VBAC without labour induction compared to ERCS, (c) planned VBAC with labour induction compared to ERCS, (d) planned and actually had VBAC compared to ERCS and (e) planned VBAC but had in-labour non-elective repeat caesarean section compared to ERCS. §Dispensed an antipsychotic and/or related drug only adjusted for year of delivery and socio-demographic factors (maternal age, mother's country of birth, marital status and socio-economic status) because of low number of events, whereas other outcomes were adjusted for year of delivery and socio-demographic factors (maternal age, mother's country of birth, marital status and socio-economic status), maternal medical and pregnancy-related factors (number of previous caesarean sections, any prior vaginal birth, inter-pregnancy interval, any prior stillbirth or neonatal death, maternal smoking status at booking, maternal BMI at booking, hypertensive disorder and diabetes) and breastfeeding at 6–8 weeks postpartum. BMI, body mass index; ERCS, elective repeat caesarean section; HR, hazard ratio; VBAC, vaginal birth after previous caesarean.
Of the women who planned a VBAC, 19.3% (1960/10 180) had their labour induced (30.3% using surgical induction alone, 33.5% using medical induction alone and 34.7% using surgical and medication induction). Outcomes by whether planned VBAC was attempted with or without labour induction compared to ERCS (Table 3 and Fig. 1b and c) were very similar to those reported for planned VBAC compared to ERCS. Compared to the women who gave birth by ERCS, women who planned a VBAC with or without labour induction had a significantly reduced risk of being dispensed any psychotropic medication even having adjusted for breastfeeding (aHR 0.86, 95% CI 0.74–1.00 and aHR 0.85, 95% CI 0.78–0.92, respectively). There was also evidence that women who planned a VBAC with or without labour induction had a reduced risk of being dispensed an antidepressant and at least two consecutive antidepressants. However, for women who planned a VBAC with labour induction these effects were not statistically significant having adjusted for breastfeeding noting the smaller number of women in this subgroup.
Table 3. Outcomes following planned VBAC with and without labour induction compared to ERCS

BMI, body mass index; CI, confidence interval; ERCS, elective repeat caesarean section; HR, hazard ratio; NC, not calculated because of low number of events; VBAC, vaginal birth after previous caesarean.
a Base model adjusted for year of delivery only.
b Model A adjusted for year of delivery and socio-demographic factors (maternal age, mother's country of birth, marital status and socio-economic status).
c Model B adjusted for variables in model A and additionally adjusted for maternal medical and pregnancy-related factors (number of previous caesarean sections, any prior vaginal birth, inter-pregnancy interval, any prior stillbirth or neonatal death, maternal smoking status at booking, maternal BMI at booking, hypertensive disorder and diabetes).
d Model C, adjusted for variables in model B and additionally adjusted for any breastfeeding at 6–8 weeks postpartum.
Bold text indicates statistically significant findings at the 5% level.
Of the women who planned a VBAC, 71.6% (7314/10 220) went on to have a VBAC and 28.4% (2906/10 220) went on to have an in-labour non-elective repeat caesarean. Compared to the women who gave birth by ERCS, both the women who actually had a VBAC and the women who gave birth by in-labour non-elective repeat caesarean had a reduced risk of being dispensed any psychotropic medication, an antidepressant and at least two consecutive antidepressants. However, for women who had an in-labour non-elective repeat caesarean the effect sizes were weaker and not statistically significant in the fully adjusted models (Table 4 and Fig. 1d and e). Women giving birth by in-labour non-elective repeat caesarean had a significantly increased risk compared to those giving birth by ERCS of being dispensed an antipsychotic and/or related drug having adjusted for year of delivery alone or year of delivery in addition to socio-demographic factors. However, due to the low number of outcome events it was not possible to adjust for additional factors that may influence this association.
Table 4. Outcomes according to actual mode of birth – planned and actually had a VBAC and planned VBAC but had in-labour non-elective repeat caesarean section compared to ERCS
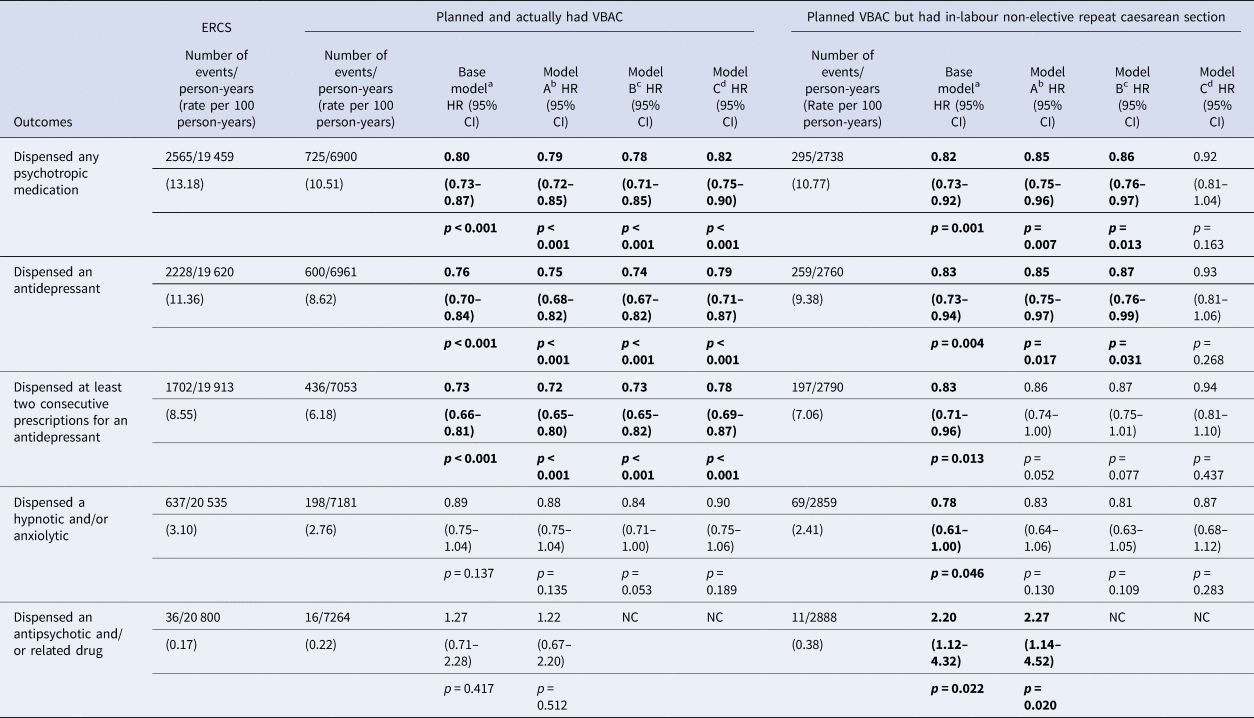
BMI, body mass index; CI, confidence interval; ERCS, elective repeat caesarean section; HR, hazard ratio; NC, not calculated because of low number of events; VBAC, vaginal birth after previous caesarean.
a Base model adjusted for year of delivery only.
b Model A adjusted for year of delivery and socio-demographic factors (maternal age, mother's country of birth, marital status and socio-economic status).
c Model B adjusted for variables in model A and additionally adjusted for maternal medical and pregnancy-related factors (number of previous caesarean sections, any prior vaginal birth, inter-pregnancy interval, any prior stillbirth or neonatal death, maternal smoking status at booking, maternal BMI at booking, hypertensive disorder and diabetes).
d Model C, adjusted for variables in model B and additionally adjusted for any breastfeeding at 6–8 weeks postpartum.
Bold text indicates statistically significant findings at the 5% level.
Examining the associations by breastfeeding status at 6–8 weeks postpartum, the effects of planned VBAC, planned VBAC without labour induction and actual VBAC were still evident in women who did and did not breastfeed with no evidence of effect modification between the exposures and breastfeeding status (online Supplementary Fig. S4). There was also no evidence of effect modification between the primary exposure and the number or prior caesareans a woman had, or whether the woman had any prior vaginal birth. The sensitivity analyses presented in online Supplementary Tables S3–S11 resulted in similar effect estimates, although the significance of some of the associations varied noting these analyses included a smaller number of women. The E-values suggest that relatively modest unmeasured confounding could fully explain the observed associations between the primary exposure and outcomes (online Supplementary Table S12). For example, to fully explain the observed HR of 0.85 for any psychotropic medication, an unmeasured confounder would need to be associated with at least a 1.63-fold increased risk for both the primary exposure and outcome through pathways independent of the covariates included in the fully adjusted model; to move the upper CI to include the null, an unmeasured confounder would need to be associated with at least a 1.39-fold increased risk for both the primary exposure and outcome, above and beyond the measured covariates.
Discussion
Among women considered clinically eligible to plan VBAC without a history of psychotropic drug use in the year before birth, planned VBAC compared to ERCS was associated with a 15% reduced risk of the mother being dispensed any psychotropic medication and a 17% reduced risk of the mother being dispensed an antidepressant and at least two consecutive antidepressants in the first year postpartum. These findings were adjusted for many potential confounders as well as breastfeeding at 6–8 weeks postpartum, a potential mediating factor.
Strengths and limitations of study
Strengths of this study include its large population-based design with very little loss to follow-up, which reduces the risk of selection bias and maximises statistical power. Other strengths include confining the study to women who were considered clinically eligible to plan a VBAC based on current UK guidelines, and the use of prospectively collected routine data which avoids recall bias. We were also able to explore the influence of many a priori potential confounders as well as the influence of breastfeeding, a potential mediating factor. However, similar to other observational studies, we cannot rule out residual confounding due to unmeasured confounding factors that we have not been able to consider such as indication for the previous caesarean. The reported E-values suggest that relatively modest unmeasured confounding could fully explain the observed associations. However, it is worth noting that in the absence of conducting a large randomised trial, which a previous study (Crowther, Dodd, Hiller, Haslam, & Robinson, Reference Crowther, Dodd, Hiller, Haslam and Robinson2012) indicates is unlikely to be feasible, large population-based observational studies with the ability to consider multiple covariates, such as our study, offer the best opportunity to inform evidence in this area.
Inferring treated mental health problems only from dispensed prescriptions of psychotropic medication is a limitation of our study. Our study is likely to have underestimated the proportion of women with treated mental health problems in the first year postpartum, as while psychotropic medication tends to be the most commonly used type of mental health treatment (McManus, Bebbington, Jenkins, & Brugha, Reference McManus, Bebbington, Jenkins and Brugha2016; Petersen, Peltola, Kaski, Walters, & Hardoon, Reference Petersen, Peltola, Kaski, Walters and Hardoon2018), other treatments, most notably psychological interventions, may be offered. There may also be a higher threshold in the postnatal period for using psychotropic medication amid concerns about the safety of these drugs for the breastfed baby (Tripathi & Majumder, Reference Tripathi and Majumder2010), noting, however, that our effects were still evident in women who did and did not breastfeed with no evidence that breastfeeding modified the effects of the exposures. We also did not have information about whether women actually took the dispensed medication or the indication for the medication. We also acknowledge that excluding women dispensed psychotropic drugs in the year, or 2 years in the case of the sensitivity analysis (online Supplementary Tables S9–S11), before they gave birth would have been unlikely to have excluded all women with previous mental health problems linked to the points raised above and the fact that not all women with mental health problems will present for treatment (McManus et al., Reference McManus, Bebbington, Jenkins and Brugha2016). Although the time when psychotropic drugs are most likely to be stopped is around the time of pregnancy recognition and restarting treatment in pregnancy is not uncommon (Petersen et al., Reference Petersen, McCrea, Sammon, Osborn, Evans, Cowen and Nazareth2016), we may also have not excluded all women with previous mental health problems as some women may have discontinued psychotropic drugs when trying to conceive. Furthermore, some women develop mental health problems de novo during pregnancy and remain untreated or are not treated with medication. However, this would only have biased the results if the proportion of women with either untreated or non-pharmacologically treated mental health problems before birth differed between those who planned a VBAC and those that had an ERCS.
We acknowledge the performance of multiple comparisons would have increased the risk of type 1 error, although using a more stringent p value to allow for multiple testing would not have altered our main findings. The amount of missing data on one or more of the covariates is recognised as another limitation. However, our use of multiple imputation is regarded as a valid method for dealing with this problem provided the unobserved data are missing at random and the models to impute the missing data have been correctly specified (Nguyen, Carlin, & Lee, Reference Nguyen, Carlin and Lee2017).
Comparison with other studies and interpretation
To our knowledge, only one small study of under 300 women (Law et al., Reference Law, Pang, Chung, Lao, Lee, Leung and Lau2010) conducted in a single hospital in Hong Kong has to date investigated the effect of planned VBAC compared to ERCS on women's mental health. This prior study used psychometric tests during pregnancy and up to 6 months postpartum to assess anxiety, depression and general psychological wellbeing, reporting no significant differences between women who planned a VBAC compared to an ERCS. Consistent with our findings, another small study of 169 Australian women with one previous caesarean found that women who had a spontaneous vaginal birth were less likely than those giving birth by planned or emergency repeat caesarean or instrumental vaginal birth to have symptoms suggestive of postnatal depression (Shorten & Shorten, Reference Shorten and Shorten2012). More recently, and again consistent with our findings, a study of nearly 900 women conducted in 15 maternity units in Europe reported that compared to women who had an emergency or planned repeat caesarean, women who had a spontaneous vaginal birth after one previous caesarean had higher postnatal health-related quality of life scores encompassing physical, psychological and social dimensions of health (Fobelets et al., Reference Fobelets, Beeckman, Buyl, Daly, Sinclair, Healy and Putman2018). A further analysis of the same study population found that women with an antenatal preference for vaginal birth who gave birth by ERCS had lower postnatal health-related quality of life scores compared to women with an antenatal preference for vaginal birth who actually gave birth vaginally (Fobelets et al., Reference Fobelets, Beeckman, Buyl, Healy, Grylka-Baeschlin, Nicoletti and Putman2019). Our effect sizes were stronger in women who planned and actually had a VBAC than in women who planned but had an in-labour non-elective repeat caesarean, supporting the potential importance of a match between preferred and actual mode of birth on women's wellbeing.
Although more studies have been conducted in the general obstetric population, as mentioned in the Introduction, these studies may not be applicable to women with previous caesarean and most have focused on the effect of actual mode of birth on postnatal depression. Caesarean section has been reported to be both protective of and a risk factor for postnatal depression (Carter et al., Reference Carter, Frampton and Mulder2006). A limited number of studies have also reported caesarean section to be a risk factor for postpartum psychosis (Kendell et al., Reference Kendell, Chalmers and Platz1987) and anxiety disorders such as post-traumatic stress disorder (Ayers et al., Reference Ayers, Bond, Bertullies and Wijma2016). However, other studies have not found a significant association between mode of birth and these outcomes or have only found an association in women with a previous history of mental health problems (Carter et al., Reference Carter, Frampton and Mulder2006; Valdimarsdottir et al., Reference Valdimarsdottir, Hultman, Harlow, Cnattingius and Sparen2009). These inconsistencies in findings may partly reflect limitations with the existing studies, with many comprising small non-population-based studies that have not differentiated between planned and emergency caesarean despite the very different contexts in which these two types of caesarean are performed. Unplanned in contrast to planned caesareans are often carried out with little time for women to prepare themselves and are frequently accompanied by concerns around the safety of the mother and/or her baby. A recent meta-analysis of a small number of studies that did distinguish between type of caesarean, reported that unplanned but not planned caesareans were associated with an increased risk of postnatal depression (Xu, Ding, Ma, Xin, & Zhang, Reference Xu, Ding, Ma, Xin and Zhang2017).
Mode of birth may affect the mother's postnatal wellbeing by influencing the likelihood of the mother or baby experiencing birth-related complications. However, our study found that despite being more likely to experience a range of adverse perinatal and maternal intrapartum or postpartum outcomes (Fitzpatrick et al., Reference Fitzpatrick, Kurinczuk, Bhattacharya and Quigley2019), women who planned a VBAC were less likely than those giving birth by ERCS to be dispensed psychotropic medication including antidepressants in the first year postpartum. This may be because women who planned a VBAC were less likely than those having an ERCS to seek treatment for mental health problems or were less likely to be offered and/or accept pharmacological treatment in the first year postpartum. Our findings may alternatively imply that women giving birth by ERCS are more likely than those having a planned VBAC to experience mental health problems severe enough to warrant pharmacological treatment, at least in the year after birth. This may arise through several potential mechanisms. Women giving birth by caesarean are more likely to express not feeling in control over their birth, may be more likely to have their expectations about childbirth violated, even in the case of planned caesarean and may experience a more painful and difficult postnatal recovery, all of which may adversely affect their subsequent mental health (Lobel & DeLuca, Reference Lobel and DeLuca2007). Caesarean birth may also adversely impact maternal mental health by disrupting physiological hormonal processes such as the release of oxytocin, a hormone which helps to reduce stress, increase sociability and maternal–infant attachment (Buckley, Reference Buckley2015). Although we excluded women with a history of psychotropic drug use in the 1–2 years before birth, we also cannot rule out that the possible increased likelihood of mental health problems in women giving birth by ERCS may be due to more prior psychiatric vulnerability in this group of women. Indeed, there is some evidence that women with a preference for elective caesarean are more likely to have a fear of childbirth, which in itself is thought to be associated with mental health problems (Saisto & Halmesmaki, Reference Saisto and Halmesmaki2003). It is also possible that women who plan VBAC may be more motivated and have personality traits associated with better mental health.
Conclusions
This study found that among women considered clinically eligible to plan VBAC without a history of psychotropic drug use in the year before birth, planned VBAC compared to ERCS was associated with a reduced risk of the mother being dispensed psychotropic medication including antidepressants in the first year postpartum. Our findings should not be extrapolated to the general obstetric population, where the majority of caesareans in high-income countries are recommended for obstetric or medical reasons rather than reflective of women's choice. Rather, our findings are likely to be generalisable to women with previous caesarean section giving birth to a term singleton in other high-income countries with similar population characteristics and clinical practice. Further research is needed to establish if our findings reflect a causal increase in the likelihood of postnatal mental health problems in women giving birth by ERCS compared to planned VBAC or whether there are other reasons behind our findings, particularly as an increasing number of women in many countries face a choice about how to plan to give birth after previous caesarean.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720005322
Acknowledgements
The authors would like to acknowledge the support of the eDRIS Team (National Services Scotland) for their involvement in obtaining approvals and provisioning and linking data and the use of the secure analytical platform within the National Safe Haven.
Financial support
KEF is funded by a National Institute for Health Research (NIHR) Doctoral Research Fellowship (DRF-2016-09-078) for this research project. This paper presents independent research. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Conflict of interest
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: KEF had financial support from the National Institute for Health Research (NIHR) for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.










