Studies have found historically high levels of mild to moderate psychiatric symptoms (Holingue et al., Reference Holingue, Badillo-Goicoechea, Riehm, Veldhuis, Thrul, Johnson and Kalb2020a; Holingue et al., Reference Holingue, Kalb, Riehm, Bennett, Kapteyn, Veldhuis and Thrul2020b; Holman, Thompson, Garfin, & Silver, Reference Holman, Thompson, Garfin and Silver2020) and serious psychological distress (SPD) (Breslau et al., Reference Breslau, Finucane, Locker, Baird, Roth and Collins2021a, Reference Breslau, North, Finucane, Roth and Collins2021b; McGinty, Presskreischer, Han, & Barry, Reference McGinty, Presskreischer, Han and Barry2020) in the US general population during the early period of the COVID-19 pandemic. These findings were not surprising, given what is known about mental health in the immediate aftermath of natural disasters (Bromet & Dew, Reference Bromet and Dew1995; Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020; Goldmann & Galea, Reference Goldmann and Galea2014; North, Reference North2016; Pfefferbaum & North, Reference Pfefferbaum and North2020) and the similarity of the early pandemic period to a natural disaster with respect to disruption of daily routines and financial and other hardships (Raker, Zacher, & Lowe, Reference Raker, Zacher and Lowe2020). Longitudinal or repeated-cross-sectional studies in the UK (Kwong et al., Reference Kwong, Pearson, Adams, Northstone, Tilling, Smith and Timpson2021; Proto & Quintana-Domeque, Reference Proto and Quintana-Domeque2021), Switzerland (Shanahan et al., Reference Shanahan, Steinhoff, Bechtiger, Murray, Nivette, Hepp and Eisner2020), and Japan (Kikuchi et al., Reference Kikuchi, Machida, Nakamura, Saito, Odagiri, Kojima and Inoue2020) have found similar patterns, although there is heterogeneity across international studies of the mental health impact of the pandemic (Prati & Mancini, Reference Prati and Mancini2021). Less is known about the persistence or emergence of clinically significant mental health conditions with longer duration of the pandemic and their relationships with multiple potential risk factors, including pre-disaster mental health, socioeconomic status, and stressful experiences during the disaster.
In this study, we examine the risk for SPD, a screening indicator of a clinically significant psychiatric condition, in a longitudinally followed cohort, assessed initially about one year prior to the pandemic (February 2019) and twice during the pandemic (May and August 2020). Prior studies have found that pre-pandemic mental health was a strong predictor of SPD early in the pandemic (Breslau et al., Reference Breslau, Finucane, Locker, Baird, Roth and Collins2021a, Reference Breslau, North, Finucane, Roth and Collins2021b), as has been found in prior disasters (North, Reference North2016), but associations of pre-pandemic mental health with stressful experiences during the pandemic have not been considered as a factor influencing mental health during the pandemic. Studies of post-disaster mental health have identified both pre-disaster socioeconomic status and specific stressful and preventable experiences during disasters as predictors of poor mental health outcomes (Galea et al., Reference Galea, Brewin, Gruber, Jones, King, King and Kessler2007) but have not considered the influence of pre-disaster mental health. Of particular interest with respect to the pandemic are widely experienced and unequally distributed experiences of disruption in employment (Gemelas, Davison, Keltner, & Ing, Reference Gemelas, Davison, Keltner and Ing2021; Montenovo et al., Reference Montenovo, Jiang, Rojas, Schmutte, Simon, Weinberg and Wing2020), childcare (Sevilla & Smith, Reference Sevilla and Smith2020), and healthcare (Fischer, Uscher-Pines, Roth, & Breslau, Reference Fischer, Uscher-Pines, Roth and Breslau2021). Longitudinal studies, which are rare following disasters (Parker, Edelman, Carman, & Finucane, Reference Parker, Edelman, Carman and Finucane2020), are needed to assess the contributions of these multiple potential sources of risk.
Methods
Sample
Data come from a survey conducted using the American Life Panel (ALP), a probability-based panel of US adults age 20 and over who are regularly interviewed over the Internet (Pollard & Baird, Reference Pollard and Baird2017). ALP participants are provided with laptops and/or a broadband connection to ensure population representation. The baseline (T1) survey was administered between February and April of 2019; 2555 out of 3932 invited respondents completed the survey for a participation rate of 65%. Of the baseline sample, 1870 (73.2%) completed the T2 survey in May 2020 and 1751 (68.5%) completed the T3 survey in August 2020.
Final sample weights were calculated as the product of survey weights and attrition weights. We generated the survey weights using the raking algorithm survwgt rake in Stata 16.1 to match the sample demographic characteristics to the 2020 Annual Social and Economic Supplement of the Current Population Survey. We matched on the joint distributions of race by gender, educational attainment by gender, age by gender, and household income by household size (Pollard & Baird, Reference Pollard and Baird2017). Prior to the application of the attrition weights, the characteristics of those who completed all three surveys are statistically different with respect to age, race/ethnicity, and household income but not with respect to SPD from those who did not respond at T2 or T3. We generated the attrition weights using inverse probability weights of being in all waves, generated using a logistic regression of inclusion in the T2 and T3 samples on the baseline outcome (in T1), family income, educational attainment, age, gender, and race/ethnicity. The survey had low item-level missingness; chained equations single imputation was used to replace missing item responses. All study procedures were approved by the RAND IRB. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Assessments
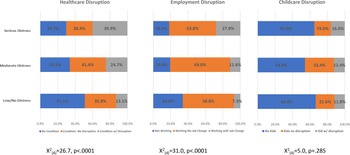
The longitudinal design is shown in Fig. 1. At T1, past-year SPD was assessed using the Kessler-6 (K6) (Kessler et al., Reference Kessler, Barker, Colpe, Epstein, Gfroerer, Hiripi and Zaslavsky2003), a measure of non-specific psychological distress calibrated using structured clinical follow-up interviews to identify clinically significant psychiatric conditions (Furukawa, Kessler, Slade, & Andrews, Reference Furukawa, Kessler, Slade and Andrews2003; Kessler et al., Reference Kessler, Andrews, Colpe, Hiripi, Mroczek, Normand and Zaslavsky2002). K6 scores were classified using established cutpoints as no/low distress (K6<8), mild/moderate distress (7 < K6<13), and serious distress (K6>12) (Kessler et al., Reference Kessler, Green, Gruber, Sampson, Bromet, Cuitan and Zaslavsky2010). We include demographic information with the T1 assessment, although information on household income was updated according to a pre-planned schedule in January of 2020. Internal consistency (coefficient α) was 0.87 at T1 and 0.75 at T3.
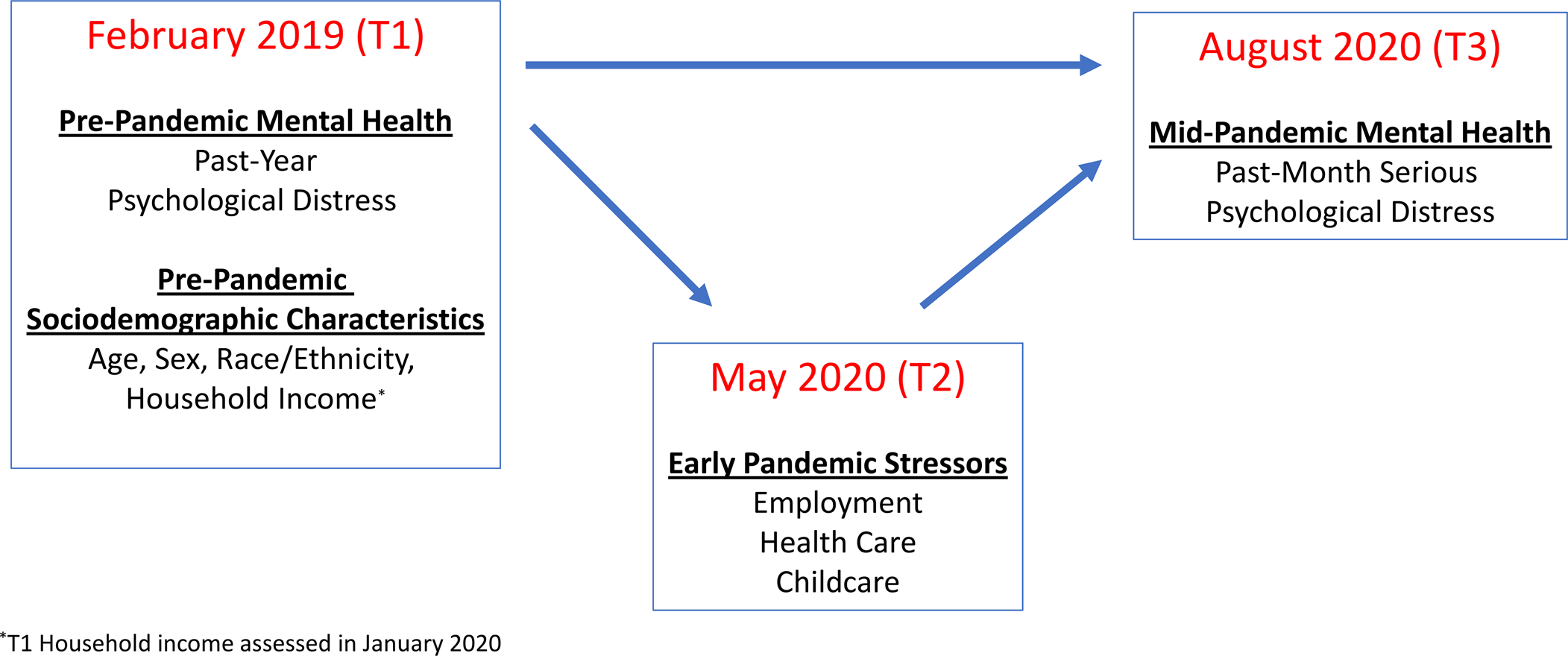
Fig. 1. Study design.
At T2, exposure to stressors related to the disruption of employment, health care, and childcare due to the COVID-19 pandemic was assessed as described below.
Employment: Respondents were asked if they were working when the pandemic began, and, if so, whether they had experienced a job change since the pandemic began. In preliminary analyses, job change was strongly associated with loss of income, so it can be assumed that job changes were overwhelmingly negative. Comparisons were made between those who experienced a job change, those who were employed during the pandemic and did not experience a job change, and those who were not working during the pandemic.
Health care: Respondents were asked if they were receiving health care for a physical or behavioral health condition when the pandemic began or had a need for care arise during the pandemic (Fischer et al., Reference Fischer, Uscher-Pines, Roth and Breslau2021). Those with either health care need during the pandemic were asked whether their care had been disrupted. Comparisons were made between those with a health care need whose care was disrupted, those with a health care need whose care was not disrupted, and those with no health care need.
Childcare: Respondents with children in their household were asked if their children's school or childcare had been disrupted during the pandemic. Comparisons were made between those with children whose childcare had been disrupted, those with children whose childcare had not been disrupted, and those without children.
At T3, SPD was assessed using the K6 with a past-month timeframe. The primary outcome was SPD (K6>12) at T3.
Statistical analysis
All analyses were conducted using survey procedures in SAS or Stata to account for the ALP sample design and weights. Associations of demographic characteristics with SPD at T1 were assessed with χ 2 tests. For each of the three T2 stressors, we defined a three-level outcome with one level indicating the absence of risk for the outcome (e.g. no children in the household for the childcare outcome), one level indicating risk without the outcome (e.g. children in the household but no disruption of childcare) and one level indicating risk and the presence of the outcome (e.g. children in the household and disruption of childcare). Associations of SPD at T1 with the T2 stressors were then examined using χ 2 tests and multinomial logistic regressions to account for sociodemographic characteristics at T1. Binary logistic regressions were used to assess the associations of SPD and demographic characteristics at T1 and experiences of stressors at T2 with SPD at T3. In binary logistic regressions, the outcome was SPD, i.e. K6>12 v. K6⩽12.
To more formally evaluate the model in Fig. 1 and test for the indirect pathways in which T1 SPD impacts T3 SPD, we estimate a generalized structural equation model (SEM) using probit link functions and with the survey weights used for the other models. We examine the standardized coefficients and estimates of the indirect effects to determine both the relative importance of indirect v. direct pathways as well as which mediating pathways have the largest total association with the outcome (MacKinnon, Fairchild, & Fritz, Reference MacKinnon, Fairchild and Fritz2007).
Results
At T1, SPD was significantly associated with age, race/ethnicity, and household income with higher distress among those with younger age, Non-Hispanic Black and Non-Hispanic white race/ethnicity, and lower household income (Table 1).
Table 1. Association of demographic characteristics and serious psychological distress at baseline (T1)
The baseline survey was conducted in February 2019. Psychological distress was assessed with the K6. Scores of 8–12 were considered moderate and scores of 13 or higher were considered serious.
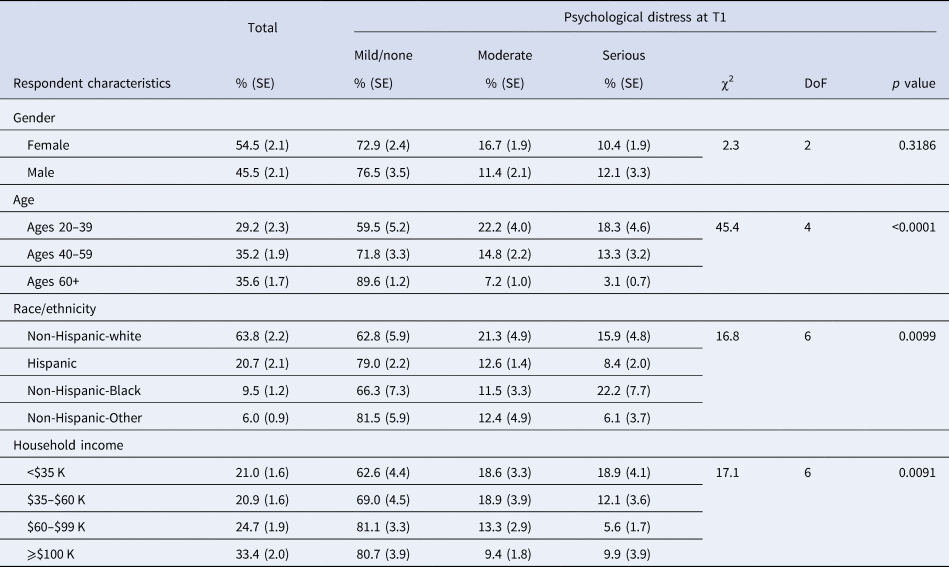
SPD at T1 was associated with the experience of stressors at T2 including disruption in employment and healthcare, but not in childcare (Fig. 2). People with serious distress at T1 were more likely to have a medical condition and more likely to have experienced disruption of health care at T2 than those with lower distress at T1. Similarly, those with higher distress at T1 were more likely to be working and more likely to have experienced a job change at T2 than those with lower levels of distress at T1. However, there was not a significant relationship between SPD at T1 and childcare disruption at T2.
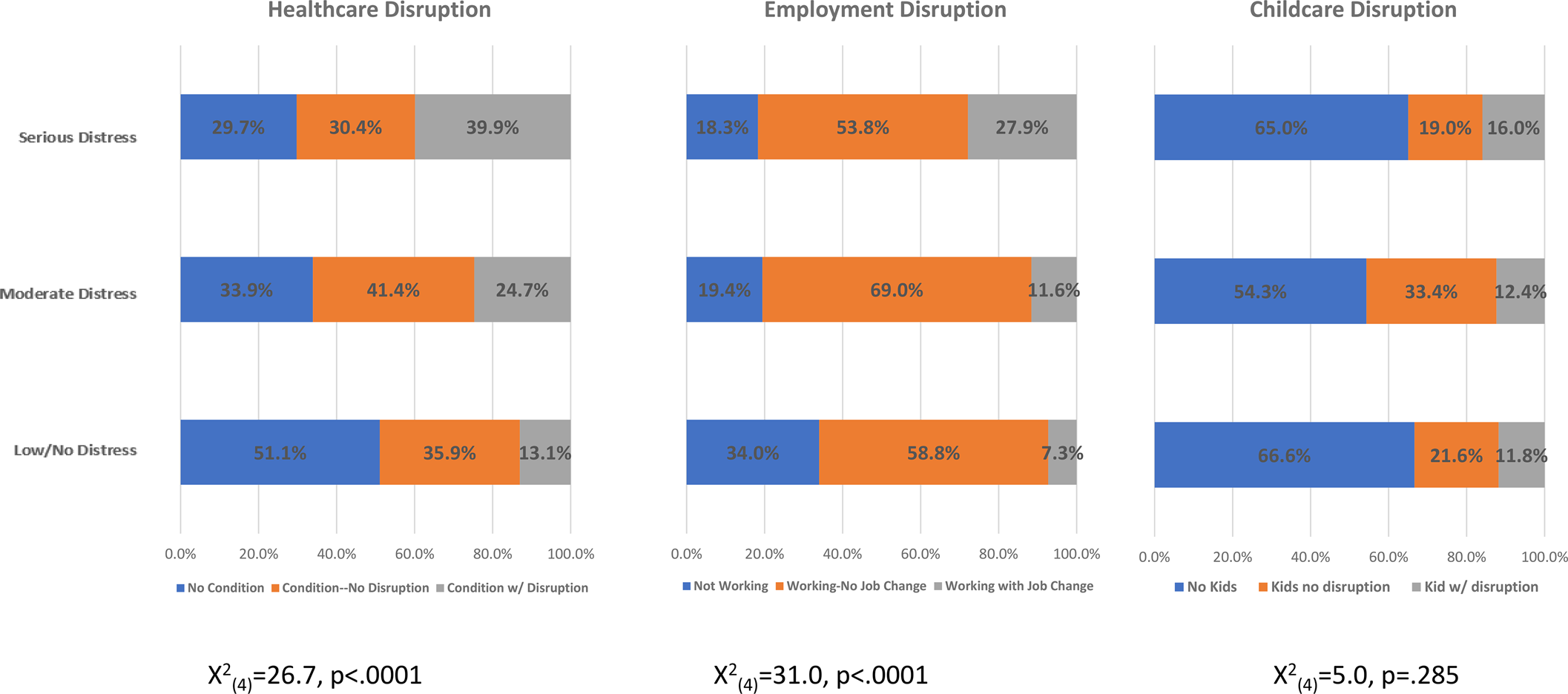
Fig. 2. Psychological distress at T1 and stressors at T2.
We estimated multinomial logistic regression models to examine the associations of SPD at T1 with the disruption of employment, healthcare, and childcare at T2, with adjustment for T1 demographic characteristics (Table 2). Adjustment for these demographic characteristics did not change the overall results. After adjustment for gender, age, race/ethnicity, and household income, SPD at T1 was associated with higher odds of employment disruption among those employed at T2 (OR 4.45, 95% CI 1.44–3.75) and with health care disruption among those with health conditions at T2 (OR 3.15, 95% CI 1.41–7.05). The association between SPD at T1 and disruption of childcare at T1 among those with children in the household was elevated but did not reach statistical significance (OR 2.16, 95% CI 0.58–8.09).
Table 2. Association of pre-pandemic sociodemographic characteristics and serious psychological distress with experience of stressors early in the pandemic
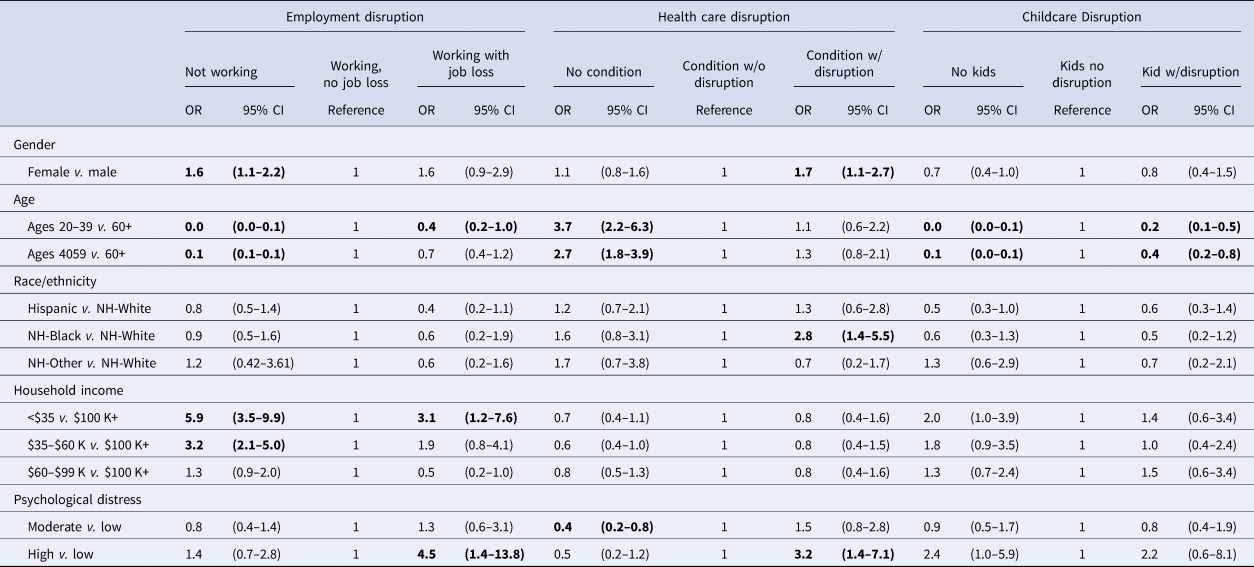
OR, odds ratio; NH, Non-Hispanic. ORs estimated in multinomial logistic regression models.
ORs >1 indicate higher risk of the outcome for the predictor category compared to the risk for the reference outcome for that predictor category. Bold text indicates ORs that are significantly different from 1 at the p = 0.05 level.
Results from the logistic regression of SPD at T3 on T1 demographic characteristics and psychological distress and T2 stressors are shown in Table 3. Risk for SPD at T3 is associated with factors from each of the three domains of stressors. Among pre-COVID demographic characteristics, the risk for SPD is higher in people age 20–39 compared to those age 60 or over (OR 2.17, 95% CI 1.0–4.8) and in those with household income below $35000 compared with those with household income above $100 000 (OR 2.64, 95% CI 1.1–6.4). Among stressors during the pandemic, SPD is higher in those who changed jobs compared to those who did not change jobs (OR 3.21, 95% CI 1.4–7.6) and in those who had medical care disrupted compared to those with a medical condition whose care was not disrupted (OR 3.32, 95% CI 1.5–7.2). No association was found between having children, with or without disruption of school or childcare, and having SPD. Finally, SPD at T1 is a strong predictor of SPD at T3; compared to those with low/no distress at T1, risk is significantly higher in those who had moderate distress (OR 4.55, 95% CI 2.0–9.7) and serious distress (OR 10.24, 95% CI 4.5–23.3).
Table 3. Association of T1 demographic characteristics, T1 psychological distress and T2 stressors with serious psychological distress at T3
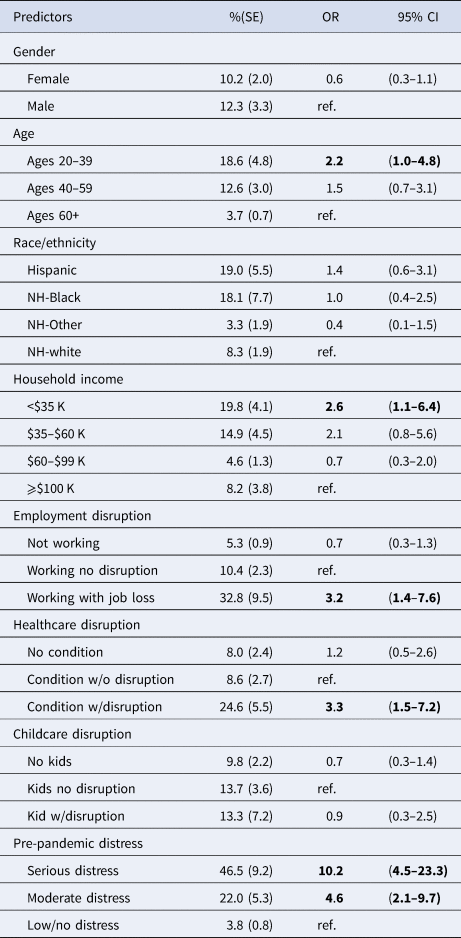
OR, odds ratio; NH, Non-Hispanic ORs estimated in binary logistic regression model.
OR >1 indicates higher odd of serious distress at T3 relative to the reference level of the predictor. Bold text indicates ORs that are significantly different from 1 at the p = 0.05 level.
In the generalized SEM model, there is an increase in SPD from T1 to T3 of 6.7% among those with no/low distress at T1. The additional (i.e. marginal) increase in the probability of SPD among those with pre-existing (T1) SPD is 6.3 percentage points (CI 4.1–8.5). In total, 37.8% of this increased probability is attributable to the indirect impact of T1 SPD on the stressors reported at T2. Among those with moderate distress at T1, the total marginal increase in the probability of SPD at T3 is 3.7 percentage points (CI 1.8–5.5). Of this effect, 32.5% is attributable to the indirect pathways from moderate SPD to reported stressors at T2.
Discussion
To inform the response to the pandemic and future prevention efforts, it is important to understand multiple factors that contribute to the risk for mental health conditions during the pandemic, including pre-pandemic psychological and social factors (Galea, Merchant, & Lurie, Reference Galea, Merchant and Lurie2020). In this study, we used data from a longitudinal cohort study of a population-based probability sample to assess prospective relationships between three domains of risk for SPD in August 2020, about 6 months after the pandemic-related disruptions of everyday life began in the USA. We find that each of these domains – pre-COVID mental health, pre-COVID socioeconomic status, and early COVID stressors – has prospective relationships with SPD during the pandemic. Specifically, SPD in August of 2020 was more common in those who had moderate or serious past-year psychological distress prior to the pandemic, low household income prior to the pandemic, and disruption in employment or health care earlier in the pandemic.
The strong relationship between pre-pandemic SPD and SPD during the pandemic is consistent with studies showing that prior mental health conditions are among the strongest predictors of post-disaster mental health status (Goldmann & Galea, Reference Goldmann and Galea2014; North, Reference North2014). Compared with those with low or no distress at T1, odds of SPD at T3 were 4.6 times higher for those with moderate distress at T1 and 10.2 times higher among those with serious distress at T1. However, our findings suggest that pre-pandemic mental health is not simply a marker of a predisposition to experience poor mental health or a continuation of prior mental health conditions. On the contrary, poor mental health prior to the pandemic is also associated with other risk factors that have prospective relationships with poor mental health during the pandemic, specifically, low household income and disruption in employment or healthcare.
To gauge the magnitude of the impact attributable to these pandemic-related stressors, we estimated a generalized SEM model to assess the apparent role of COVID stressors as mediators of the relationship between pre-COVID SPD (T1) and SPD during the pandemic (T3). Our design does not permit causal interpretation of these pathways and the magnitude of the mediating pathways might be reduced if additional variables unmeasured by our survey were included in the model. However, the findings provide some useful guidance as to the potential relative influences of pre-COVID factors v. COVID-related stressors. The SEM model shows that T1 SPD has both direct and indirect associations with T3 SPD, with about a third of the association attributable to indirect effects through disruption in employment or health care.
Low household income is likely to be an important pathway through which people with mental health conditions face increased risk for poor mental health during the pandemic. At T1, the prevalence of SPD was about twice as high among those with household income below $35 000 as among those with household income above $100 000. This underlying association between mental health status and income likely reflects the accumulation of impacts of mental illness on earnings, education, and employment over the life course (Breslau, Miller, Chung, & Schweitzer, Reference Breslau, Miller, Chung and Schweitzer2011; Kessler et al., Reference Kessler, Heeringa, Lakoma, Petukhova, Rupp, Schoenbaum and Zaslavsky2008; Luciano & Meara, Reference Luciano and Meara2014). The finding here illustrates how the social impacts of mental illness can increase the risk for subsequent experiences that exacerbate the risk for new onset or persistent course of illness (Gilman et al., Reference Gilman, Trinh, Smoller, Fava, Murphy and Breslau2013).
During the pandemic, people in the lowest quartile of income were more likely to experience SPD than people with higher incomes. Risk was also elevated, though not statistically significant, for those with incomes in the third quartile of household income relative to those in the highest quartile. The association between low income and risk for SPD likely reflects limited financial and other resources to respond effectively to the challenges posed by the pandemic. Notably, these associations are found after accounting for pre-pandemic mental health and disruption of employment during the pandemic, suggesting vulnerability that is not explained by mental health status or specific financial hardships occurring during the pandemic. Studies of prior disasters, including Hurricane Katrina (Galea et al., Reference Galea, Brewin, Gruber, Jones, King, King and Kessler2007), have also found that lower socioeconomic position is associated with poorer mental health outcomes (Norris et al., Reference Norris, Friedman, Watson, Byrne, Diaz and Kaniasty2002).
The interaction between mental health and exposure to social stressors over time is also clear in the relationship between pre-pandemic mental health, stressors early in the pandemic, and SPD later in the pandemic. Pre-pandemic psychological distress was associated with higher risk for exposure to disruption in employment and healthcare; people with SPD pre-pandemic were more likely than other people who were employed at the beginning of the pandemic to experience a job change and more likely than other people with health care needs during the pandemic to have their health care disrupted. Disruption in employment and healthcare early in the pandemic also had significant relationships with SPD later in the pandemic. In both cases, the magnitude of association is strong, with more than threefold higher odds associated with disruption relative to others at risk for disruption. Disruption in childcare was elevated in people with SPD pre-pandemic, though the association did not reach statistical significance, and not associated with SPD at T3.
Risk for disruption of employment among those with pre-pandemic psychological distress may reflect more precarious connections to jobs among people with mental health conditions and higher likelihood of employment in positions that were affected by the pandemic. Those working in high-skilled office-based jobs were less likely to lose their jobs than those working in non-essential service sector jobs. Job loss is particularly concerning given the persistent economic slowdown associated with the pandemic and the strong association of unemployment, even for short periods of time, with serious mental health consequences, including suicide attempts (Elbogen et al., Reference Elbogen, Lanier, Montgomery, Strickland, Wagner and Tsai2020; Frasquilho et al., Reference Frasquilho, Matos, Salonna, Guerreiro, Storti, Gaspar and Caldas-de-Almeida2016).
The greater likelihood of disruption of health care among those with SPD may reflect the greater burden of co-morbidity in the population with mental health conditions (Scott et al., Reference Scott, Von Korff, Alonso, Angermeyer, Bromet, Fayyad and Williams2009); higher and more complex health care needs are likely to be associated with higher likelihood of having some aspect of that care disrupted. A study of women impacted by Hurricane Katrina found that disruption of health care was among the stressors most strongly associated with persistent post-disaster mental health conditions (Raker et al., Reference Raker, Zacher and Lowe2020). Our study confirms and extends this finding by comparing people with healthcare disruption to others who also had pre-existing healthcare needs. Excluding people without immediate health care needs strengthens this comparison, but there remains a possibility that the severity of the pre-existing condition may also be related to mental health status. The associations of prior psychological distress with both employment and healthcare disruption after the onset of a disaster are particularly striking because of the indiscriminate, population-wide impact of the COVID-19 pandemic. Even in the context of a shock that adversely affects the entire population, those with prior SPD were more likely to be directly affected in ways that have adverse mental health consequences.
This study has some distinct strengths. Longitudinal studies of the psychiatric sequelae of disasters that include pre-disaster mental health assessments are rare (Parker et al., Reference Parker, Edelman, Carman and Finucane2020). Following a cohort established prior to the pandemic also minimizes common problems of implementing a robust population sampling design in the context of social disruption and dislocation that often follows disasters. This study also addresses a limitation of many studies of mental health during the pandemic in drawing on a probability-based epidemiological sample rather than convenience, ‘opt-in’ samples that have commonly been used despite the limitations in generalizability (Pierce et al., Reference Pierce, McManus, Jessop, John, Hotopf, Ford and Abel2020).
Another strength of this study is also the use of an instrument designed to identify clinically significant psychological distress. While the instrument used here, the K6, does not assess psychiatric diagnoses according to DSM criteria, it is validated against follow-up structured clinical interviews (Kessler et al., Reference Kessler, Barker, Colpe, Epstein, Gfroerer, Hiripi and Zaslavsky2003). Compared with instruments that measure the symptoms of depression, it identifies a broader range of cases, and compared to other instruments used to measure distress, it has a more direct clinical interpretation. Given that some studies have found that the prevalence of anxiety and depressive symptoms was decreasing in the general population by the summer of 2020 (Daly & Robinson, Reference Daly and Robinson2020; Riehm et al., Reference Riehm, Holingue, Smail, Kapteyn, Bennett, Thrul and Stuart2021), cases of SPD in August of 2020 are likely to reflect persistent or worsening psychiatric conditions. Notably, a study conducted in Norway that used a structured diagnostic instrument did not find increases in the prevalence of psychiatric disorders in that country over the course of the pandemic (Knudsen et al., Reference Knudsen, Stene-Larsen, Gustavson, Hotopf, Kessler, Krokstad and Reneflot2021). Whether that study's findings reflect epidemiological factors specific to Norway or to the difference between distress and clinical disorder deserves greater attention. The finding of higher prevalence of psychological distress during the pandemic has not been limited to the USA.
It is also important to note that the stressors described here do not qualify as traumatic experiences by DSM definition of posttraumatic stress disorder (PTSD). In fact, the proportion of the population exposed to traumatic events according to DSM is likely to be small (North, Suris, & Pollio, Reference North, Suris and Pollio2021). PTSD has been considered the core of post-disaster mental health response, but here we find a major population mental health response that does not involve widespread exposure to traumatic events.
The study has several limitations. First, we assessed major types of widespread stressors affecting the entire population, but we also know that certain groups, notably health care workers, experienced extremely stressful work demands and work environments during the pandemic. Moreover, we did not assess a comprehensive set of stressors, which may have included other stressors related to the pandemic, such as fear of infection, or to concurrent events, such as reactions to police brutality. Second, as noted, we were not able to assess specific psychiatric disorders, which would have enabled a sharper focus on clinically significant cases. Third, the sample is limited to English-speaking respondents; studies have yet to examine the mental health of non-English-speaking Americans during the pandemic.
This study provides evidence regarding mental health conditions 6 months following the beginning of the pandemic in the USA. Serious distress at that point in time indicates more than a transient reaction to the event, given the length of time between the beginning of the pandemic and the assessments at T3 in this study, but the longer-term trajectory of psychiatric conditions over the course of the pandemic remains an important unanswered question. Studies of prior disasters suggest that the large majority of affected individuals achieve remission over time, with a smaller portion experiencing protracted illness (Pietrzak et al., Reference Pietrzak, Tracy, Galea, Kilpatrick, Ruggiero, Hamblen and Norris2012; Pietrzak, Van Ness, Fried, Galea, & Norris, Reference Pietrzak, Van Ness, Fried, Galea and Norris2013), though prior studies focus on PTSD following exposures to specific traumatic experiences. The stressors examined here, particularly disruption of employment, were of long duration and may have longer-term mental health impacts.
As in prior studies, the clearest message from epidemiological research is that people with prior mental health history are at higher risk of poor mental health following a disaster. Policies and interventions focused on secondary prevention of exacerbation of prior illnesses are an important strategy for disaster preparedness. These strategies could make use of treatment records to reach out to current and former patients. This strategy is further supported by the finding that a large portion of those who perceived a need for mental health treatment during the pandemic had a history of mental health treatment (Breslau, North, Finucane, Roth, & Collins, Reference Breslau, North, Finucane, Roth and Collins2021b). The potential for targeting high-risk populations using cell phone apps or other Internet-based methods has been highlighted in the literature (Goldman et al., Reference Goldman, Druss, Horvitz-Lennon, Norquist, Kroeger Ptakowski, Brinkley and Jorgensen2020). Our findings also highlight the importance of addressing social determinants of health as a component of secondary prevention. In addition to the need for mental health treatment, people with prior mental health conditions may also have high needs for a wide variety of social supports (Pfefferbaum & North, Reference Pfefferbaum and North2020).
Our findings have implications beyond the current pandemic, underlining the complex ways that social stressors interact with pre-existing vulnerabilities over time. Similar evidence comes from studies showing that social stressors are associated with the persistence of mental health conditions over time (Gilman et al., Reference Gilman, Ni, Dunn, Breslau, McLaughlin, Smoller and Perlis2015, Reference Gilman, Trinh, Smoller, Fava, Murphy and Breslau2013). Psychiatric disorders, which are likely to begin in childhood or early adolescence, are markers of vulnerability to events, as indicated by the elevated risk associated with pre-disaster SPD. However, this is only one of the ways in which risk for subsequent disorder is elevated. Psychiatric disorders also have social consequences with respect to income, employment and health that increase exposure to subsequent adverse events and amplify risk.
Financial support
This work was funded by gifts from RAND supporters and income from operations. Additional support was provided by a grant from the National Institute on Minority Health and Health Disparities (PI: Breslau R01MD010274).
Conflict of interest
Dr Breslau has received funding in 2020 from Otsuka Pharmaceuticals (USA) in the form of a research grant to the RAND Corporation. The authors have no other financial disclosures.