Background
In spite of well-established benefits in terms of morbidity and mortality, preventive care remains insufficient in general practice (Anderson and May, Reference Anderson and May1995; Davis, Reference Davis1998; Wild et al., Reference Wild, Espina, Bauld, Bonanni, Brenner, Brown, Dillner, Forman, Kampman, Nilbert, Steindorf, Storm, Vineis, Baumann and Schüz2019). General practitioners (GPs), because they treat virtually everyone (Orueta et al., Reference Orueta, Lopez-De-Munain, Báez, Aiarzaguena, Aranguren and Pedrero1999), are responsible for providing preventive care (Calderón et al., Reference Calderón, Balagué, Cortada and Sánchez2011; Crabtree et al., Reference Crabtree, Miller, Tallia, Cohen, DiCicco-Bloom, McIlvain, Aita, Scott, Gregory, Stange and McDaniel2005; OMS Europe, 1998; WONCA, 2005), and it is within their reach to improve the currently poor level of prevention. However, it seems not all of them systematically include the recommendations in their practice (Holmberg et al., Reference Holmberg, Sarganas, Mittring, Braun, Dini, Heintze, Rieckmann, Muckelbauer and Müller-Nordhorn2014; Luquis and Paz, Reference Luquis and Paz2015). Several characteristics related to organization of care have been identified as potential supports for the inclusion of preventive care in general practice, but with somewhat mixed results: one component of organization of care can be positively associated with one type of preventive care and negatively associated with another. For instance, group practice is associated with less preventive care concerning alcohol use (Kaner et al., Reference Kaner, Heather, Brodie, Lock and McAvoy2001), but with more frequent cancer screening (López-de-Munain et al., Reference López-de-Munain, Torcal, López and Garay2001). GPs with a higher number of weekly consultations are more likely to provide HPV vaccination (Collange et al., Reference Collange, Fressard, Pulcini, Sebbah, Peretti-Watel and Verger2016a) and cardiovascular disease prevention (Pelletier-Fleury et al., Reference Pelletier-Fleury, Le Vaillant, Hebbrecht and Boisnault2007) but less likely to engage in alcohol use prevention (Kaner et al., Reference Kaner, Heather, Brodie, Lock and McAvoy2001). No study has examined the differential effect of specific components of health care organization on the realization of different types of preventive care. However, such a study should be instrumental for the design of prevention-focused public health policies. When one component of health care organization – say multi-professional group practice – is identified as positively associated with engagement in several or all types of preventive care, then promoting the development of group practice should be largely beneficial. On the other hand, the development of other types of organization differently associated with various types of preventive care (i.e. positively associated with some preventive care and negatively with others) should be thought through more carefully.
In this work, we consider preventive care to include several different types of care that are usually unevenly performed, that is to say that performing very well in one type of preventive care does not guarantee equal engagement in other areas of preventive care. Indeed, GPs may have different levels of knowledge, competences, and beliefs concerning different areas of prevention, and competence in one aspect of prevention is not necessarily transferrable to another. This is why we chose here to focus on two very different types of preventive care: immunization and addiction prevention. While immunization is fast, requires limited engagement from GPs, and benefits from a widely accepted biomedical footing, addiction-related prevention is more time-consuming and requires meaningful exchanges with patients concerning their lifestyles and mental well-being, and an overall psychosocial engagement in preventive care.
We chose to focus on four types of preventive care. Concerning immunization, we focused on flu and HPV vaccination. While flu vaccination has been in use for many years (INVS, n.d.) and is very well established in GP practices (Collange et al., Reference Collange, Verger, Launay and Pulcini2016b), HPV vaccination is more recent (Koulova et al., Reference Koulova, Tsui, Irwin, Van Damme, Biellik and Aguado2008), subject to more discussion (Collange et al., Reference Collange, Fressard, Pulcini, Sebbah, Peretti-Watel and Verger2016a), and less solidly established in GP practices (Wild et al., Reference Wild, Espina, Bauld, Bonanni, Brenner, Brown, Dillner, Forman, Kampman, Nilbert, Steindorf, Storm, Vineis, Baumann and Schüz2019). Regarding addiction prevention, we focused on alcohol (Madureira-Lima and Galea, Reference Madureira-Lima and Galea2018) and tobacco use (Marie et al., Reference Marie, Freeman, Fleming, Robinson, Dwyer-Lindgren, Thomson, Wollum, Sanman, Wulf, Lopez, Murray and Gakidou2014), the two most frequent addictive behaviors.
In France, as in other countries, GPs are responsible for prevention and the promotion of healthy behaviors to a great extent (J.O., 2004 ; WONCA, 2005). Aside from specialist who provide prevention services on occasion, no dedicated medical staff are responsible for prevention work.
Almost half of practicing physicians are GPs in private practices (CNOM and Bouet, Reference Bouet2018). They work on a fee-for-service basis, in solo or group practice. Group practice (generally from two to five GPs) concerns half of French GPs today (DREES, 2019). With the lowest fee directly supported by patients in Europe, and good geographical access (98% of the French population live within 10 min of a GP), general access to GPs is high (DREES, 2015). In France, GPs lack meaningful financial incentives to systematically perform prevention services (Samson, Reference Samson2009). Most GPs are paid on a fee-for-service basis, with an identical fee whatever the service (only 6 % of GPs are able to establish their own fees) (Bras, Reference Bras2015). Capitation constitutes only 15% of GPs’ income (with prevention work contributing to only one-third of capitation fees) (DREES, 2020). By contrast, in the Netherlands, GPs are paid through capitation that includes prevention services (Pellet, Reference Pellet2016).
We investigate here the association between health care organization in general practice and engagement in these two different areas of preventive care in France.
Methods
Data
We used the data of the 2009 GP Health Barometer which targets GPs in private practices in France. This survey is a nationally representative telephone study conducted by the French National Institute for Health Prevention and Education (INPES). These surveys collect GPs’ characteristics and self-reported prevention practices. The 2009 issue included 1,935 respondents (participation rate of 57.1%).
Variables of interest
We used four variables informing on different preventive care practices. Two of them concerned immunization: flu and HPV vaccination. The other two variables concerned prevention of addictive behaviors: tobacco and alcohol use prevention. For immunization, respondents were asked how often they offered flu vaccination to patients aged above 65 years and how often they offered HPV vaccination to teenage girl patients: systematically, often, sometimes, and never (Santé publique France, 2019). Less than 2% of respondents answered ‘sometimes’ or ‘never’; therefore, the variables were recoded into ‘systematically’ (coded as 1) versus all other answers (coded as 0). Concerning tobacco and alcohol use prevention, respondents were asked how often they provided prevention counseling: at least once with each patient, only with at-risk patient, only when patients bring up the issue, and never (SFA, 2015). On average, only 1.9% of respondents answered ‘only when patients bring up the issue’ or ‘never’. Therefore, the variables were recoded into ‘at least once with each patient’ (coded as 1) versus all other answers (coded as 0).
GPs’ characteristics
We considered health care organization characteristics reported by each GP : fee regulation (either regulated or unregulated : fees and coverage rates are fixed in accordance with National Health Insurance, while GP working with unregulated fees decide higher fees, the difference is supported by patient or complementary insurance), digitalization of medical files, practice of alternative medicine such as homeopathy or acupuncture (regular, occasional, or none), solo or group practice, number of daily consultations (< 15, 15 to 30, and > 30). We also used GPs’ demographic characteristics: sex and age (< 45, 45 to 65, and > 65 years old).
We used two characteristics related to the context of the area of practice, with potential impact on preventive care practice and health care organization. The first one is a measure of spatial accessibility to GPs computed by the French National Organization for Research, Evaluation and Statistics (DREES) (Barlet et al., Reference Barlet, Coldefy, Collin and Lucas-Gabrielli2012). This indicator is computed for each French city and provides a measure of GP accessibility (number of GPs for 100 000 inhabitants) with a national average of 71. We classified counties into two groups according to spatial accessibility: above or below the national average. The second context-related characteristic is the socioeconomic level of the area of practice, estimated with the average annual income level per consumption unit for each county. It allows us to consider the income of households of different sizes or compositions, attributing different weights to household members (adult aged 18 years and over = 1.0; child aged below 14 years = 0.3) (Accardo, Reference Accardo2007; Insee, 2021). Counties were also classified into two groups, above or below the national average (19 270 euros/consumption unit).
The association between our variables of interest and the two characteristics related to the context of the area of practice being nonlinear, we built several models using different categorizations of the indicators: as binary variables (above/below the national average) and as variables with five categories (based on the quintile distribution). In view of parsimony, we selected the binary categorization of indicators, allowing to compute models with lower AIC (Akaïke information criterion) values (Hurvich and Tsai, Reference Hurvich and Tsai1995). Observations with missing values for our context-related characteristics (n = 122) were excluded. Analyses were conducted on 1813 respondents.
Statistical analyses
To take into account the hierarchical structure of our data (i.e. the fact that several GPs worked in the same county), mixed logistic regression models with random intercept were used (Snijder and Bosker, Reference Snijder and Bosker1999). We first described the characteristics of respondents. To assess the comparability of respondents with regard to their area of practice, we compared the distribution of their demographic and organization characteristics according to the area spatial accessibility and income level. We conducted univariate analyses testing for associations between each of the four organization characteristics (independents variables) and each of the four preventive care (dependants variables). We then conducted a multivariate logistic regression analysis controlling for GPs’ demographic characteristics and the two characteristics related to the context of the area of practice.
In order to test whether the associations between the organization variables and each of the preventive care types were similar, we computed a new database. While our initial database included one line for each respondent and four columns for the four considered preventive care types, our new dataset contained four lines for each respondent, each line corresponding to one preventive care type (as binary dependent variables). An indicator variable ranging from 1 to 4 was computed to indicate to what preventive care type each line corresponded. A random term allowed us to take into account in the analyses the fact that the four preventive care types referred to one respondent. We were then able to analyze the interaction between each organizational variable and the indicative variable. A significant interaction term meant that the associations between the organization variable and the various preventive care services differed. A nonsignificant interaction term indicated that the organization characteristic was associated with preventive care in the same way for all preventive services. In this case (no interaction), (1) we called this newly dependant variable ‘overall provision of preventive care’ as it corresponded to the proportion of preventive care carried out by GPs and (2) we ran the analyses on this new variable.
We considered tests to be significant with P-value < 0,05. No correction for multiple testing was performed, but P-values were presented because they give a measure of the degree of data compatibility with the null hypothesis.
Results
Two-third of the respondents were men GPs, most of them aged 45 to 65 years, practicing in cities with a mean GP spatial accessibility of 80.1 GPs per 100 000 inhabitants (standard deviation = 25.5) and a mean household income per consumption unit of 18 871 euros (standard deviation = 3,800) (Table 1). GPs working in an area with low GP spatial accessibility often did not practice alternative medicine and did not work in a group practice. GPs working in areas with low-income levels were more often older men, had more daily consultations, and worked more often with regulated fees. Reported provision of preventive care to patients varied from 87% for flu vaccination, 57.2% for HPV vaccination, to 68% for tobacco smoking, to 25% for alcohol use (Table 2).
Table 1. GPs’ characteristics according to geographical accessibility and income level of their area of practice (N = 1935) Values in bold correspond to a significant test with a P-value < 0.05

Table 2. GPs’ organizational characteristics and preventive care services (univariate analysis) (N = 1813) Values in bold correspond to a significant test with a P-value < 0.05
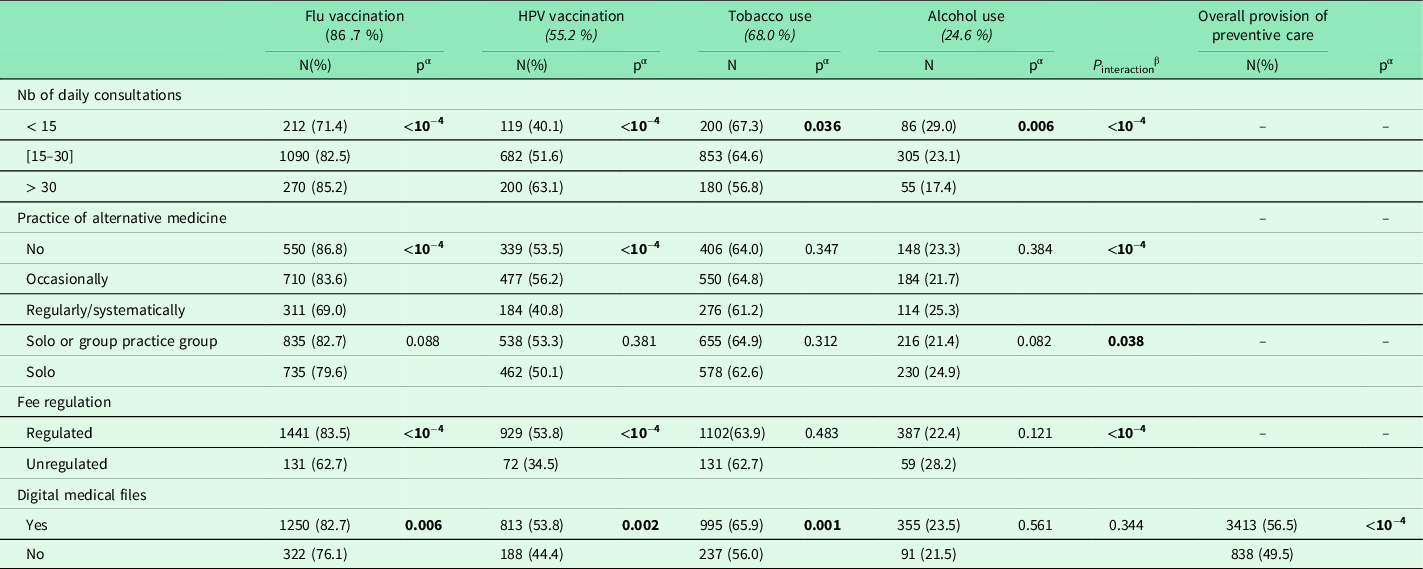
pα = P-value for univariate mixed-models logistic regression testing the association between preventive care variables/overall provision of preventive care (dependent variable) and organization variables (independent variables).
β A significant test indicates that the associations between the organization variable and the four preventive care are not similar.
We found that four out of five health care organization characteristics were differently associated with preventive care realization depending on the type of preventive care considered, with statistically significant interaction terms. Number of daily consultations were positively associated with vaccination and negatively with tobacco and alcohol use prevention, with GPs seeing the most patients daily offering vaccination more often but providing tobacco or alcohol use prevention counseling less often. Practicing alternative medicine was negatively associated with vaccination and positively associated with tobacco and alcohol use prevention. Working with unregulated fees was associated with offering vaccination more often but was not associated with providing tobacco or alcohol use prevention counseling. Working in solo or group practice was not associated with the four preventive care types. On the contrary, having digital medical files was positively associated with all four preventive care variables.
In multivariate analyses, similar results were found, except for working with digital medical files, not associated here with offering flu vaccination (Table 3). It was associated with the overall provision of preventive care.
Table 3. GPs’ organizational characteristics and preventive care services (multivariate analysis) (N = 1813)

*Odd ratios for multivariate mixed-models logistic regression testing the association between preventive care variables/overall provision of preventive care (dependent variable) and organization variables (independent variables) controlling for GPs’ demographic characteristics (age, sex, and area of practice) and contextual variables (practice income level and spatial accessibility).
β A significant test indicates that the associations between the organization variable and the four preventive care are not similar.
Discussion
Our results confirm our hypothesis that different organization characteristics have uneven impacts on different types of preventive care. Some characteristics, such as number of daily consultations, are associated with better immunization prevention but with poorer prevention counseling in addictive behaviors. Some characteristics are associated with only one type of preventive care, as working with regulated fees is associated only with immunization. Other characteristics, such as working with digital medical files, are uniformly associated with both types of preventive care.
Previous studies that have investigated the association between GPs’ organization characteristics and providing preventive care support our findings of an association between organization characteristics and preventive practices. A large number of daily consultations has been shown to be associated with offering HPV vaccination (Collange et al., Reference Collange, Fressard, Pulcini, Sebbah, Peretti-Watel and Verger2016a) but not with offering flu vaccination (Pelletier-Fleury et al., Reference Pelletier-Fleury, Le Vaillant, Hebbrecht and Boisnault2007) and to be inversely associated with tobacco prevention in Spain and alcohol use prevention in England (Kaner et al., Reference Kaner, Heather, Brodie, Lock and McAvoy2001). The practice of alternative medicine was associated with less HPV vaccination in a quantitative study (Collange et al., Reference Collange, Fressard, Pulcini, Sebbah, Peretti-Watel and Verger2016a). Our findings also resonate with previous qualitatives studies that found that GPs practicing alternative medicine were more likely to have a negative perception of vaccination (Pulcini et al., Reference Pulcini, Massin, Launay and Verger2013; Verger et al., Reference Verger, Fressard, Collange, Gautier, Jestin, Launay, Raude, Pulcini and Peretti-Watel2015). However, these previous studies did not compare the strength of associations between each organizational characteristic and the different types of preventive care, and we were able to do it using interaction tests. This allowed us to show that having digital medical files is the only organization characteristic consistently associated with all preventive practices. This could be due to the use of digital reminders (Mitchell and Sullivan, Reference Mitchell and Sullivan2001).
In France, GPs are free to organize their own practice as they see fit. We have demonstrated that these organization choices are associated with the frequency and the nature of the preventive care provided. Our findings suggest that the selection of preventive care provided is understood in terms of areas of prevention: immunization versus addictive behaviors counseling. Indeed, in our findings, within the immunization area of prevention, both vaccinations are associated with similar organization characteristics, and the same is true for the prevention of addictive behaviors. For example, working with regulated fees is associated with more systematic offering of both vaccinations, while it is not associated with prevention of both tobacco and alcohol use. We hypothesize that this is due to the fact that different types of preventive care within an area of prevention have common characteristics. For instance, they require different consultation duration : (Bucher et al., Reference Bucher, Maury, Rosso, de Chanaud, Bloy, Pendola-Luchel, Delpech, Paquet, Falcoff, Ringa and Rigal2017) vaccinations are rapidly carried out, while addressing dependence to tobacco or alcohol is considered time-consuming (Helgason and Lund, Reference Helgason and Lund2002; Vogt et al., Reference Vogt, Hall and Marteau2005). They also require different medical skills (Chartier et al., n.d.; Miller, Reference Miller1990). Vaccination is a technical act, while addressing additions can involve a wider discussion on patients’ lifestyles, emotional needs, and coping mechanisms. This hypothesis of different medical skills has been raised by GPs concerning the practice of alternative medicine. GPs who do not practice alternative medicine have reported little investment in addiction prevention in their practice, considering themselves not to be competent on this topic (van Haselen et al., Reference van Haselen, Reiber, Nickel, Jakob and Fisher2004; Vogt et al., Reference Vogt, Hall and Marteau2005). This, in turns, has lead GPs practicing alternative medicine to address this area, especially as an area under-addressed by their colleagues (van Haselen et al., Reference van Haselen, Reiber, Nickel, Jakob and Fisher2004).
Several existing studies have demonstrated that GPs are convinced that they play an important role in prevention in general (Rafferty, Reference Rafferty1998; McAvoy et al., Reference McAvoy, Kaner, Lock, Heather and Gilvarry1999; Yarnall et al., Reference Yarnall, Pollak, Østbye, Krause and Michener2003; Gelly et al., Reference Gelly, Le Bel, Aubin-Auger, Mercier, Youssef, Mentre, Nougairede, Letrilliart and Duval2014; Bucher et al., Reference Bucher, Maury, Rosso, de Chanaud, Bloy, Pendola-Luchel, Delpech, Paquet, Falcoff, Ringa and Rigal2017). Then why do we observe such selectivity among different types of preventive care? We suggest that time constraints play a role here. Indeed, providing prevention care is time-consuming (Bucher et al., Reference Bucher, Maury, Rosso, de Chanaud, Bloy, Pendola-Luchel, Delpech, Paquet, Falcoff, Ringa and Rigal2017) and this could be the main reason why GPs choose to provide one type of preventive care over others. In turn, this choice is determined by characteristics related to the organization of their practice. It appears that GPs who receive a large number of patients in a day favor immunization, while GPs with a lighter workload invest in more time-consuming addiction-related preventive care.
Strengths and limitations
One limitation of our work is that no data about respondents’ patients are available. However, patients’ characteristics influence preventive care practices. Concerning an alcohol use-related score, it has been shown that the higher the score, the likelier it is that the topic of alcohol use will be raised (Cheeta et al., Reference Cheeta, Drummond, Oyefeso, Phillips, Deluca, Perryman and Coulton2008; Mansfield et al., Reference Mansfield, Crellin, Denholm, Quint, Smeeth, Cook and Herrett2019). Also, flu vaccination is more likely to take place among patients who have frequent GP visits (Pelletier-Fleury et al., Reference Pelletier-Fleury, Le Vaillant, Hebbrecht and Boisnault2007). Secondly, because our study took place in France where the 98.5% of general medicine consultations take place in private practice (SNDS, 2020), our results cannot be generalized to contexts where GPs work in public facilities such as, for instance, the UK (Pellet, Reference Pellet2016) or certain regions of Spain (Diurni, Reference Diurni2016). An additional limitation is that our data were collected in 2009. We chose to analyze the Health Barometer from 2009 in order to take into account the socioeconomic context and GP local availability in our analyses. These characteristics, known to influence GPs’ preventive practices (Shi et al., Reference Shi, Macinko, Starfield, Wulu, Regan and Politzer2003; Starfield et al., Reference Starfield, Shi and Macinko2005; Maj et al., Reference Maj, Poncet, Panjo, Gautier, Chauvin, Menvielle, Cadot, Ringa and Rigal2019), were available only for the Health Barometer 2009, and not in the subsequent Health Barometer data collections. Although it is possible that the association between organization characteristics and prevention practices have changed since 2009, several elements points to the contrary. First, the national guidelines concerning flu vaccination and prevention have not changed: at-risk patients should receive flu vaccination once a year (INPES) and addictive behaviors should be discussed as often as possible (HAS). Moreover, the engagement of GPs in prevention has remained limited (Sebo et al., Reference Sebo, Cerutti, Fournier, Rat, Rougerie, Senn, Haller and Maisonneuve2017); public policies for prevention promotion have remained ineffective (OECD, 2019). There has been no modification to the organization of preventive care delivery. However, public perception of prevention may have changed, since tobacco and alcohol consumption have decreased: 4.5 percentage points for tobacco and 0.5 g/week for alcohol between 2014 and 2019 (Palle, Reference Palle2019; Pasquereau and Andler, Reference Pasquereau and Andler2020). However, vaccination coverage have seen no increase (Richard and Beck, Reference Richard and Beck2016; SPF, 2019; INVS, 2020). In addition, we analyze self-reported prevention practices. It is likely that GPs overestimate their prevention work. It has been shown to be the case when practitioners are asked to self-evaluate their medical skills (Davis et al., Reference Davis, Mazmanian, Fordis, Van Harrison, Thorpe and Perrier2006; Sargeant, Reference Sargeant2008). However, there are no reason to believe that the association between self-reported prevention practices and organization characteristics would be much different from the association between actually carried out prevention practices and organization characteristics. Moreover, we chose to categorize reported practices in binary variables and to separate systematic practice from occasional practice, ranging from ‘sometimes’ to ‘often’ and leaving space for a measurement bias. Lastly, because this is a cross-sectional study, we were not able to demonstrate causality between dependent and organizational variables, but only statistical associations.
Our main strength is that we have been able to include in our multivariate analyses characteristics that are known to be associated with prevention practices such as income level and spatial accessibility to GPs in the area of practice (Starfield et al., Reference Starfield, Shi and Macinko2005). Moreover, we used a mixed-model approach to take into account the geographic variability of GPs.
Research in practice
These results are relevant for implementing meaningful health promotion prevention. First, our analyses are GP-centered: an approach that improves prevention practice at their level would be beneficial for all patients. Second, our findings provide tools for political action that will positively impact GPs prevention practices, regardless of the variability of income level and spatial accessibility across the country.
Our findings add to existing research insofar as looking at different types of preventive care separately will allow to better understand the specific processes at play and the effect of the geographical context on prevention practices.
Our results should be taken into account by public health policies. Promoting one type of organization of care can be beneficial for one aspect of prevention but less so for others. Our results show that promoting organization characteristics that have a consistently positive impact on prevention care, such as using digital medical files, could be an effective way to improve preventive practices generally.
Future research should explore this question in different settings with a different organization of health care (for instance in settings where GPs work in public facilities). GPs should be made aware of these results, as it appears that even while systematically performing specific prevention services, other types of prevention services might be overlooked. Lastly, and for the French context specifically, where only cervical cancer screening incurs specific additional payment, specific compensation could be established for time-consuming prevention services, since lack of time during consultation is likely to be a key reason for performing only types of preventive care.
Conclusion
Prevention is not a set of identical preventive care services, but a group of activities each carrying its own logic and time frame. Too often, prevention is understood or presented as a homogenous package to be delivered by GPs. An approach centered on specific types of preventive care should help deepen our understanding of prevention and possibly to identify a new typology for preventive care, specifying technical, behavioral, or other types of preventive care. It appears eventually that no organizational characteristic is associated with less or no prevention, but rather that some organization characteristics are more favorable for some types of preventive care than for others.
Acknowledgments
The authors would like to thank all members of the French National Institute for Health Prevention and Education (INPES) members and all the participants who took part in the 2009 GP Health Barometer from where data for this current study were used.
Declaration
Ethics approval and consent to participate
The 2009 GP Health Barometer study, from which the data were derived for this current study, obtained all the necessary ethical regularly permissions. It was approved by the National Data Protection Authority (Commission nationale de l’informatique et des libertées), which is responsible for the ethical issues and protection of individuals from illegal or inappropriate electronic data collection. This ethical approval was for the 2009 GP Health Barometer study and subsequent research using the same data. As this current study carried out secondary data analysis of the 2009 GP Health Barometer, it did not require direct ethical approval.
Consent for publication
Not applicable
Avaibility of data and material
GP Health Barometer survey is available from the Santé Publique France (https://www.santepubliquefrance.fr/) upon reasonable request.
Competing interests
The authors declare that they have no competing interests
Funding
This project was funded by the French Research Institute in Public Health (IReSP). The funder had no role in the creation of the research question, design of the study, data collection, analysis, interpretation, or in the writing of this manuscript.








