Introduction
Often referred to as psychotic-like experiences, hallucinations and delusions that occur in the absence of a psychotic disorder are not uncommon in the general population (Van Os et al. Reference Van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009, Kelleher et al. Reference Kelleher, Connor, Clarke, Devlin, Harley and Cannon2012a). Although many individuals who experience hallucinations or delusions do so in the absence of any mental disorder (Peters et al. Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016), higher rates of both concurrent and later mental disorder have been found in young people who report these phenomena (Kelleher et al. Reference Kelleher, Keeley, Corcoran, Lynch, Fitzpatrick, Devlin, Molloy, Roddy, Clarke, Harley, Arseneault, Wasserman, Carli, Sarchiapone, Hoven, Wasserman and Cannon2012b, DeVylder et al. Reference DeVylder, Burnette and Yang2014, Kelleher et al. Reference Kelleher, Wigman, Harley, O’Hanlon, Coughlan, Rawdon, Murphy, Power, Higgins and Cannon2015, Waters et al. Reference Waters, Blom, Jardri, Hugdahl and Sommer2017, Healy et al. Reference Healy, Gordon, Coughlan, Clarke, Kelleher and Cannon2018b, Hielscher et al. Reference Hielscher, Connell, Lawrence, Zubrick, Hafekost and Scott2018, Carey et al. Reference Carey, Gillan, Healy, Dooley, Campbell, McGrane, O’Neill, Coughlan, Clarke, Kelleher and Cannon2020). For this reason, young people with a history of hallucinations and delusions represent a unique and important group for ongoing research into the relationship between these phenomena and psychopathology. Phenomenological studies can play a key role in this effort (Humpston Reference Humpston2014, Bentall Reference Bentall2015, Upthegrove et al. Reference Upthegrove, Ives, Broome, Caldwell, Wood and Oyebode2016, Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020). They have the potential to provide new insights into the nature of these phenomena and if and how they are related to psychopathology. This is reflected in a recent increase in phenomenological studies exploring these phenomena in individuals with both psychotic (Woods et al. Reference Woods, Jones, Alderson-Day, Callard and Fernyhough2015, Upthegrove et al. Reference Upthegrove, Ives, Broome, Caldwell, Wood and Oyebode2016) and non-psychotic disorders (Johns et al. Reference Johns, Kompus, Connell, Humpston, Lincoln, Longden, Preti, Alderson-Day, Badcock, Cella, Fernyhough, McCarthy-Jones, Peters, Raballo, Scott, Siddi, Sommer and Larøi2014, Wallis et al. Reference Wallis, Denno, Ives, Mallikarjun, Wood, Oyebode, Broome and Upthegrove2020).
With some exceptions, most phenomenological studies to date have examined singular hallucinatory phenomena, voice-hearing in particular (e.g. Beavan Reference Beavan2011, McCarthy-Jones et al. Reference McCarthy-Jones, Krueger, Larøi, Broome and Fernyhough2013, Wallis et al. Reference Wallis, Denno, Ives, Mallikarjun, Wood, Oyebode, Broome and Upthegrove2020). However, evidence suggests that individuals’ experiences extend well beyond voice-hearing (Peters et al. Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016, Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020, Sullivan et al. Reference Sullivan, Kounali, Cannon, David, Fletcher, Holmans, Jones, Jones, Linden and Lewis2020). In their study of over 3,800 individuals, the Avon Longitudinal Study of Parents and Children (ALSPAC) found that 85% had experienced hallucinatory phenomena, 29% delusion-like beliefs and 15% had experienced both between the ages of 12 and 24 years (Sullivan et al. Reference Sullivan, Kounali, Cannon, David, Fletcher, Holmans, Jones, Jones, Linden and Lewis2020). Recently, we also found evidence of multi-modal hallucinations and delusions in young people aged 11–13 years. In those who reported these phenomena, 98% reported hallucinations, 40% reported delusional or delusion-like beliefs and 38% reported both (Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020). Two further longitudinal studies we conducted also found that not all young people who reported early experiences of hallucinations and delusions were at high risk for poor outcomes in early adulthood (Coughlan et al. Reference Coughlan, Healy, Ní Sheaghdha, Murray, Humphries, Clarke and Cannon2019, Coughlan et al. Reference Coughlan, Walton-Ball, Carey, Healy, O’Regan-Murphy, Uidhir, Clarke and Cannon2021). These findings raise questions about if and how phenomenological differences in early hallucinatory and delusional experience may be related to differing outcomes in later life.
Using longitudinal phenomenological data from the Adolescent Brain Development (ABD) study, the aim of the current study was to examine phenomenological trajectories and characteristics of hallucinatory and delusional phenomena in young people between early adolescence and early adulthood. The study adopted a phenomenological approach, giving primacy to individuals’ subjective interpretations of their lived experiences and searching for shared meanings across multiple individual experiences (Kvale Reference Kvale1996, Creswell Reference Creswell2012).
Material and methods
Study participants
Participants were 17 young people from the ABD study. The ABD study is a longitudinal study that has been examining psychopathology, brain development and neurocognitive functioning among Irish youth since 2007. Full details about the ABD study have been described in detail elsewhere (Kelleher et al. Reference Kelleher, Murtagh, Molloy, Roddy, Clarke, Harley and Cannon2012c, Coughlan et al. Reference Coughlan, Tiedt, Clarke, Kelleher, Tabish, Molloy, Harley and Cannon2014). Briefly, participants were recruited from a representative sample of 16 primary schools in North Dublin and environs. At baseline, 1,131 young people aged 11–13 years were screened using the Strengths and Difficulties Questionnaire (SDQ) (Goodman et al. Reference Goodman, Ford, Simmons, Gatward and Meltzer2003) and the Adolescent Psychotic Symptoms Screener (APSS) (Kelleher et al. Reference Kelleher, Harley, Murtagh and Cannon2011). A representative sample of 211 of those who were screened attended for clinical interview and neurocognitive testing. Of those, 100 also attended for magnetic brain resonance imaging, 86 of whom attended for follow-up when they were aged 14–18 years. A nested qualitative study was later conducted with a subsample of 17 of these individuals when they were aged 18–21 years. For the nested study, all individuals aged 18 years or older with a history of hallucinations and/or delusions who had attended at both baseline and follow-up (N = 18) were invited to take part. Of those, 17 opted into the nested study (see Fig. 1). One individual did not respond to two letters of invitation to take part. No further contact was made with that individual thereafter. Longitudinal data from these 17 individuals were analysed for the current study.

Fig. 1. Longitudinal study design and sample size at each time point
Assessment of hallucinations, delusions and psychopathology
Assessment of psychopathology
At baseline and mid-adolescence follow-up, psychopathology was assessed using the Schedule for Affective Disorders and Schizophrenia (K-SADS-PL) (Kaufman et al. Reference Kaufman, Birmaher, Brent, Rao, Flynn, Moreci, Williamson and Ryan1997). The K-SADS-PL is a validated clinical interview assessment tool, used to determine lifetime and current (past month) rates of mental disorders in children and adolescents using Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria (American Psychiatric Association 1994). Psychopathology was not clinically assessed as part of the nested qualitative study. However, all participants were asked if they had been diagnosed with any mental disorder and/or had attended mental health services. For the current study, any participant report of a mental disorder diagnosis given by a health or mental health professional was coded as a lifetime experience of mental disorder.
Assessment of hallucinations and delusions
As part of the clinical interview protocol at baseline and mid-adolescence follow-up, a detailed assessment was completed to determine lifetime rates of hallucinations and/or delusions. Interviewers recorded responses to questions on hallucinatory and/or delusional experiences using contemporaneous, hand-written notes taken during participants’ clinical interviews. These were stored as string data. All data on reported hallucinatory and delusion-like experiences were first rated independently by three members of the ABD study team, all of whom had qualifications and experience in psychiatry, psychology or an allied health profession. After this, a consensus meeting was held to finalise ratings and determine rates of hallucinations and/or delusions within the sample. Detailed information on this assessment and rating process have been extensively described previously (Kelleher et al. Reference Kelleher, Murtagh, Molloy, Roddy, Clarke, Harley and Cannon2012c, Healy et al. Reference Healy, Campbell, Coughlan, Clarke, Kelleher and Cannon2018a, Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020).
During the nested qualitative study, all participants were asked the following:
Thinking back over your whole life, have you ever had any experiences that you would describe as unusual, like seeing things other people didn’t see or hearing voices or sounds that other people didn’t hear? Have you ever had other kinds of experiences like this? Have you ever experienced anything like thinking you had special powers, could read people’s minds, or that aliens or other spirits were controlling you or sending you messages?
Any participant who answered yes to any of these questions was asked a series of follow-up questions about the details, attributions and meaning of their experiences. Qualitative interviews, lasting between 45 and 110 minutes, were conducted by the lead author (HC) from May to July 2016 at the Royal College of Surgeons in Ireland (RCSI). Audio recordings were transcribed by an external transcription agency and were subject to a non-disclosure agreement.
Phenomenology coding
This study was grounded in phenomenology, an approach that can be conceptualised in multiple ways depending on the philosophical, ontological and epistemological position held (Davidsen Reference Davidsen2013). In this study, descriptive phenomenology was used, an approach that gives primacy to the description and subjective perceptions of the individual (Kvale Reference Kvale1996). In the field of psychopathology, it is used when the aim is to describe and categorise experiences without seeking to interpret the origins or causes of the phenomena described (Oyebode Reference Oyebode2015).
For the current study, data on hallucinations, delusions and psychopathology were extracted from data files at all three time points. At both baseline and mid-adolescence follow-up, data on hallucinations and delusions were in the form of hand-written interviewer notes, recorded as string data. At early adulthood, they were in the form of verbatim qualitative interview data. Content analysis was used to examine the data. This method has particular application in the analysis of multiple forms of recorded communication (Mayring Reference Mayring2004). It can be used to conduct both categorical and thematic coding, which enables researchers to both quantify and describe phenomenological experiences (Krippendorff Reference Krippendorff2004, Hsieh & Shannon-Reference Hsieh and Shannon2005, Assarroudi et al. Reference Assarroudi, Heshmati Nabavi, Armat, Ebadi and Vaismoradi2018). It was therefore ideally suited to the combination of interviewer notes and qualitative data that were used for this study.
To track phenomenological trends, use was made of a coding frame we had previously developed to analyse data on hallucinations and delusions in a cross-sectional phenomenological study of the ABD baseline study sample (see Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020). It was organised under four phenomenological domains: (1) auditory verbal phenomena; (2) auditory non-verbal phenomena; (3) non-auditory perceptual phenomena; and (4) unusual thoughts and beliefs. For this study, neither illusions nor voice-hearing that only involved hearing one’s name called aloud were included in the analysis.
At each time point, phenomenological data were also ascribed a temporal code. At early adolescence, hallucinations and/or delusions were coded as occurring at any time up to and including the baseline interview (lifetime). At both other time points, phenomena were coded as occurring either in the interim (occurring between the previous and current interviews but not within the past 12 months), recently (within the past 12 months) or retrospectively (a childhood or adolescent experience that had not been reported prospectively at an earlier phase of the study). Once coding was complete, codes were used to track phenomenological characteristics of hallucinations and delusions over time using a quantitative count of categories and domains.
Phenomenological aspects of young people’s experiences of hallucinations and delusions over time were also examined using inductive thematic analysis (Braun & Clarke Reference Braun and Clarke2006). Qualitative differences among young people who reported reoccurring hallucinations and/or delusions from early adolescence to early adulthood were explored and compared. To protect their identity, each individual was assigned a pseudonym. These pseudonyms are used to report findings. Illustrative qualitative findings are presented using either verbatim extracts of interviewer notes (early and mid-adolescence) or qualitative interview data (early adulthood). To protect the anonymity of some participants, a small number of quotes use a generic descriptor in place of detailed data (placed in square brackets in the quote). All analyses were conducted by the first author (HC). Microsoft Excel was used for coding and organising the data.
Results
Sample characteristics
The sample was made up of 10 males and 7 females, most of whom had met lifetime criteria for either an Axis I (N = 14) and/or Axis II (N = 2) DSM-IV disorder (see Table 1). One individual had briefly been diagnosed with a psychotic disorder in early adulthood. This was a transient diagnosis.
Table 1. Sample characteristics at the age of 18–21 years
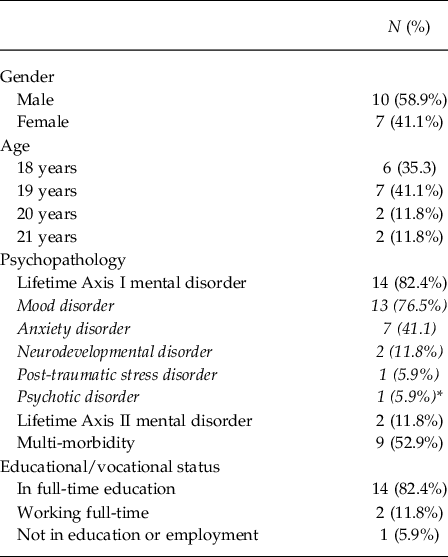
* During qualitative interviews, one individual reported being briefly diagnosed with a psychotic disorder while attending adult mental health services. However, the individual indicated that this diagnosis was subsequently changed to another diagnosis. To protect this individual’s anonymity, we have not indicated specific details regarding the changed diagnosis in this paper.
Trajectories and phenomenological characteristics of hallucinations and delusions between early adolescence and early adulthood
Among the sample, experiences of hallucinations and delusions decreased between early adolescence and early adulthood (see Fig. 2). Eight individuals only reported hallucinations and/or delusions in early adolescence, two in both early and mid-adolescence and six at all three time points. The remaining one individual retrospectively reported a childhood experience in mid-adolescence. Although decreasing rates were observed across all domains, the most notable reduction was in auditory verbal phenomena between early and mid-late adolescence. No individual reported hearing voices after mid-adolescence. Table 2 summarises participant reports regarding the phenomenology and attributions of hallucinations and delusions experienced between early adolescence and early adulthood.
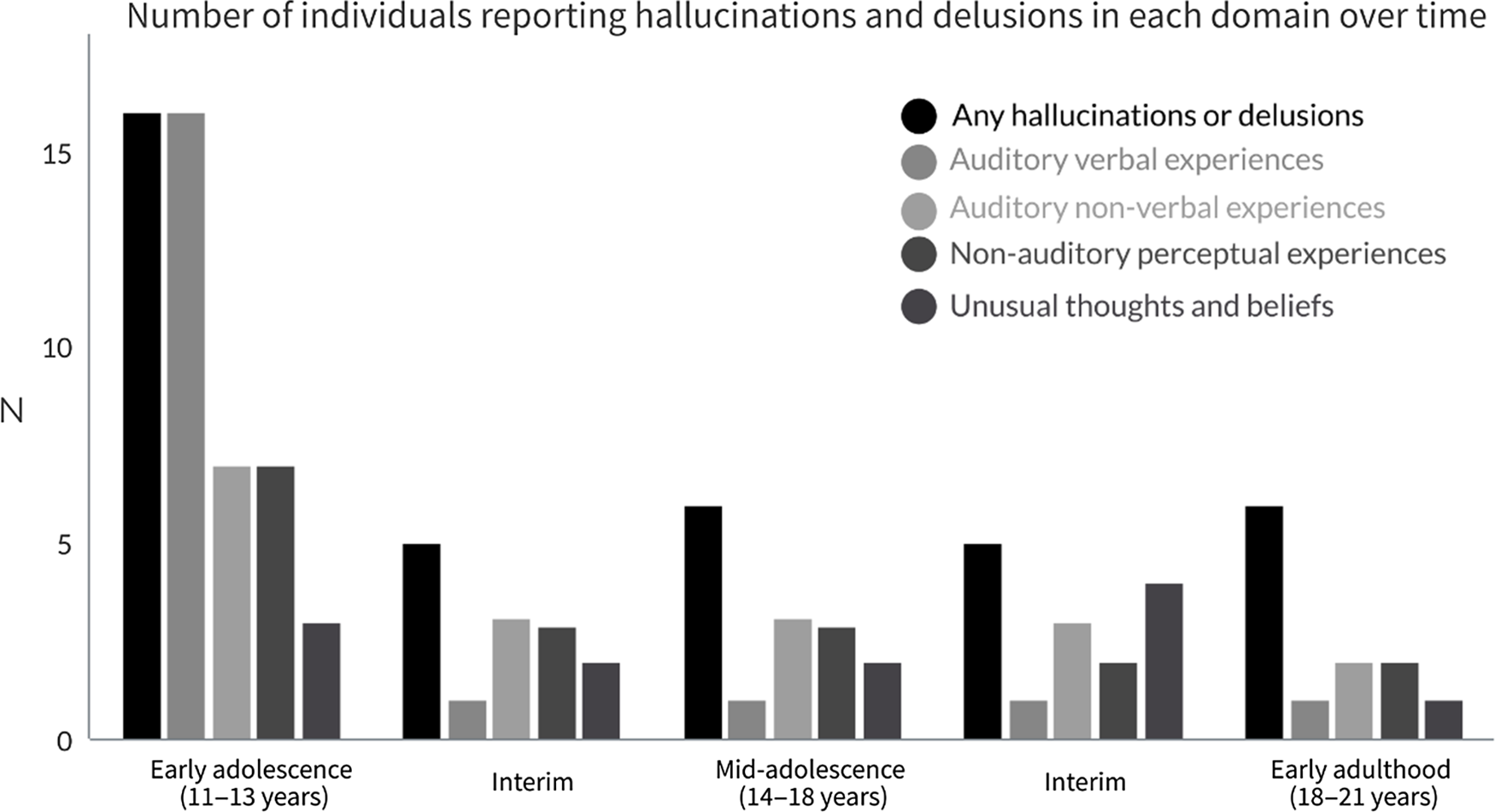
Fig. 2. Number of individuals who reported hallucinations and delusions in each domain between early adolescence and early adulthood
Table 2. Longitudinal summary of reported hallucinations, delusions and related attributions from early adolescence to early adulthood

a To protect the anonymity of participants, all names are pseudonyms.
b These include hallucinatory and delusional experiences that occurred between time points (e.g. mid-adolescence includes any hallucinatory and delusional experiences reported after individuals’ early adolescent interviews, up to including the time of their mid-adolescence interview).
c These refer to hallucinatory and delusional experiences reported in either mid-adolescence or early adulthood that were not reported contemporaneously in childhood or adolescence.
d CluedoTM is a murder mystery board game.
Although no specific phenomenological characteristics were found that consistently related to differing trajectories of reoccurrence or cessation over time, with some exceptions, those whose hallucinations and delusions ceased by mid-late adolescence reported fewer hallucinatory or delusional phenomena in early adolescence compared to those who reported reoccurring experiences. Furthermore, two young people who reported reoccurring hallucination and delusions were the only individuals to report these phenomena across all four domains in early adolescence.
Consistency of reporting between early adolescence and early adulthood
As evident in Table 2, there was a high level of inconsistent reporting across the sample over time. Most individuals did not remember, recall or re-report hallucinations and/or delusions they had previously reported at an earlier time point. This was particularly the case for hallucinations and delusions reported in early adolescence, even among individuals who reported vivid, detailed and complex hallucinations or delusions. Only two individuals who reported voice-hearing in early adolescence re-reported their childhood voice-hearing experiences after that time, only one of whom recalled the exact nature of the experience. It was more common for individuals to re-report specific phenomena between mid-adolescence and early adulthood. Furthermore, eight individuals retrospectively reported childhood hallucinations or delusions in mid-adolescence or early adulthood that they had not reported prospectively at an earlier time point.
Phenomenological findings in those with reoccurring hallucinations and delusions
In early adulthood, two typologies of hallucinatory and delusional experiences were identified among young people who reported reoccurring hallucinations and delusions (N = 6). We defined the first typology as ‘Paranormal Perceptions and Beliefs’ (Paranormal typology). It was characterised by hallucinations and/or delusions that were exclusively attributed to spiritual or paranormal beliefs and were not experienced as a source of distress. The experiences of three individuals were classified within this typology. We defined the second typology as ‘Pathological Perceptions and Beliefs’ (Pathological typology). These were characterised by a more nuanced and complex pattern of hallucinations and delusions that were more ‘psychotic-like’ in nature. They typically involved delusion-like beliefs and related experiences that were aligned to individuals’ mood states and a source of distress. The experiences of the remaining three individuals with reoccurring hallucinations and delusions were classified within this typology. Mid-adolescence was identified as the key period for identifying the emergence of the typological patterns identified in those young people who reported these phenomena into early adulthood.
One individual within the Paranormal typology had a diagnosis of autism spectrum disorder, with a history of co-morbid behavioural, anxiety and mood disorders in childhood and adolescence. The other two individuals within this typology had a history of childhood mood disorders. Although one also met criteria for a depressive disorder in mid-adolescence, neither had a recent diagnosis of any mental disorder in early adulthood. In those whose experiences were classified within the Pathological typology, two individuals had been diagnosed with emotionally unstable personality disorder (EUPD) in the months preceding their early adult interview. The other individual within this typology had been diagnosed with both a mood and a dissociative disorder in late adolescence.
Intrapersonal and subcultural factors in individuals with reoccurring hallucinations and delusions
Intrapersonal and subcultural factors reported both in mid-adolescence and early adulthood discriminated between experiences within the Paranormal and the Pathological typology. Intrapersonal factors related to how individual’s integrated and appraised their experiences. Subcultural factors related to the degree to which their experiences were shared or validated by others. All themes were interrelated.
Intrapersonal factors
Two intrapersonal themes were identified that discriminated between the experiences of those within the Paranormal and the Pathological typologies.
Theme 1: source
This theme relates to whether young people perceived their experiences as originating internally, as a reflection of their conscious or unconscious emotional states and emotions, or externally, caused by entities or forces outside of themselves.
The existence of external entities, in the form of Gods, spirits and ghosts, was the dominant belief held by those with Paranormal Perceptions and Beliefs. This belief system provided them with an externally derived source to which they could attribute all unusual perceptual experiences and was held with unwavering conviction.
‘Like, after we did the Ouija board, I’d be lying in bed and something would scratch me…or there would be a perfectly circular bruise somewhere. Yeah, you would see it. And, yeah, sometimes you feel it being done. Like someone would grip me sharp and tight one night. And, then another night, it actually, like hit me’. [Tom describing experiences relating to a ghost touching him at night]
‘But I have occasionally felt, just a malevolent presence in the area. Sure, I remember. testing out one of my little exorcism spells, and one of the doors opened itself wide and slammed itself shut full force’. [Ben]
Conversely, all three young people who reported Pathological Perceptions and Beliefs perceived at least some of their experiences to have originated from and to reflect their internal mood states and/or aspects of their unconscious.
‘I used to think that people could hear my thoughts when I was on like the bus, but that’s, that’s again during my really, like, bad period in school. So I don’t know if it was to do with, like, feeling so down. But yeah I was, like, convinced they could hear my thoughts’. [Emma]
‘There was a time. It would have been around fifth year, so, kind of maybe two years ago. Em, I wouldn’t say I saw people. No, I didn’t. I felt people. It was kind of like I, I got, I got very very depressed in fifth year. And I would say that kind of depression lasted, and anxious and anxiety came out of that then very strongly as well. But there was a time where, em, like, I didn’t feel I deserved to sleep in my bed. So I would sleep on the floor. But I remember I felt like people were standing over me and, and it was almost like I could see them in my mind’s eye if that makes sense. I guess the way people describe the mind’s eye. Em, but that, that’s mainly around low moods in, in times of high anxiety stuff like that would happen’. [Scott]
‘So when I had real bad anxiety I had like mad hypochondria and I just became fixated on HIV. So, like, any time anything came up about HIV on the telly I had it, d’you know what I mean? Someone was telling me I had it. But I could find links to it with everything. I started getting like swollen glands, like I started displaying symptoms of it and everything, like…. I got tested. And then, still, like, It’s kind of like instant relief for a little while. And then it started again. …. I just, like, I just panicked, like, like coming up to my college exams last year I just started freaking out and my mam was just, like, here this has to stop. So we just went and got checked. And now I have, like, I have copped on and realised that I definitely don’t have it like’. [Ava]
Within this subgroup, Ava and Emma also attributed some perceptual phenomena they had experienced to the paranormal. However, their paranormal beliefs were not personally resonant. Rather, they arose from being unable to make sense of the experience or distancing themselves from a psychopathological explanation.
‘Yeah, well, again, either hallucination - you see like you have really got limited options when things like that happen - it’s either you’re crazy or, it’s a ghost. That’s the most reasonable and not frightening’. [Emma]
‘And there was nothing. No, like, source of an alarm. But then that freaked me out then because I started to actually question my mental health. I thought I was going schizophrenic or something as well… I was watching out for other things so I didn’t get any other symptoms’. [Ava]
Theme 2: appraisals
This theme is about whether hallucinations or delusions were viewed as either a positive and welcome aspect of individuals’ lives or negative and unwelcome experiences. For Ross, Tom and Ben, who were classified within the Paranormal typology, even though the experiences could evoke fear, these individuals valued their beliefs and experiences and reported them as a positive aspect of their life.
‘I love telling these stories because people think I’m actually crazy’. [Tom]
‘When you said that at the start I couldn’t wait to get onto this topic. I, I know you said you have a belief in this, and I do as well…I still remember in my, in my Mam and Dad’s house, my Mam and step-Dad’s house, eh, I remember telling someone like I seen someone, like hands coming at me and stuff.’ [Ross]
Although not exclusively the case, many of the hallucinations and/or delusions reported by the three young people within the Pathological typology were appraised negatively. This was particularly the case for unusual thoughts and beliefs, which were typically a source of discomfort, distress and/or shame.
‘I don’t. Sorry, I don’t really like, eh, vocalising it, because it makes me feel, eh, mad I guess’. [Scott]
Subcultural factors
Theme 3: cultural validation
This theme relates to whether young people’s experiences were validated by other people. This involves the subthemes of acceptance or rejection of hallucinations and delusions by others, connections to subcultural communities and the promotion or discouragement of hallucinations and delusions.
All three individuals within the Paranormal typology found a subcultural context within which their experiences could be validated and have meaning. Ross and Tom received positive validation and a sharing of their experiences with multiple individuals within their network of family and friends. Ben’s beliefs were rejected by his parents but he successfully sought out validation for his beliefs through online fora and platforms. This provided these individuals with a sense of connection to like-minded others and grounded their experiences in a meaningful subcultural context.
‘There’s one other thing, where like me and my cousin thought we saw a man with, like, a gun or something lean over the gate at my grandparents’ house, which is next door to mine. And then we looked over again and it was just gone. And we just, we still talk about that…I don’t know. We had just been told since we were kids that ghosts is a real thing…like by our grandparents and stuff so, I don’t know, maybe that’s an element of, like, it’s something we have been told for years’. [Tom]
Was at his uncle’s house putting up wallpaper and his friend saw someone upstairs. There was nobody there. Found out that somebody died in that room. Heard singing in that room upstairs the next day. A few weeks later a different friend saw a person upstairs also. Participant definitely thinks it was the woman who used to live there that he heard singing as she used to sing. Participant was scared by it. Was age 14/15 at the time. Participant is convinced that the lady was singing in the room. [Ross]
Conversely, for Ava, Emma and Scott, their hallucinations and/or delusions were either rejected or by others or aligned by others to psychopathology.
‘I got really freaked out by that though. Really scared. And I just went down and I told everyone about it and they were just, like, ‘You’re crazy’. But, like, I’m real prone to worrying and over-analysing things so they won’t feed in… Like, none of my family will feed into any of my things’. [Ava, describing response of her family when she told them she saw a bracelet fly across a room on its own]
For Scott, his experiences resulted in him feel isolated, different and disconnected from others, which was a primary source of distress for him.
‘SCOTT: Because on the one hand I think maybe it’s perfectly normal and no-one vocalises it, they just consider it normal. And on the other hand it’s….maybe it is something different, maybe it is something happening or maybe there is something wrong with me.
INTERVIEWER: Does it upset you that you have that experience at all?
SCOTT: Em, I guess sometimes yeah. Because you know the feeling of being abnormal and stuff or different, you know, because to some extent I always – maybe it sounds a bit strong, but maybe craved conformity. You know, just to, to be the same as other people that like, like I feel like I fit in. So I guess…I guess the feeling that, that it may not be normal, em, makes me feel more separate.
INTERVIEWER: OK. So you are saying that, when it happens, in and of itself, it isn’t necessarily distressing. It’s the fact that it could signify something about you being abnormal that’s more distressing or upsetting?
SCOTT: Yeah…yeah’. [Scott talking about hearing his thoughts aloud]
Discussion
For the first time, we present descriptive longitudinal findings on the phenomenology of hallucinations and delusions in a sample of young people with a childhood history of these phenomena. As has been reported elsewhere (Dominguez et al. Reference Dominguez, Wichers, Lieb, Wittchen and van Os2011, Kelleher et al. Reference Kelleher, Connor, Clarke, Devlin, Harley and Cannon2012a), findings from this study revealed an age-related decline in these phenomena between early adolescence and early adulthood. Among those who reported reoccurring hallucinatory and delusional experiences into their early adult years, we identified two typologies of experience: Paranormal Perceptions and Beliefs and Pathological Perceptions and Beliefs. These typologies emerged in mid-adolescence and continued into early adulthood. Each reflected how individuals’ experiences of hallucinatory and/or delusional phenomena were enmeshed with their emotional or mood states, integrated into their cultural or personal frames of reference and the emotional and cognitive reactions of young people in response to their experiences.
Although most hallucinations and/or delusions are self-limiting (Maijer et al. Reference Maijer, Hayward, Fernyhough, Calkins, Debbané, Jardri, Kelleher, Raballo, Rammou and Scott2019), the complete cessation of voice-hearing during mid-late adolescence in those young people who reported reoccurring hallucinations and/or delusions was a somewhat unexpected finding in this study, particularly given that high levels of voice-hearing have been found in non-clinical adult samples (Peters et al. Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016). This, along with the finding of stronger evidence for multi-modal hallucinations and delusions across non-auditory perceptual domains and unusual thoughts and beliefs during mid- and late-adolescence, raises questions about the dominance of studies that focus on the unimodal phenomenon of voice-hearing. The dominance of voice-hearing studies has meant that other forms of hallucinations and delusions are often neglected in research (Montagnese et al. Reference Montagnese, Leptourgos, Fernyhough, Waters, Laroi, Jardri, McCarthy-Jones, Thomas, Dudley and Taylor2020). This is limiting our understanding of the potential significance of other forms of hallucinations and delusions, such as those found in this study.
A key finding from this study was our identification of two typologies of hallucinatory and delusional experiences. Complementing and extending findings from two previous qualitative studies (Jackson & Fulford Reference Jackson and Fulford1997, Heriot-Maitland et al. Reference Heriot-Maitland, Knight and Peters2012), we found that individuals’ appraisals and attributions of their hallucinations and/or delusions and the degree to which their experiences were integrated meaningfully into their cultural or subcultural world views were the most influential factors influencing how pathological their perceptions and beliefs were (Jackson et al. 1997, Heriot-Maitland et al. Reference Heriot-Maitland, Knight and Peters2012). In all cases, experiences reported by those within the Paranormal typology were exclusively attributed to external paranormal or spiritual forces, appraised positively, and grounded in a meaningful subcultural context. Additionally, the accounts of individuals in this typology were characterised both by the absence of any distress relating to their experiences and by the absence of any identifiable connection between their experiences and beliefs and their underlying mood states. Outside of the field of psychiatric literature, there are many studies documenting paranormally based experiences of hallucinations and delusions. Rabeyron et al. (Reference Rabeyron and Loose2015) report that, as far back as the late 1800s, there is evidence that up to 1 in 10 people will report hallucinatory experiences that they ascribe to the paranormal. Although an association between schizotypy and paranormal beliefs has been found (Hergovich et al. Reference Hergovich, Schott and Arendasy2008), there is a body of evidence that, for many individuals, paranormal beliefs and experiences are not pathological phenomena or associated with underling psychopathology (Jackson et al. Reference Jackson and Fulford1997, Rabeyron & Watt Reference Rabeyron and Watt2010, Rabeyron et al. Reference Rabeyron and Loose2015, Unterrassner et al. Reference Unterrassner, Wyss, Wotruba, Ajdacic-Gross, Haker and Rossler2017). The fact that many psychiatry researchers recruit individuals with ‘non-clinical’ hallucinations and/or delusions through psychic, paranormal and spiritualist organisations (e.g. Peters et al. Reference Peters, Ward, Jackson, Morgan, Charalambides, McGuire, Woodruff, Jacobsen, Chadwick and Garety2016) suggests that there is an implicit understanding that, although the hallucinatory and delusional experiences reported by those aligned to spiritualism and the paranormal may be phenomenologically similar to those in clinical samples, they are qualitatively different to pathological symptoms of psychosis. In this context, the experiences described by those within the Paranormal typology did not demonstrate characteristics that were ‘psychotic-like’ in nature.
Conversely, those in the Pathological typology perceived at least some of their experiences to be a reflection of their poor mental health and labelled them as negative and unwelcome experiences. In all three cases, there was evidence of delusion-like thinking (Oyebode Reference Oyebode2015), the qualities of which could be characterised as ‘psychotic-like’ in nature. For example, Ava reported somatic delusions with related ideas of reference, thought broadcasting beliefs and delusional mood. A notable finding was that only individuals who had been diagnosed with either EUPD or a dissociative disorder were classified within this typology. This finding is consistent with evidence of hallucinations and/or delusions in people who experience dissociative states (Allen et al. Reference Allen, Coyne and Console1997, Longden et al. Reference Longden, Madill and Waterman2012) and personality disorders (Allen et al. Reference Allen, Coyne and Console1997, Schroeder et al. Reference Schroeder, Fisher and Schäfer2013, Merrett et al. Reference Merrett, Rossell and Castle2016, Niemantsverdriet et al. Reference Niemantsverdriet, Slotema, Blom, Franken, Hoek, Sommer and van der Gaag2017, Cavelti et al. Reference Cavelti, Thompson, Hulbert, Betts, Jackson, Francey, Homan and Chanen2018). Although experiences of hallucinations and delusions in the context of EUPD have been both quantified (Schroeder et al. Reference Schroeder, Fisher and Schäfer2013, Merrett et al. Reference Merrett, Rossell and Castle2016, Niemantsverdriet et al. Reference Niemantsverdriet, Slotema, Blom, Franken, Hoek, Sommer and van der Gaag2017) and described (Wallis et al. Reference Wallis, Denno, Ives, Mallikarjun, Wood, Oyebode, Broome and Upthegrove2020), heretofore, the direction of research has been to examine the prevalence or phenomenology of hallucinations and/or delusions in individuals who have been diagnosed with a personality disorder, EUPD in particular (Schroeder et al. Reference Schroeder, Fisher and Schäfer2013, Niemantsverdriet et al. Reference Niemantsverdriet, Slotema, Blom, Franken, Hoek, Sommer and van der Gaag2017, Wallis et al. Reference Wallis, Denno, Ives, Mallikarjun, Wood, Oyebode, Broome and Upthegrove2020). That research suggests that between 26 and 54% of people with a diagnosis of EUPD experience hallucinations across all modalities (Niemantsverdriet et al. Reference Niemantsverdriet, Slotema, Blom, Franken, Hoek, Sommer and van der Gaag2017). Delusions are also commonly reported by people with EUPD (Yee et al. Reference Yee, Korner, McSwiggan, Meares and Stevenson2005, Kingdon et al. Reference Kingdon, Ashcroft, Bhandari, Gleeson, Warikoo, Symons, Taylor, Lucas, Mahendra and Ghosh2010). These findings mirror our finding of both multi-modal perceptual experiences and delusion-like beliefs among young people with EUPD. However, in contrast to evidence that an estimated 50% of people with EUPD report voice-hearing (Merrett et al. Reference Merrett, Rossell and Castle2016), while most young people in our nested qualitative sample had a history of voice-hearing in childhood, neither of the young people with reoccurring hallucinations and/or delusions and a diagnosis of EUPD reported hearing voices in young adulthood. Our small sample size may explain this difference. However, our finding of hallucinations and/or delusions in young adults with a diagnosis of EUPD did mirror findings on the nature and impact of hallucinatory and delusional experiences in individuals with EUPD. Specifically, that they are more pathological in nature, a source of distress and experienced over a long duration (Merrett et al. Reference Merrett, Rossell and Castle2016, Niemantsverdriet et al. Reference Niemantsverdriet, Slotema, Blom, Franken, Hoek, Sommer and van der Gaag2017).
Importantly, not all experiences reported by those within the Pathological typology were understood as a reflection of underlying emotional or mental health issues. Two of the individuals within this typology did align some of their unexplained perceptual experiences to the paranormal. However, their explanations involving ghosts or other paranormal activity appeared to act as a ‘cultural buffer’ (Rabeyron et al. Reference Rabeyron and Loose2015). Rather than being grounded in an integrated paranormal belief system, their paranormal explanations provided these young people with a means of distancing themselves (Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020) from any association with psychosis (Larøi et al. Reference Larøi, Luhrmann, Bell, Christian, Deshpande, Fernyhough, Jenkins and Woods2014). In this way, the adoption of a paranormal attribution for perceptual experiences in these individuals was qualitatively different to the subgroup of individuals whose strong paranormal beliefs provided them with an acceptable and culturally contextualised way to make sense of their experiences.
Consistency of reporting
The level of inconsistent reporting over time is an important secondary finding in this study. It suggests that young people may interpret questions about hallucinations and delusions differently at different developmental stages, do not remember earlier childhood experiences or choose not to disclose childhood hallucinations or delusions during their adolescent or early adult years. At the time of their early adulthood qualitative interviews, young people in this study were not reminded of any hallucinations or delusions they had previously reported. Future prospective studies that explicitly prompt and remind individuals about previously reported experiences may offer new and important insights into the dynamics of remembering or reporting hallucinatory and delusional phenomena at different developmental phases of the lifespan.
The language of unusual perceptual experiences, thoughts and beliefs
Findings from this study suggest that hallucinations and/or delusions experienced by young people ebb and flow over time and are typically not experienced continuously or with the same phenomenological qualities. It is for this reason that we use the term reoccurrence rather than persistence to describe these phenomena in young people who experienced them over time. We suggest that the term persistence should only be used in instances where hallucinations and/or delusions are experienced continuously. While this linguistic issue may appear to be of marginal importance, it is widely recognised that the contexts within which words are used affect how those words are interpreted and understood (Innis Reference Innis and Hörmann1986). Thus, a word that erroneously suggests persisting hallucinations and/or delusions in young people has the potential to be both misleading and stigmatising (Sato Reference Sato2006, Rogers & Pilgrim Reference Rogers and Pilgrim2014). A similar argument applies to the use of the term ‘psychotic experiences’. As this study has demonstrated, many hallucinations and/or delusions are not psychotic-like in nature, raising questions about the widespread use of the term psychotic experiences to characterise such a diverse range of phenomena and beliefs (Coughlan et al. Reference Coughlan, Healy, Humphries, Clarke, Kelleher and Cannon2020).
Strengths and limitations
Access to longitudinal data spanning 9 years from early adolescence to early adulthood is a notable strength of this study. The fact that data were collected by psychologists, psychiatrists and allied health professional = s using in-depth clinical and qualitative interviews is a further strength. However, the sample size was small and the study is therefore solely descriptive. The small sample size also meant that we were unable to reliably analyse gender and other potentially relevant demographic variables. Additionally, clinical assessments were not conducted in early adulthood. This meant that we were unable to systematically assess for the presence or absence of mental disorders in our sample at that time point. We also acknowledge that EUPD traits may be accentuated in late adolescence and early adulthood, which has relevance to the characteristics of individuals in our Pathological typology. However, our finding of more pathologically expressed phenomena in young people who are given a diagnosis of EUPD is important. As diagnoses of personality disorders are typically made in adulthood, this study may be the first to prospectively document the evolution of hallucinations and/or delusions in individuals who are diagnosed with personality disorders. Our use of prospectively collected data suggest that reoccurring hallucinations and/or delusions that are more pathologically expressed and enmeshed with individuals’ mood states may be a relevant marker of personality dysfunction in young people.
Implications and future research
As suggested by Jackson and Fulford (Reference Jackson and Fulford1997), the distinction between pathological and non-pathological (spiritual) hallucinations and/or delusions depends ‘on the way in which [the] phenomena themselves are embedded in the values and beliefs of the person concerned’. The need for more nuanced conceptualisations and assessments of hallucinations and/or delusions and the lives of young people who report them cannot be understated. This study has highlighted that not all reoccurring experiences of hallucinations and/or delusions are pathological or psychotic-like in nature. However, the field of psychosis and youth mental health research has thus far given limited attention to how factors such as the phenomenology and attributions of hallucinations and delusions may help to discriminate between those that are pathological or psychotic-like in nature and those that are not. This has particular implications for the use of self-report questionnaires in quantitative studies of hallucinations and/or delusions, which typically fail to address the context and ascribed meaning of the phenomena that are endorsed. If any progress is to be made in determining which young people who report hallucinations and/or delusions are at greatest risk for later psychopathology, assessments of hallucinations and/or delusions need to be dimensional in nature (Maijer et al. Reference Maijer, Hayward, Fernyhough, Calkins, Debbané, Jardri, Kelleher, Raballo, Rammou and Scott2019, Montagnese et al. Reference Montagnese, Leptourgos, Fernyhough, Waters, Laroi, Jardri, McCarthy-Jones, Thomas, Dudley and Taylor2020). They should also enable the exploration of the phenomenological characteristics of hallucinations and/or delusions, how young people make sense of them, and the cultural and subcultural contexts within which they integrate or frame their experiences (Jackson et al. Reference Jackson and Fulford1997).
The fact that qualitative, attributional and subcultural factors of reported hallucinations and/or delusions in adolescence were more reliable indicators of future trajectories and typologies in this study indicated that this may be a promising avenue for longitudinal qualitative research on these phenomena in youth samples. Future studies should consider examining combinations of subtypes of phenomena rather than focusing only on individual phenomenological subtypes or replying on a general binary categorisation (i.e. ‘psychotic-like experiences’ versus ‘no psychotic-like experiences’). Additional research with more complex models of these phenomena may provide new and important insights into risk profiles of early manifestations of hallucinations and delusions in the general population.
Conflict of interest
Helen Coughlan has no conflicts of interests to disclose. Colm Healy has no conflicts of interests to disclose. Niamh Humphries has no conflicts of interests to disclose. Mary Clarke has no conflicts of interests to disclose. Mary Cannon has no conflicts of interests to disclose.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. Ethical approval was granted by the Research Ethics Committees of Beaumont Hospital Dublin and the Royal College of Surgeons in Ireland. Participants were compensated for their time with a gift voucher.
Financial support
This work was supported by the Health Research Board (HC, HPF-2015–974; NH, EIA-2017; MCC, HRA-2015; MC, HRA-2015) and the European Research Council (CH, ERC-2016-COG-724809; MC, ERC-2016-COG-724809).








