Introduction
Over the past few decades, adolescent suicide has become a major public health concern. According to the United Nations International Children’s Emergency Fund, suicide is the fifth leading cause of death in adolescents aged 10–19 years worldwide (UNICEF, 2021). Suicidality, including suicidal ideation (SI), plans (SP) and attempts (SA), is reported to be the precursor of suicide death (Nock et al., Reference Nock, Borges, Bromet, Alonso, Angermeyer, Beautrais, Bruffaerts, Chiu, de Girolamo, Gluzman, de Graaf, Gureje, Haro, Huang, Karam, Kessler, Lepine, Levinson, Medina-Mora, Ono, Posada-Villa and Williams2008). The global prevalence rates of SI, SP and SA among adolescents aged 12–15 years are estimated to be 16.5%, 16.5% and 16.4%, respectively (Tang et al., Reference Tang, Yu, Wilcox, Kang, Wang, Wang, Wu and Chen2020). In China, a cross-sectional study involving 7,986 middle school students reported that the prevalence rates of SI, SP and SA were 22.9%, 10.8% and 4.7%, respectively (Xie et al., Reference Xie, Xu, Wang, Wu, Tao, Wan and Tao2022). As the prevalence of suicidality is high in early adolescents, there is an urgent need to identify modifiable risk factors to inform the development of effective suicide prevention and intervention strategies.
Recently, the potential beneficial roles of vitamin D in mental and brain health have increasingly gained attention (Focker et al., Reference Focker, Antel, Ring, Hahn, Kanal, Ozturk, Hebebrand and Libuda2017). Previous observational studies and interventional trials have investigated the association between vitamin D status or supplementation and several common psychiatric traits (Cheng et al., Reference Cheng, Huang and Huang2020; Focker et al., Reference Focker, Antel, Ring, Hahn, Kanal, Ozturk, Hebebrand and Libuda2017; Glabska et al., Reference Glabska, Kolota, Lachowicz, Skolmowska, Stachon and Guzek2021; Guzek et al., Reference Guzek, Kolota, Lachowicz, Skolmowska, Stachon and Glabska2021; Jamilian et al., Reference Jamilian, Amirani, Milajerdi, Kolahdooz, Mirzaei, Zaroudi, Ghaderi and Asemi2019), including depression (Li et al., Reference Li, Sun, Wang, Pan, Feng, Ng, Ungvari, Tao, Li, Wang, Xiang and Guo2019; Ronaldson et al., Reference Ronaldson, Arias de la Torre, Gaughran, Bakolis, Hatch, Hotopf and Dregan2022), anxiety (de Koning et al., Reference de Koning, Verweij, Lips, Beekman, Comijs and van Schoor2017; Maddock et al., Reference Maddock, Berry, Geoffroy, Power and Hypponen2013) and psychosis (Lally et al., Reference Lally, Ajnakina, Singh, Gardner-Sood, Stubbs, Stringer, Di Forti, David, Smith, Murray, Howes and Gaughran2019). To the best of our knowledge, limited epidemiological studies have investigated the association between vitamin D and suicidality. Additionally, most of these epidemiological studies were based on cross-sectional or case–control designs and reported inconsistent results (supplementary eTable 1). Some studies reported that peripheral vitamin D was significantly associated with the risks of SI, SA and completed suicide (Grudet et al., Reference Grudet, Malm, Westrin and Brundin2014; Kim et al., Reference Kim, Jeon, Lim, Oh, Shin, Cho, Park, Kim and Shin2020; Umhau et al., Reference Umhau, George, Heaney, Lewis, Ursano, Heilig, Hibbeln and Schwandt2013). However, other studies have reported that vitamin D was not significantly associated with SI (Park et al., Reference Park, Yang, Won Park and Chung2016). One possible explanation for these discrepant results is the usage of different cut-off values for vitamin D levels in these studies [e.g. >30 ng/mL for sufficiency (Park et al., Reference Park, Yang, Won Park and Chung2016); ≥20 ng/mL for sufficiency (Kim et al., Reference Kim, Jeon, Lim, Oh, Shin, Cho, Park, Kim and Shin2020); see details in eTable 1]. Other factors, such as differences in adjusted covariates and population characteristics, may also have contributed to the discrepant results (see eTable 1). Recent studies have suggested the threshold of vitamin D concentration below which disease risk and vitamin D supplementation benefits can be observed, indicating a non-linear relationship between vitamin D and some chronic diseases (Scragg, Reference Scragg2018). Therefore, both linearity and non-linearity should be considered when investigating the relationship between vitamin D and suicidality risk.
Traditional observational studies are susceptible to confounding bias and reverse causality, limiting their ability to draw causal inferences. Mendelian randomization (MR), as a natural analogue of randomized controlled trials, offers an opportunity to detect possible causal effects in a time-efficient and cost-effective manner and has been applied in the field of nutritional psychiatry (Carnegie et al., Reference Carnegie, Zheng, Sallis, Jones, Wade, Evans, Zammit, Munafo and Martin2020; Wootton et al., Reference Wootton, Jones and Sallis2022). Recently, the causal role of vitamin D in some psychiatric conditions, such as depression (Libuda et al., Reference Libuda, Laabs, Ludwig, Buhlmeier, Antel, Hinney, Naaresh, Focker, Hebebrand, Konig and Peters2019; Mulugeta et al., Reference Mulugeta, Lumsden and Hypponen2020) and schizophrenia (Taylor et al., Reference Taylor, Burgess, Ware, Gage, Richards, Davey Smith and Munafo2016), has been examined using MR. However, traditional MR is based on the hypothesis that the association between exposure and outcome is linear. To overcome this limitation, non-linear MR has been developed and used to investigate the causal effect of vitamin D on some medical outcomes (Navale et al., Reference Navale, Mulugeta, Zhou, Llewellyn and Hypponen2022; Sutherland et al., Reference Sutherland, Zhou and Hypponen2022; Zhou et al., Reference Zhou, Selvanayagam and Hypponen2022). Thus, both linear and non-linear MR methods should be employed to explore the causal effect of vitamin D on suicidality.
One case–control study constructed a genetic risk score (GRS) using four vitamin D–related gene polymorphisms (namely, DHCR7-rs12785878, CYP2R1-rs10741657, GC-rs2282679 and CYP24A1-rs6013897). GRS analysis showed a higher risk of attempted suicide with a greater number of low vitamin D alleles in men but not in women (Wei et al., Reference Wei, Liu, Qiu, Zhang, Wang and Jia2021), indicating a sex-specific relationship. Additionally, the relationship between vitamin D and other mental problems was reported to be sex-specific (Hinata et al., Reference Hinata, Kitamura, Watanabe, Kabasawa, Saito, Takahashi, Takachi, Kobayashi, Oshiki, Iki, Tsugane, Sasaki, Watanabe and Nakamura2023; Wang et al., Reference Wang, Yuan, Chang, Li, Blum and Su2022). However, most previous studies on vitamin D and suicidality matched sex or adjusted sex as a covariate in the statistical models, which would overlook the sex differences. Therefore, sex-stratified analysis is needed to examine whether vitamin D affects suicidality in a sex-dependent manner.
Additionally, previous studies examining the relationship between vitamin D and suicidality were mainly conducted in adults. To the best of our knowledge, only one case–control study was conducted in adolescents and revealed that the mean vitamin D levels were significantly decreased in patients who attempted suicide (Gokalp, Reference Gokalp2020). Early adolescence (10–14 years of age), which represents a transition period from childhood to adolescence, is characterized by immense cognitive and emotional changes. Previous studies have reported that the incidence of the first onset of suicidality peaks during early adolescence (van Vuuren et al., Reference van Vuuren, van der Wal, Cuijpers and Chinapaw2021) and increases with age. Meanwhile, the prevalence of vitamin D deficiency tends to increase rapidly from childhood to early adolescence (Hu et al., Reference Hu, Jiang, Lu, Yang, Yang and Yang2022a) due to increased academic burden and decreased outdoor activities. Therefore, there is a need to investigate the causal effect of vitamin D on suicidality in early adolescence, which will provide new insights for implementing a feasible programme for suicide prevention and intervention.
This study aimed to use data from a Chinese early adolescent cohort to investigate the relationship of serum 25-hydroxyvitamin D [25(OH)D, an improved indicator of vitamin D stores] with the risk of suicidality. Traditional statistical methods were used to investigate the observational association of the baseline 25(OH)D concentration or levels with baseline and incident suicidality. Next, linear and non-linear MR methods were employed to establish the causal association of baseline 25(OH)D concentration with baseline and incident suicidality. Additionally, sex-stratified analysis was performed to determine sex differences in the observational and causal associations of baseline 25(OH)D with baseline and incident suicidality risk.
Methods
This study was approved by the ethical committee of Anhui Medical University (No. 20180083) and complied with the guidelines of the Declaration of Helsinki. All school leaders, adolescents and their caregivers participating in the study signed an informed consent form. The Strengthening the Reporting of Observational studies in Epidemiology (STROBE) and STROBE-MR guidelines were followed for reporting observational and MR studies, respectively (Skrivankova et al., Reference Skrivankova, Richmond, Woolf, Yarmolinsky, Davies, Swanson, VanderWeele, Higgins, Timpson, Dimou, Langenberg, Golub, Loder, Gallo, Tybjaerg-Hansen, Davey Smith, Egger and Richards2021; von Elm et al., Reference von Elm, Altman, Egger, Pocock, Gotzsche, Vandenbroucke and Initiative2007). Detailed information on these two checklists is shown in eTables 2 and 3.
Study settings and participants
In this study, data were obtained from the Chinese Early Adolescents Cohort (CEAC) (Wang et al., Reference Wang, Yuan, Chang, Li, Blum and Su2022). The CEAC is an annual three-wave longitudinal study to examine the risk factors associated with emotional and behavioural problems in Chinese early adolescents. This study included 1,814 participants from one middle school in Huaibei City (Anhui Province, China) who provided written informed consent. The exclusion criteria were as follows: severe liver/renal diseases, physical disabilities, severe injuries or infection, the use of psychiatric medications and incomplete questionnaire data on covariates and/or suicidality. In total, 1,426 students with complete data on serum 25(OH)D concentration, covariates and suicidality were included for baseline suicidality analysis using traditional observational methods. Of these 1,426 participants, only those students who reported no suicidality at baseline were included for incident suicidality analysis using the traditional observational method (SI: 1,083; SP: 1,282; SA: 1,404). In total, 1,411 students with complete data on serum 25(OH)D concentration, covariates, suicidality and vitamin D–related genotypes were included for baseline suicidality analysis using the MR method. Of these 1,411 participants, only those students who reported no suicidality at baseline were included for incident suicidality analysis using the MR method (SI: 1072; SP: 1,269; SA: 1,389). Further details on the selection process of the study participants are provided in online supplementary eFigure 1.
Measurements
Baseline serum 25(OH)D concentration
At baseline, fasting blood samples were collected from participants in the morning. The blood samples were centrifuged to obtain the serum. The serum samples were aliquoted and stored at −80℃ until further use. In December 2021, the baseline serum 25(OH)D concentration (ng/mL) was measured using the LIASON 25-OH vitamin D TOTAL assay (DiaSorin, Inc.). Based on previous studies (Cheng et al., Reference Cheng, Chen, Li, Pei, Fan, He, Liu, Liu, Zhang and Cheng2022; Hu et al., Reference Hu, Zhi, Ma, Li, Wang, Zhu, Li and Zhang2022b), the serum 25(OH)D levels were grouped into the following three categories: sufficiency (≥30 ng/mL), insufficiency (≥20 and < 30 ng/mL) and deficiency (<20 ng/mL). The distribution of serum 25(OH)D concentration in blood samples was approximately normal (eFigure 2).

Figure 1. The role of proteins encoded by the selected candidate genes in the vitamin D synthesis and metabolism.
Note. DHCR7 and CYP2R1 are involved in vitamin D synthesis. GC, CYP24A1 and CYP27B1 are involved in vitamin D metabolism.
Baseline and incident suicidality
At wave I, suicidality in the past 6 months was assessed. However, at waves II and III, suicidality in the past year was assessed. In each wave, the following three questions were asked: (1) have you ever thought about killing yourself? (SI), (2) have you ever planned to end your life? (SP), and (3) have you ever attempted to take your own life? (SA). The responses were recorded as yes or no. Therefore, SI, SP and SA were treated as dichotomous variables. For baseline suicidality analysis, participants who reported having suicidality at wave I were regarded as having baseline suicidality. For incident suicidality analysis, we calculated two incident suicidality outcomes: (1) 1-year incident suicidality (i.e. reported no suicidality at wave I but reported having suicidality at wave II) and (2) 2-year incident suicidality (i.e. reported no suicidality at wave I but reported having suicidality at waves II and/or III).
Calculation of vitamin D polygenic score
DNA was extracted from the peripheral blood samples collected at baseline. Based on the Chinese genetic background, single-nucleotide polymorphisms (SNPs) were mainly selected in the following two steps: selection of common vitamin D metabolism-related genes (Cheung et al., Reference Cheung, Lau, Sham, Tan and Kung2013; Lu et al., Reference Lu, Sheng, Li, Gan, Liu, Zhu, Loos and Lin2012; Robien et al., Reference Robien, Butler, Wang, Beckman, Walek, Koh and Yuan2013; Zhang et al., Reference Zhang, Wang, Liu, Qu, Qu, Wang and Ren2012; Zhou et al., Reference Zhou, Zhao, Xu, Ye, Travers-Gustafson, Zhou, Wang, Zhang, Lee Hamm, Deng, Recker and Lappe2014) (Fig. 1) and selection of key SNPs in these genes (Ahn et al., Reference Ahn, Yu, Stolzenberg-Solomon, Simon, McCullough, Gallicchio, Jacobs, Ascherio, Helzlsouer, Jacobs, Li, Weinstein, Purdue, Virtamo, Horst, Wheeler, Chanock, Hunter, Hayes, Kraft and Albanes2010; Wang et al., Reference Wang, Zhang, Richards, Kestenbaum, van Meurs, Berry, Kiel, Streeten, Ohlsson, Koller, Peltonen, Cooper, O’Reilly, Houston, Glazer, Vandenput, Peacock, Shi, Rivadeneira, McCarthy, Anneli, de Boer, Mangino, Kato, Smyth, Booth, Jacques, Burke, Goodarzi, Cheung, Wolf, Rice, Goltzman, Hidiroglou, Ladouceur, Wareham, Hocking, Hart, Arden, Cooper, Malik, Fraser, Hartikainen, Zhai, Macdonald, Forouhi, Loos, Reid, Hakim, Dennison, Liu, Power, Stevens, Jaana, Vasan, Soranzo, Bojunga, Psaty, Lorentzon, Foroud, Harris, Hofman, Jansson, Cauley, Uitterlinden, Gibson, Jarvelin, Karasik, Siscovick, Econs, Kritchevsky, Florez, Todd, Dupuis, Hypponen and Spector2010) Finally, five SNPs (rs10741657, rs6013897, rs1790349, rs4588 and rs7041) located in four genes were selected (Table 1). In December 2021, SNPs were genotyped using the Sequenom MassARRAY iPLEX platform (Agena Bioscience, Inc., San Diego, CA, USA). An unweighted vitamin D polygenic score (VD-PGS) was calculated for further MR analysis (Supplementary eMethods). The higher the VD-PGS, the lower the 25(OH)D concentration (eTable 4).
Table 1. Basic characteristics of the candidate genes
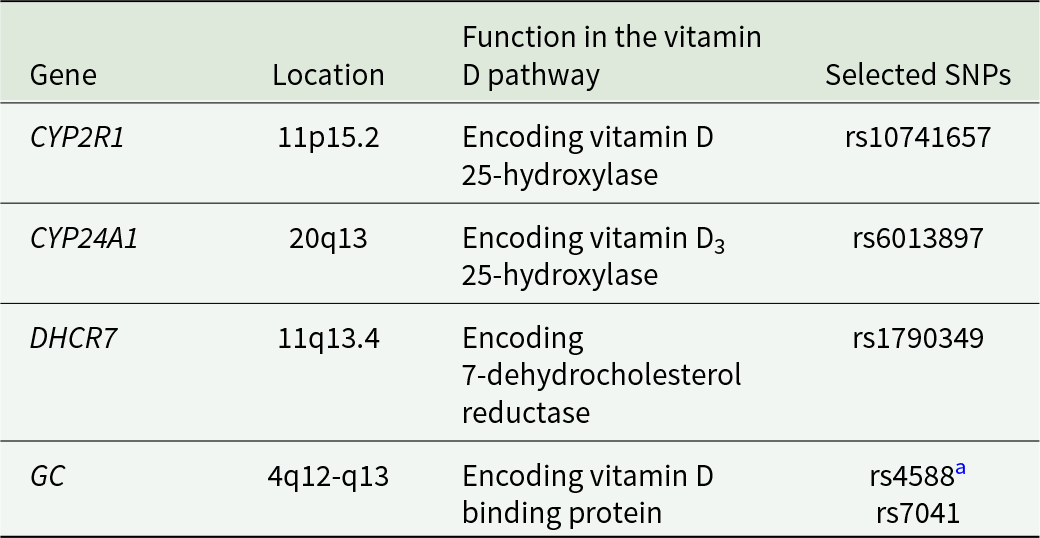
SNPs, single-nucleotide polymorphism
a indicates that rs4588 is in high-LD with rs2282679.
Identification of genetic instrument variables
The selection of instrument variables (IVs) needs to satisfy three IV assumptions (Lousdal, Reference Lousdal2018). To reduce weak genetic instrument bias, the association between each SNP and vitamin D was examined. Two SNPs (rs6013897 and rs1790349) that were not significantly related to serum 25(OH)D concentration were excluded (eTable 5). Finally, three SNPs (rs10741657, rs4588 and rs7041) were included (Supplementary eMethods). To assess the adequacy of IVs, the serum 25(OH)D concentration was regressed on VD-PGS with adjustment for age and sex to obtain the proportion of variance explained by the specified SNPs (i.e. R 2). The F-statistic was calculated as follows: F = ${{{R^2} \times \left( {N - 2} \right)} \over {1 - {R^2}}}$ (N represents the total sample size) (Yin et al., Reference Yin, Huang, Wang, Yang, Tao, Li, Ni and Pan2022). Generally, F > 10 was considered to have sufficient genetic instrument strength (Pierce et al., Reference Pierce, Ahsan and Vanderweele2011). Additionally, the association between VD-PGS and potential risk factors for suicidality was examined to explore the presence of horizontal pleiotropic effects.
${{{R^2} \times \left( {N - 2} \right)} \over {1 - {R^2}}}$ (N represents the total sample size) (Yin et al., Reference Yin, Huang, Wang, Yang, Tao, Li, Ni and Pan2022). Generally, F > 10 was considered to have sufficient genetic instrument strength (Pierce et al., Reference Pierce, Ahsan and Vanderweele2011). Additionally, the association between VD-PGS and potential risk factors for suicidality was examined to explore the presence of horizontal pleiotropic effects.
Covariates
Potential covariates were identified based on previous literature investigating the causal risk factors for vitamin D among children and adolescents (Arguelles et al., Reference Arguelles, Langman, Ariza, Ali, Dilley, Price, Liu, Zhang, Hong, Wang, Xing, Li, Liu, Zhang, Xu and Wang2009; Hu et al., Reference Hu, Chen, Wang, Li, Yun, Li, Yang, Piao, Yang and Yang2017; Mulugeta et al., Reference Mulugeta, Lumsden and Hypponen2020; Revez et al., Reference Revez, Lin, Qiao, Xue, Holtz, Zhu, Zeng, Wang, Sidorenko, Kemper, Vinkhuyzen, Frater, Eyles, Burne, Mitchell, Martin, Zhu, Visscher, Yang, Wray and McGrath2020; Tolppanen et al., Reference Tolppanen, Fraser, Fraser and Lawlor2012). The predictors of adolescent suicidality (Abreu et al., Reference Abreu, Oquendo, Galfavy, Burke, Grunebaum, Sher, Sullivan, Sublette, Mann and Lafer2018; Carballo et al., Reference Carballo, Llorente, Kehrmann, Flamarique, Zuddas, Purper-Ouakil, Hoekstra, Coghill, Schulze, Dittmann, Buitelaar, Castro-Fornieles, Lievesley, Santosh, Arango and Consortium2020; Miranda-Mendizabal et al., Reference Miranda-Mendizabal, Castellvi, Pares-Badell, Alayo, Almenara, Alonso, Blasco, Cebria, Gabilondo, Gili, Lagares, Piqueras, Rodriguez-Jimenez, Rodriguez-Marin, Roca, Soto-Sanz, Vilagut and Alonso2019), especially in China (Liu et al., Reference Liu, Chen, Liu, Wang and Jia2019), were identified. Next, a directed acyclic graph was used to identify a set of minimal sufficient covariates (eFigure 3). Mood disorders, anxiety disorders and substance misuse are the most prevalent psychiatric morbidities in individuals with suicidality (Knipe et al., Reference Knipe, Williams, Hannam-Swain, Upton, Brown, Bandara, Chang and Kapur2019). Among Chinese early adolescents, attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), generalized anxiety disorder and major depressive disorder are the most common psychiatric disorders (Shen et al., Reference Shen, Chan, Liu, Zhou, Cui, He, Fang, Xiang and Luo2018). The trait-impulsivity etiological model posits impulsivity as the underlying construct shared in many externalizing problems (e.g. substance misuse, ADHD and ODD) (Beauchaine et al., Reference Beauchaine, Zisner and Sauder2017; Martel et al., Reference Martel, Levinson, Lee and Smith2017; Rodenacker et al., Reference Rodenacker, Hautmann, Gortz-Dorten and Dopfner2018), which could strongly predict adolescent suicidality (Gorlyn, Reference Gorlyn2005). Thus, depression, anxiety and impulsivity were selected as comorbid psychiatric covariates in this study. Information on the prevalence of psychiatric comorbidities in suicidality among the study participants is shown in eTable 6. Finally, adjusted covariates in the traditional observational analysis of this study included sex, age, household registration, family economy, paternal education, maternal education, moderate physical activity, vigorous physical activity and psychiatric comorbidities (i.e. impulsivity, depression and anxiety). Furthermore, only sex and age were adjusted in MR analysis. Detailed information on these covariates is provided in eTable 7.
Statistical analysis
Descriptive statistics including the mean [standard deviation (SD)] for continuous variables and the number of participants (%) for categorical variables were used to describe the basic characteristics of the study participants.
For traditional observational analysis, logistic regression models were constructed to calculate odds ratios (ORs) for suicidality based on the continuous serum 25(OH)D concentration and categorical 25(OH)D levels with adjustments for potential covariates. Additionally, fractional polynomial models were constructed to determine the appropriate functional form of continuous 25(OH)D concentration. Likelihood ratio tests were performed to compare the best-fitting fractional polynomial model against the linear model. A P-value <.05 indicated the presence of a non-linear association.
For MR analysis, both linear [the ratio of coefficients method (Burgess et al., Reference Burgess, Small and Thompson2017)] and non-linear MR (Staley and Burgess, Reference Staley and Burgess2017) methods were employed to examine the association between genetically determined serum 25(OH)D concentration and the risk of suicidality using individual-level data. For linear MR, linear regression models were employed to estimate the effect of the genetic instrument (VD-PGS) on vitamin D ( ${\hat \beta _{X|Z}}$) and logistic regression models were subsequently used to estimate the effect of VD-PRS on suicidality risk (
${\hat \beta _{X|Z}}$) and logistic regression models were subsequently used to estimate the effect of VD-PRS on suicidality risk ( ${\hat \beta _{Y|Z}}$). Both regressions were adjusted for age and sex. Linear MR estimates can be expressed as
${\hat \beta _{Y|Z}}$). Both regressions were adjusted for age and sex. Linear MR estimates can be expressed as  ${{{{\hat \beta }_{Y|Z}}} \over {{{\hat \beta }_{X|Z}}}}$, and their 95% confidence intervals (CIs) can be computed using a first-order Taylor series approximation (Arvanitis et al., Reference Arvanitis, Qi, Bhatt, Post, Chatterjee, Battle and McEvoy2021). For non-linear MR, fractional polynomial models were fitted to localized average causal effects (LACEs) using a meta-regression method. Briefly, the study sample was split into 10 quantiles according to the instrument-free 25(OH)D (residuals of serum 25(OH)D after regressing on VD-PGS). Within each quantile, a linear MR estimate was fitted, known as LACEs. Next, meta-regression of LACEs was performed against quantile-specific mean 25(OH)D by fitting a range of fractional polynomial models of Degrees 1 and 2. The best-fitting model was selected. The following three statistical non-linear tests were reported: the fractional polynomial test, which compares the best-fitting fractional polynomial model of Degree 1 against the linear model; the quadratic test, which assesses the linear trend among LACEs; and the Cochran’s Q, which assesses differences in LACEs across 10 quantiles. Two heterogeneity tests (Cochran’s Q and trend tests) were performed to examine whether the association between VD-PGS and 25(OH)D was constant across 10 quantiles of vitamin D concentration. The statistical power for MR analysis was calculated using the online mRnd website (https://shiny.cnsgenomics.com/mRnd/) (Brion et al., Reference Brion, Shakhbazov and Visscher2013). Notably, bidirectional MR was not performed due to the unavailability of genotype data on suicidality-related SNPs in this study.
${{{{\hat \beta }_{Y|Z}}} \over {{{\hat \beta }_{X|Z}}}}$, and their 95% confidence intervals (CIs) can be computed using a first-order Taylor series approximation (Arvanitis et al., Reference Arvanitis, Qi, Bhatt, Post, Chatterjee, Battle and McEvoy2021). For non-linear MR, fractional polynomial models were fitted to localized average causal effects (LACEs) using a meta-regression method. Briefly, the study sample was split into 10 quantiles according to the instrument-free 25(OH)D (residuals of serum 25(OH)D after regressing on VD-PGS). Within each quantile, a linear MR estimate was fitted, known as LACEs. Next, meta-regression of LACEs was performed against quantile-specific mean 25(OH)D by fitting a range of fractional polynomial models of Degrees 1 and 2. The best-fitting model was selected. The following three statistical non-linear tests were reported: the fractional polynomial test, which compares the best-fitting fractional polynomial model of Degree 1 against the linear model; the quadratic test, which assesses the linear trend among LACEs; and the Cochran’s Q, which assesses differences in LACEs across 10 quantiles. Two heterogeneity tests (Cochran’s Q and trend tests) were performed to examine whether the association between VD-PGS and 25(OH)D was constant across 10 quantiles of vitamin D concentration. The statistical power for MR analysis was calculated using the online mRnd website (https://shiny.cnsgenomics.com/mRnd/) (Brion et al., Reference Brion, Shakhbazov and Visscher2013). Notably, bidirectional MR was not performed due to the unavailability of genotype data on suicidality-related SNPs in this study.
In the sex-stratified analysis, male and female samples were separately analyzed to determine sex differences in the relationship between serum 25(OH)D and suicidality risk. All statistical analyses and figures were generated using R statistical software (version 4.1.0). A two-sided P-value <.05 was considered statistically significant.
Results
A total of 1,426 students (60.8% of males; mean [SD] = 12.48 [0.48]) were included for traditional observational analysis. The mean serum 25(OH)D concentration was 23.12 ng/mL (SD = 5.76 ng/mL). Approximately 30.7%, 57.0% and 12.3% of the participants exhibited 25(OH)D deficiency, insufficiency and sufficiency, respectively. The baseline characteristics of the study participants are presented in eTable 8. At baseline, 24.1%, 10.1% and 1.5% of the participants reported SI, SP and SA, respectively (Table 2). Among the participants who did not report suicidality at baseline, 12.8%, 7.8% and 2.8% reported 1-year incident SI, SP and SA, respectively (Table 2). A total of 25.6%, 13.4% and 4.1% of participants who had no baseline suicidality reported 2-year incident SI, SP and SA, respectively (Table 2). Additionally, 1,411 participants included in the traditional observational analysis who had data on vitamin D–related SNPs were included for subsequent MR analysis. The characteristics of the participants included in the MR analysis were similar to those included in the traditional observational analysis (eTable 8).
Table 2. Traditional observational associations between baseline serum 25(OH)D concentration and the risk of suicidality in the total sample
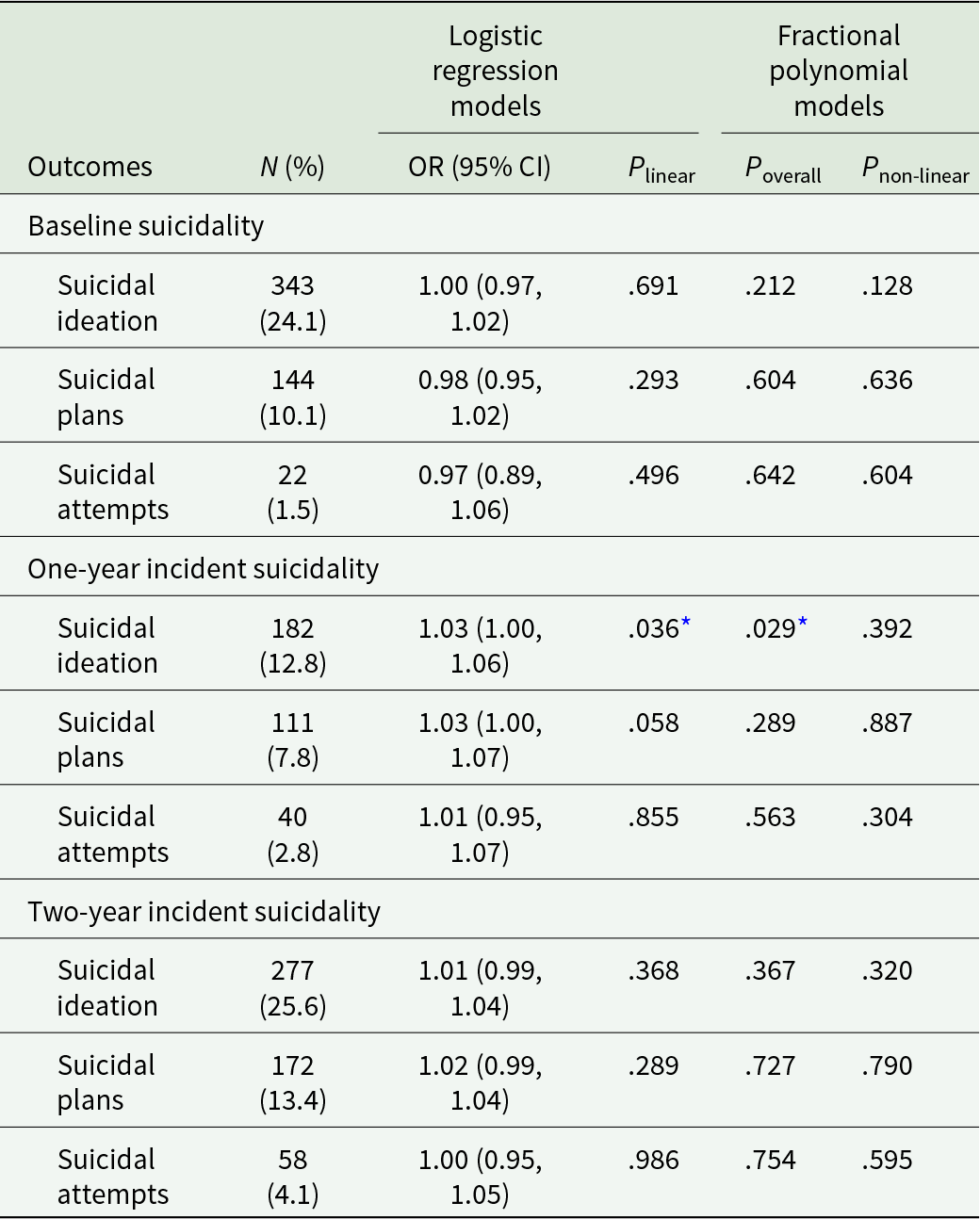
Note. All models adjusted for age, sex, household registration, family economy, paternal education, maternal education, moderate physical activity, vigorous physical activity, impulsivity, depression and anxiety. P linear indicates P-value for logistic regression model. P overall indicates P-value for comparing the best-fitting second-degree model against the null model. P non-linear indicates P-value for comparing the best-fitting second-degree model against the linear model.
* indicates P-value <.05.
Instrument validation
After adjusting for sex and age, VD-PGS was associated with the serum 25(OH)D concentration (β = 0.199, standardized error = 0.026, P < .001), explaining 3.97% (R 2) of the variation (F-statistic = 58.25). No significant heterogeneity was observed in the association between VD-PGS and serum 25(OH)D concentration across 10 quantiles of residual serum 25(OH)D concentration for any suicidality outcomes (P > .05 for all; eFigure 4). Thus, the association between VD-PGS and 25(OH)D associations in the 1st and 10th quantiles appeared to be outliers (eFigure 4). VD-PGS was not associated with potential confounders (P = .204–.977; eTable 9).
Traditional observational analysis
In the multivariable-adjusted logistic regression models (Table 2), the serum 25(OH)D concentration was not significantly associated with the risk of baseline (OR = 0.97–1.00; P linear > .05 for all) and 2-year incident (OR = 1.00–1.02; P linear > .05 for all) suicidality. However, the 25(OH)D concentration was significantly associated with the risk of 1-year incident SI (OR [95% CI] = 1.03 [1.00–1.06], P linear = .036). Additionally, the serum 25(OH)D concentration did not exhibit a significant non-linear association with the risk of baseline (P non-linear = .128–.636) and incident (P non-linear = .304–.887 for 1-year incidence; P non-linear = .320–.790 for 2-year incidence) suicidality outcomes (Table 2). Compared with those in the 25(OH)D deficiency group, the risk of baseline SI was significantly lower (OR [95% CI], 0.69 [0.51–0.92]; P = .012) and the risks of incident SIs were higher (OR [95% CI] = 1.63 [1.11–2.41], P = .013 for 1-year incident SI; OR [95% CI] = 1.42 [1.02–1.96], P = .037 for 2-year incident SI) in the 25(OH)D insufficiency group (Table 3). The risk of baseline or incident suicidality outcomes was not significantly different between the 25(OH)D deficiency and sufficiency groups (Table 3).
Table 3. Traditional observational associations between baseline serum 25(OH)D levels and the risk of suicidality in the total sample
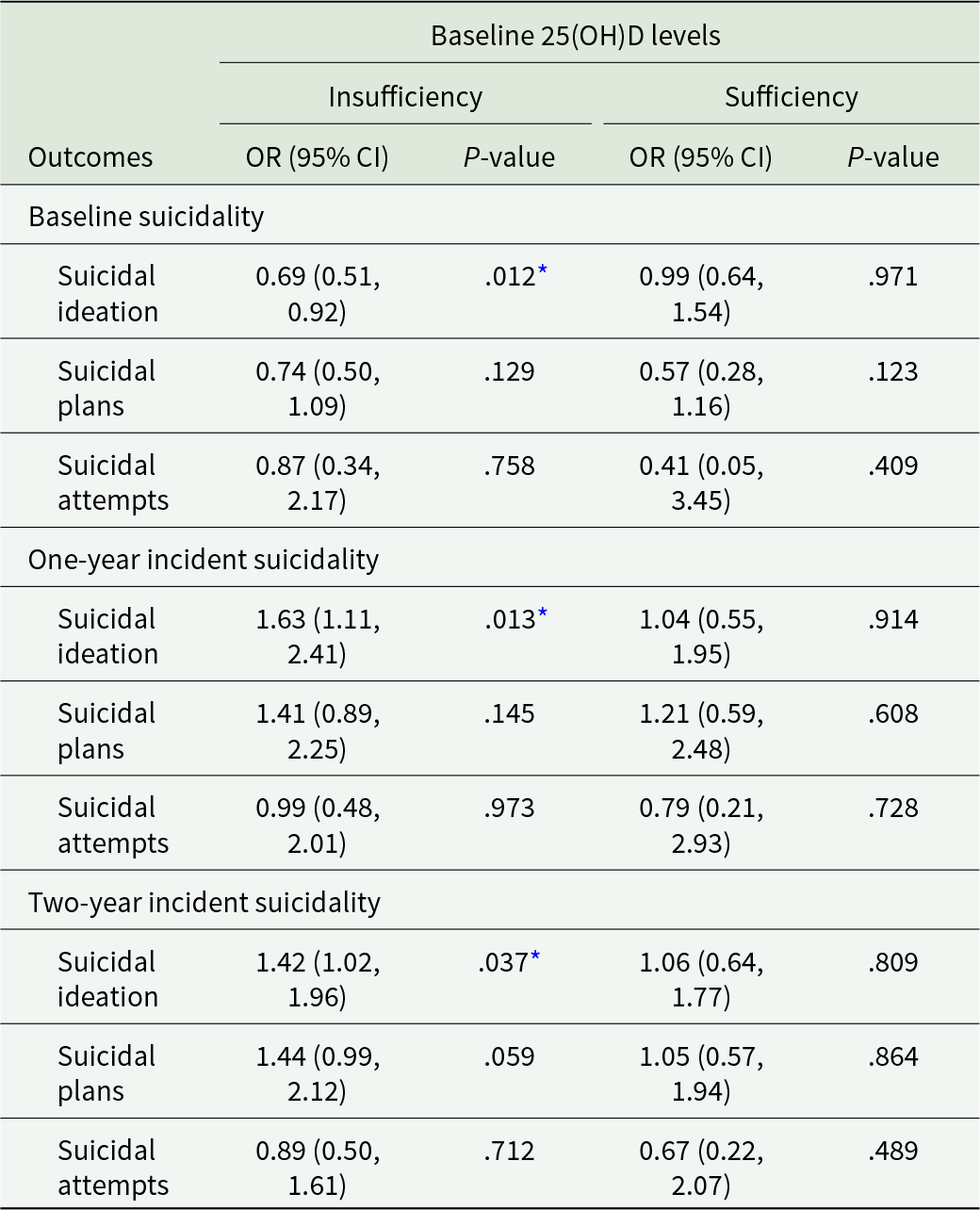
OR, odds ratio; CI, confidence interval.
All logistic regression models were adjusted for sex, age, household registration, family economy, paternal education, maternal education, moderate physical activity, vigorous physical activity, impulsivity, depression and anxiety, with reference to 25(OH)D deficiency group.
* indicates P-value <.05.
MR analysis
Linear MR analysis revealed that no significant linear relationship between serum 25(OH)D concentration and the risk of baseline, 1-year and 2-year incident suicidality outcomes (P linear > .05 for all; Table 4). Additionally, non-linear MR analysis revealed no significant non-linear association between 25(OH)D concentration and the risk of baseline suicidality (P-values for the fractional polynomial, Cochran’s Q and quadratic tests were in the range of .658–1.000, 139–.834 and .754–.975, respectively). There was no significant non-linear MR association between 25(OH)D concentration and the risk of 1-year (P-values for the fractional polynomial, Cochran’s Q and quadratic tests were in the range of .622–.739, .392–.695 and .543–.615, respectively) or 2-year (P-values for the fractional polynomial, Cochran’s Q and quadratic tests were in the range of .343–.530, .403–.594 and .091–.331, respectively) incident suicidality (Table 4). Detailed information on the power calculation for MR analysis is provided in supplementary eTable 10.
Table 4. MR associations between serum 25(OH)D concentration and the risk of suicidality in the total sample

OR, odds ratio; CI, confidence interval; MR, Mendelian randomization.
All MR analyses adjusted for sex and age. P linear indicates P-value for logistic regression model. P fp indicates P-value for fractional polynomial test. P quadratic indicates P-value for quadratic test. P Cochrane’s Q indicates P-value for Cochran’s Q test.
Sex differences
Sex-stratified traditional observational analysis revealed no linear or non-linear relationship between serum 25(OH)D concentration and the risk of baseline or incident suicidality outcomes among men (all P linear and P non-linear > .05; eTable 11). However, the 25(OH)D concentration exhibited a significant non-linear relationship with the risk of baseline SI in women (P non-linear = .001; eTable 12; eFigure 5). When the 25(OH)D concentration was categorized into three levels, the risk of baseline or incident suicidality in the 25(OH)D insufficiency/sufficiency group was not significantly different from that in the 25(OH)D deficiency group among men (all P > .05; eTable 13). However, the risk of baseline SI in the 25(OH)D insufficiency group was lower than that in the 25(OH)D deficiency group among women (OR [95% CI], 0.59 [0.40–0.87]; P = .008) (eTable 14). The 25(OH)D insufficiency group had a higher risk of 1-year incident SI than the deficiency group (OR [95% CI] = 1.78 [1.03–3.09], P = .038) in women (eTable 14). Additionally, sex-stratified MR analysis did not reveal a linear or a non-linear relationship between genetically predicted 25(OH)D concentration and the risk of baseline and incident suicidality outcomes in both men (eTable 15) and women (eTable 16).
Discussion
This study aimed to use traditional observational and MR analyses to investigate the causal effects of 25(OH)D on suicidality in a Chinese early adolescent cohort. Traditional observational analysis did not reveal a significant linear or non-linear association between serum vitamin D concentration and baseline suicidality in the total sample. Interestingly, analysis with the prespecified cut-off values for vitamin D levels revealed that the risk of baseline SI in the serum 25(OH)D deficiency group was significantly higher than that in the 25(OH)D insufficiency group but was not significantly different with that in the 25(OH)D sufficiency group. As different vitamin D cut-off values are used, comparative analysis of findings across different studies is challenging. A cross-sectional study using vitamin D cut-off values similar to those used in this study reported no significant association between vitamin D levels and SI (Park et al., Reference Park, Yang, Won Park and Chung2016). However, another cross-sectional study classified participants with vitamin D levels < 10, 10–20 and ≥20 ng/mL into deficiency, insufficiency and sufficiency groups, respectively (Kim et al., Reference Kim, Jeon, Lim, Oh, Shin, Cho, Park, Kim and Shin2020). The risk of SI in the vitamin D deficiency group was higher than that in the vitamin D sufficiency group (adjusted OR = 1.138; 95% CI = 1.027–1.262). Surprisingly, the risks of 1- and 2-year incident SIs in the 25(OH)D insufficiency group were slightly higher than those in the 25(OH)D deficiency group. However, the association between 25(OH)D levels and the risk of 2-year incident SI disappeared in the sex-stratified analysis, suggesting that this significant association is spurious. Future studies with large sample sizes are needed to confirm the results of incident suicidality analysis with repeated measurements of 25(OH)D. These findings highlighted the importance of sex-stratified analysis rather than controlling for sex as a covariate in statistical models.
In sex-stratified traditional observational analysis, the risk of baseline SI in the 25(OH)D deficiency group was significantly higher than that in the 25(OH)D insufficiency group but was not higher than that in the 25(OH)D sufficiency group in women, indicating the presence of a non-linear association. Indeed, the vitamin D concentration exhibited a significant non-linear association with the risk of baseline SI. Specifically, the risk of baseline SI decreased with increasing 25(OH)D concentration when 25(OH)D was <20 ng/mL and remained stable when 25(OH)D was 20–30 ng/mL. These significant observational associations may be biologically plausible. Vitamin D deficiency can promote inflammation and oxidative stress, increasing the risk of baseline SI. A previous study reported that the concentrations of several biomarkers of inflammation and oxidative stress (malondialdehyde, myeloperoxidase, 3-nitrotyrosine, interleukin-6 and soluble vascular cellular adhesion molecule-1) in participants with vitamin D deficiency were higher than those in participants without deficiency (Filgueiras et al., Reference Filgueiras, Rocha, Novaes and Bressan2020). Inflammation and oxidative stress are reported to be putative factors involved in the pathophysiology of suicidality (Brundin et al., Reference Brundin, Bryleva and Thirtamara Rajamani2017; Koweszko et al., Reference Koweszko, Gierus, Zalewska, Maciejczyk, Waszkiewicz and Szulc2020). Increased inflammation levels have also been identified as a risk factor for various psychiatric disorders, such as bipolar disorder, borderline personality disorder and psychosis (Fraguas et al., Reference Fraguas, Diaz-Caneja, Ayora, Hernandez-Alvarez, Rodriguez-Quiroga, Recio, Leza and Arango2019; Saccaro et al., Reference Saccaro, Schilliger, Dayer, Perroud and Piguet2021), which can partly explain the observational association between vitamin D deficiency and the risk of SI. Additionally, the non-linear association between vitamin D and baseline SI can be partly explained by a threshold effect of vitamin D on inflammation. A recent study reported that vitamin D exerted L-shaped effects on C-reactive protein (CRP) concentration (Zhou and Hypponen, Reference Zhou and Hypponen2023). The CRP level dropped down with increasing vitamin D concentration at low vitamin D concentrations and levelled off when the vitamin D concentration reached 50 nmol/L (Zhou and Hypponen, Reference Zhou and Hypponen2023). Furthermore, at 25(OH)D concentrations >30 ng/mL, the risk of baseline SI increased with an increase in vitamin D concentration. As this study involved a small sample size, the findings of the 25(OH)D sufficiency group should be further confirmed.
However, serum 25(OH)D was not significantly associated with any suicidality outcome in men. These results suggest a sex difference in the association between 25(OH)D and baseline SI. Similarly, a previous study reported that vitamin D concentration was inversely associated with mental health and psychosocial stress only among women (Chen et al., Reference Chen, Zhu, Harshfield, Treiber, Pollock, Pollock, Okereke, Su and Dong2020). A plausible explanation for the sex differences is sex-related hormones. In women, low vitamin D levels are associated with decreased estradiol levels (Zhao et al., Reference Zhao, Ouyang, de Boer, Lutsey, Farag, Guallar, Siscovick, Post, Kalyani, Billups and Michos2017). Estrogen downregulation can increase the risk of mood disturbances through the activation of neuroinflammation in the hippocampus (Xu et al., Reference Xu, Sheng, Bao, Wang, Lu and Ni2016) and the upregulation of serotonin neurotransmission (Hernandez-Hernandez et al., Reference Hernandez-Hernandez, Martinez-Mota, Herrera-Perez and Jimenez-Rubio2019). Sex differences in the association between vitamin D and suicidality warrant further investigation.
According to the Bradford Hill criteria, biological plausibility is not a specific criterion for causal inference (Fedak et al., Reference Fedak, Bernal, Capshaw and Gross2015). The presence or absence of biological plausibility did not influence the validity of traditional observational analysis, which is usually determined based on methodological considerations (Savitz, Reference Savitz2021). MR can overcome methodological limitations commonly occurred in traditional observational analysis, such as potential confounders and reverse causality. In this study, MR analysis did not reveal a linear or a non-linear association between genetically predicted 25(OH)D and the risk of suicidality, indicating that vitamin D did not exert causal effects on adolescent suicidality. Similar results were obtained in sex-stratified MR analysis. Revez et al. (Reference Revez, Lin, Qiao, Xue, Holtz, Zhu, Zeng, Wang, Sidorenko, Kemper, Vinkhuyzen, Frater, Eyles, Burne, Mitchell, Martin, Zhu, Visscher, Yang, Wray and McGrath2020) reported that 25(OH)D concentration did not exert causal effects on various neuropsychiatric traits, including schizophrenia, bipolar disorder, autism spectrum disorder and ADHD. Mulugeta et al. (Reference Mulugeta, Lumsden and Hypponen2020) demonstrated that a higher 25(OH)D concentration significantly decreased the risk of depression in observational analysis but genetically predicted 25(OH)D was not associated with depression in MR analysis. A possible explanation for these findings is that the significant association between vitamin D and suicidality observed in previous observational studies is driven by potential confounders and/or reverse causality. Individuals with SI may tend to avoid outdoor activities (leading to decreased sunlight exposure and consequently decreased endogenous vitamin D synthesis) and have a poor appetite with decreased dietary vitamin D intake. Moreover, previous bidirectional MR studies reported the causal effect of several psychiatric disorders on vitamin D (Mulugeta et al., Reference Mulugeta, Lumsden and Hypponen2020; Revez et al., Reference Revez, Lin, Qiao, Xue, Holtz, Zhu, Zeng, Wang, Sidorenko, Kemper, Vinkhuyzen, Frater, Eyles, Burne, Mitchell, Martin, Zhu, Visscher, Yang, Wray and McGrath2020). However, the possibility of type II error accounting for the null findings in this study cannot be excluded. Thus, a small-to-modest effect may not have been detected owing to the low statistical power. MR studies with a large sample size must be performed in the future.
The findings of this study have several implications for future studies. The non-linear cross-sectional association between vitamin D and SI was significant in women but not in men. This indicates that both non-linearity and sex differences need to be considered in future studies investigating the relationship between vitamin D and suicidality. Moreover, the application of the MR method in nutritional psychiatry is novel, which will aid in the identification of causal nutritional exposures in psychiatry. Future MR studies with large sample sizes should be conducted in this field. Additionally, MR analysis in this study revealed no evidence for the causal effect of vitamin D on suicidality. Thus, the observed association between vitamin D and suicidality in observational studies may be attributed to confounders and/or reverse causality. Accordingly, more attention should be paid to focusing on vitamin D as a potential indicator or a consequence than a causal risk factor for adolescent suicidality in future research examining the relationship between vitamin D and suicidality. Alternatively, the true causal effect of vitamin D on suicidality may be lower than that we had enough power to detect. Thus, further studies are needed with a large sample size.
Strengths and limitations
This study used data from a longitudinal cohort to investigate the relationship between vitamin D and suicidality in early adolescence. Both linear and non-linear effects were considered using flexible statistical methods to compensate for the limitation of statistical methods with linear hypotheses. Currently, the development of MR in the field of psychiatry is at a relatively early stage (Wootton et al., Reference Wootton, Jones and Sallis2022). MR-based psychiatry research has mainly focused on schizophrenia, major depression, autism spectrum disorders and bipolar disorder, with no studies on suicidality (Saccaro et al., Reference Saccaro, Gasparini and Rutigliano2022). The findings of this study, which examined the causal effect of vitamin D on suicidality using MR, will promote the application of MR in psychiatry, especially in suicidality research.
Several limitations should be considered when interpreting the findings of this study. Considering that the sample size was relatively small for MR analysis, the statistical power may have not been enough to rule out the possibility of vitamin D exerting a small-to-modest causal effect on suicidality. Further MR studies with a large sample size are needed to confirm the results of this study. Additionally, bidirectional MR analysis was not performed to examine the causal effect of suicidality on vitamin D due to the unavailability of genotype data on suicidality-related SNPs in this study. Future bidirectional MR studies are needed. Furthermore, the study participants were from one school, which limits the generalization of the results. Finally, this study evaluated suicidality outcomes based on self-reporting instead of clinical diagnosis, although the application of objective measures to the general population for research is not feasible.
Conclusions
In the Chinese early adolescent cohort, traditional observational analysis revealed a significant non-linear association between the 25(OH)D concentration and the risk of baseline SI in women. Moreover, the risk of baseline SI in the 25(OH)D deficiency group was higher than that in the 25(OH)D deficiency group in the total sample. This difference remained significant in women but not in men. However, both linear and non-linear MR methods did not support the causal effect of 25(OH)D on baseline and 1- or 2-year incident suicidality risk. The findings of this study improved our knowledge by indicating that the observed association between vitamin D and suicidality is likely to be driven by potential confounders and/or reverse causation. These findings should be confirmed in a large cohort with sufficient statistical power in the future.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796023000665.
Availability of data and materials
Data will be available upon reasonable request.
Acknowledgements
The authors would like to thank all the students for their participation and support, and the teacher’s assistance in data collection.
Author contributions
M. Yuan, G. Wang and P. Su conceived and designed the study. M. Yuan, Y. Li and J. Chang designed the statistical analysis plan. X. Zhang, S. Wang, L. Cao and Y. Li analysed the data and developed the figures and tables. M. Yuan, G. Wang and P. Su reviewed the findings and contributed to the interpretation. All authors contributed intellectual content during the drafting and revision of the work and approved the final version of the paper. GF. Wang and PY. Su contributed equally in this work. GF. Wang can also be contacted for correspondence wanggenfu@ahmu.edu.cn.
Financial support
This work was supported by the National Natural Science Foundation of China (G. Wang, grant number: 82204071) (P. Su, grant numbers: 81874268, 82173539).
Competing interests
None declared.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









