INTRODUCTION
Orthopedic injuries are common painful conditions,Reference Spady, Saunders and Schopflocher 1 comprising more than 10% of emergency department (ED) visits in children.Reference Chamberlain, Patel and Pollack 2 Fractures comprise approximately 10% to 25% of injuries in children.Reference Landin 3 The most severe pain following an orthopedic injury occurs within the first 48 hours following discharge, and over 80% of children experience compromise in at least one functional domain.Reference Drendel, Lyon and Bergholte 4 Limited comprehension of discharge instructions can be attributed to disparity between literacy levels and written discharge material.Reference Herndon, Chaney and Carden 5 In children with musculoskeletal injuries, little information is provided to caregivers on managing pain following discharge.Reference Maimon, Marques and Goldman 6 As a possible consequence, it has been reported that only 72% of parents provide pain relief after an injury, and only 28% use pharmacologic therapies.Reference Maimon, Marques and Goldman 6 In addition, almost a third of parents are reportedly dissatisfied with the pain relief that their child receives at home following ED care for a fracture.Reference Gill, Drendel and Weisman 7 There are challenges regarding the best way to disseminate information on the recognition and home management of pain in children. Indeed, ED clinicians are often constrained by the time that they can devote to comprehensive caregiver education. As a result, the content of discharge instructions is often highly variableReference De Maio, Joseph, Tibbo-Valeriote and Cabanas 8 , Reference Sarsfield, Morley, Callahan and Grant 9 and is poorly understood by most ED patients.Reference Engel, Heisler, Smith and Robinson 10 , Reference Engel, Buckley, Forth and McCarthy 11 Digital media approaches overcome literacy barriers and have shown benefit in caregiver knowledge acquisition in autism,Reference Kobak, Stone, Wallace and Warren 12 type I diabetes,Reference Boren, Gunlock, Peeples and Krishna 13 epilepsy,Reference Walker, Wexler, Dilorio and Escoffery 14 asthma,Reference Bussey-Smith and Rossen 15 and juvenile idiopathic arthritis.Reference Stinson, McGrath and Hodnett 16 In pediatric fractures, however, such interventions have not been explored. Almost 75% of North American households have Internet access,Reference File and Ryan 17 and up to 90% of parents access the Internet for health resources.Reference Park, Weiss and Repar 18 , Reference Bianco, Zucco, Nobile and Pileggi 19 Therefore, digital media may be a feasible and efficient way to disseminate information to caregivers in a busy ED. Given the frequency of pediatric fractures and the well-documented suboptimal management of children’s pain following ED discharge, we sought to assess caregiver knowledge acquisition and child functional outcomes for two novel digital media strategies (an interactive Web-based module [WBM] and a video) for children who sustained a nonoperative fracture. Demonstrating the effectiveness of these strategies in terms of knowledge improvement is an important initial step to inform their further development and utilization.
METHODS
Study design and setting
We conducted an open-label, parallel group, randomized, three-arm superiority trial to test the hypothesis that a novel educational video was superior to 1) a novel interactive WBM and 2) verbal instructions, the standard of care (SOC), with respect to caregiver knowledge acquisition in the ED on the recognition and management of fracture pain in children. We recruited participants from the pediatric ED of the Children’s Hospital, London Health Sciences Centre in London, Ontario from September 2015 to November 2016. Our institution is a tertiary care pediatric centre with an average annual census of 37,000 visits, including over 1,000 nonoperative fractures. The study received approval from Western University’s Health Sciences Research Ethics Board (www.clinicaltrials.gov NCT02435498).
Participants
We included the primary caregivers of all children ages 0 to 17 years who were diagnosed with a nonoperative fracture and were managed by the attending emergency physician. We excluded caregivers with a language barrier precluding comprehension of study-related tasks or lack of a home computer with Internet access; children with fractures requiring operative reduction, external fixation, or associated with multisystem trauma; children transferred from another facility; and children with a history of renal, liver disease, bleeding diathesis, chronic pain, or pregnancy.
A research assistant (RA) unaware of the study hypothesis assessed eligibility, obtained informed consent, and performed all correspondence with participants. Participants were recruited consecutively for 7 days a week between 1700 and 2200 hours, following the initial physician assessment.
Interventions
Participants were randomized using a 1:1:1 allocation, with a block size of four or six to receive pain management education with a WBM, video, or SOC based on a computer-based randomization sequence found at http://www.randomization.com. All interventions were administered in the ED, and participants in the WBM and video group were provided online access to their respective interventions for 120 hours following discharge. Allocation concealment was performed using sequentially numbered, opaque, sealed envelopes. We collected demographic information from all caregivers, including age, highest education level, employment status, relationship to the child, and history of fractures in their children.
Participants were administered in the ED, a novel 21-item knowledge questionnaire (Supplementary Appendix 1) on the recognition and management of post-fracture pain using SurveyMonkey. This was immediately followed by the intervention with the exception of the SOC, whose timing was variable, depending on the availability of the bedside nurse. An identical knowledge questionnaire was administered immediately following the intervention, in an effort to avoid cross-contamination between study groups, with participants potentially accessing additional sources of education.
At 120 hours post-discharge, participants were emailed a link to a five-item survey (Table 1) hosted on SurveyMonkey that assessed caregiver confidence in managing pain at home using a five-item Likert scale and functional outcomes. The question stems for the functional outcomes were modified from similar outcomes assessed by Drendel et al. in their study of children with upper extremity fractures.Reference Drendel, Gorelick and Weisman 20
Table 1 Responses to 5-day survey questions assessing functional outcomes
Tool development
The knowledge questionnaire was developed de novo using a focus group of four investigators (SGP, NP, SA, AD) and two ED nurses. It was pilot tested among another five pediatric ED physicians and five ED nurses. As a final step, the tool was pre-tested among 10 lay caregivers for content validity, face validity, comprehension, and readability. It was scored from zero to 21, with one point for each correct answer and no penalty for guessing.
The WBM was developed de novo using WordPress, which covered recognition of pain, over-the-counter analgesic dosing and indications; risks and safety in children; signs and symptoms of pain in children; and misconceptions about treating pain. Images used in the WBM were taken from two online sources of stock images.Reference Stockvault 21 , 22 Participants used their touchpad to click on the screen to activate the intervention’s interactive component that consisted of a dose calculator for analgesics.
The video was a 5-minute instructional clip, entitled Treating Pain at Home and hosted on the WordPress platform. It was developed de novo by pediatric investigators at the Medical College of Wisconsin for a previous studyReference Mueller, Summerill, Keyes and Drendel 23 using a focus group of pediatric providers. It was informed by qualitative interviews of caregivers that identified frequently asked questions about outpatient pediatric pain and its management. The video was recorded using a Betacam video recorder, and its utility was evaluated in a pediatric ED population.Reference Mueller, Summerill, Keyes and Drendel 23 Both the WBM and video contained identical factual content that was presented differently. Both the WBM and video can be accessed at www.fracturepain.com (password: londonpain).
The SOC included verbal instructions provided by the bedside nurse on dosing and frequency of over-the-counter analgesics and when to return to the ED. Although the content of the SOC was outlined by the nursing directive at our centre, it was not standardized in order to optimally reflect the SOC in most EDs, including our own.Reference Saidinejad and Zorc 24 The bedside nurse and physician were asked not to provide discharge teaching to participants in the WBM and video groups, and therefore they did not receive the SOC. All participants received a paper-based handout outlining how to care for the cast or splint and when to return to the ED (Supplementary Appendix 2). Questions about care following discharge were answered by the treating physician. At discharge, participants in the WBM and video groups were provided with a unique username and password to access their respective interventions following discharge. If participants did not access the intervention within 24 hours, they received a phone call from the RA confirming that they could access the site. The number of times that the WBM or video was accessed and the duration of access were recorded using custom website programming (Sublime Text). To minimize the risk of unaccounted co-interventions, participants in the WBM and video groups were asked to refrain from seeking out other educational materials.
Statistical analysis and outcomes
The per protocol analysis included participants who completed both the pre-intervention and post-intervention knowledge questionnaires. The primary outcome was the pre-intervention to post-intervention difference (gain score) on the 21-item knowledge questionnaire in the ED and was analysed using the analysis of variance (ANOVA). Pairwise differences were explored using a Tukey adjustment for multiple comparisons. Secondary outcomes were analysed using the Kruskal-Wallis test and included caregiver confidence in recognizing pain and providing analgesia, the number of sleep-interrupted nights for both the caregiver and child, the number of days of work or school missed for the caregiver or child, respectively, and the number of days before resumption of a normal diet for the child. For each secondary outcome, we performed ordinal logistic regression models to examine the effect of the duration of the time that participants accessed the WBM and video post-discharge. To examine whether the participant’s decision to access the intervention post-discharge influenced group differences in functional outcomes, we performed a sensitivity analysis in which Kruskal-Wallis tests were rerun for each functional outcome after removing participants in the WBM (n=2) and video (n=2) groups who did not access the respective interventions post-discharge. A between-group difference of 10% (two points) on the gain score was chosen as a minimal clinically important difference (MCID), based on a study of a video to educate caregivers about proper antibiotic use.Reference Schnellinger, Finkelstein, Thygeson and Vander Velden 25 Assuming a standard deviation (SD) of 20% from a previous study of an interactive Web-based intervention,Reference Hart, Nedadur, Reardon and Sirizzotti 26 86 participants per group were required to detect a 10% difference between all three groups at the 5% two-sided level of significance with 90% power. The sample size was increased by 10% per group to account for dropouts. Data were entered into a study-specific Excel spreadsheet and analysed using SPSS (version 24, IBM SPSS, Armonk, New York), and p values of less than 0.05 were used to reject the null hypothesis of no difference between groups.
RESULTS
Participants
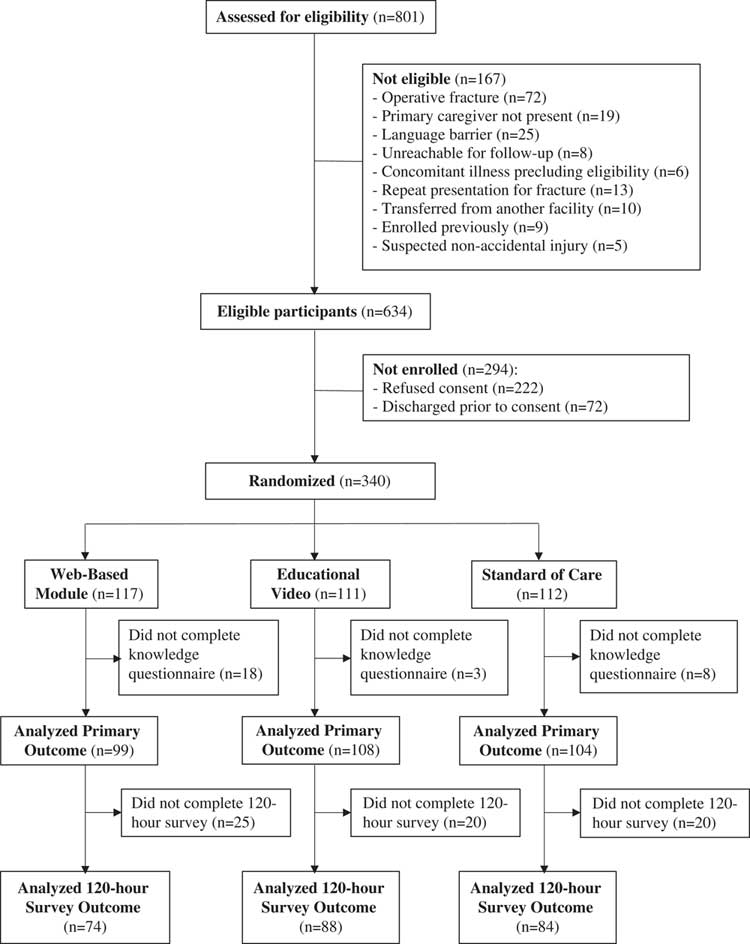
All 340 randomized participants completed each intervention. However, 29 did not complete the knowledge questionnaire. We analysed the results of the remaining 99 and 108 and 104 participants in the WBM, video, and SOC groups, respectively (Figure 1). The overall mean (SD) age of participants was 9.6 (4.2) years, of which 125/311 (40.2%) were female (Table 2). Sixty-five participants did not complete the 120-hour survey.
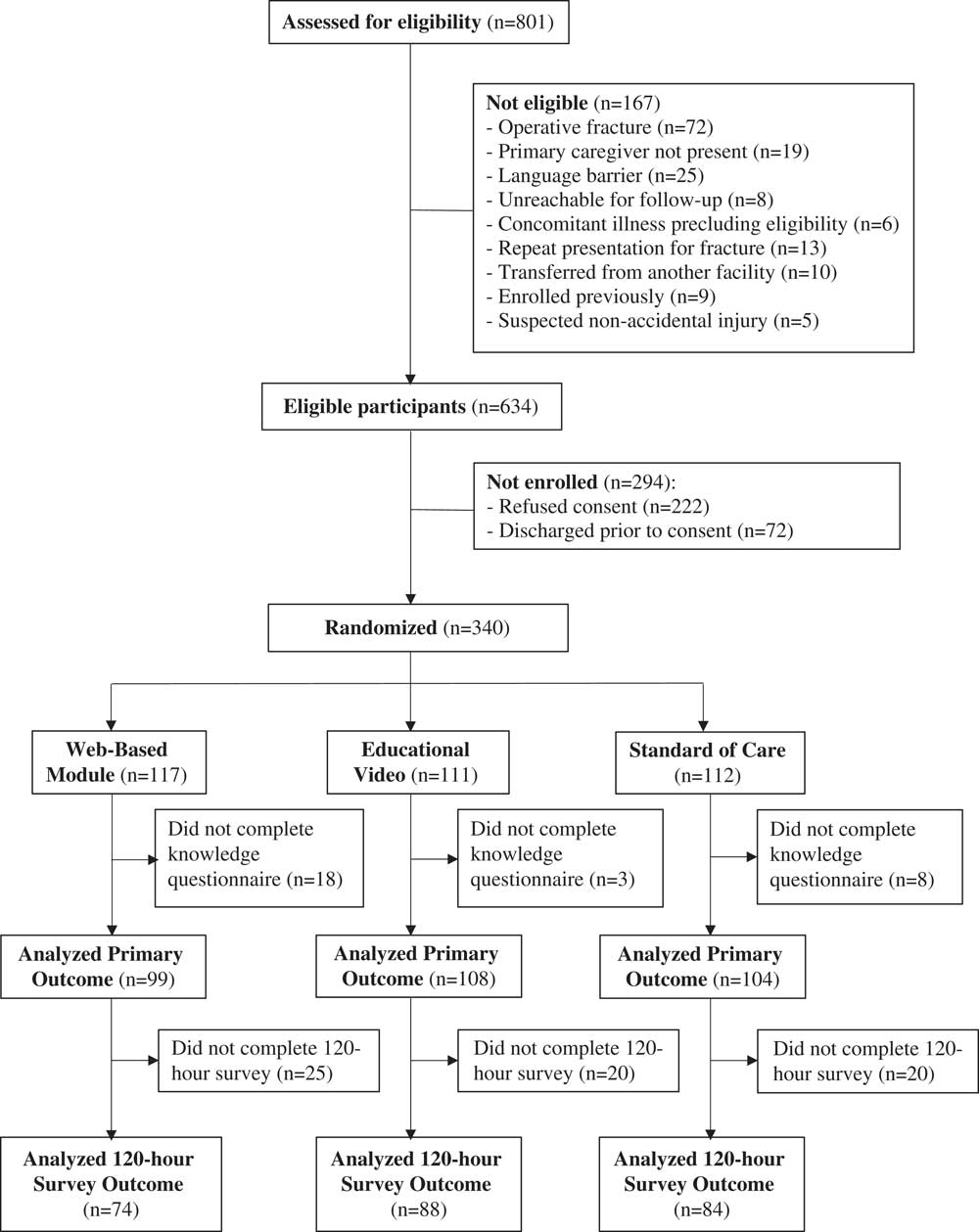
Figure 1 Flow of participants through the trial.
Table 2 Demographic characteristics of participants
SD=standard deviation.
* Percentage of total in column.
Primary outcome
There was an increase in knowledge questionnaire scores from pre- to post-intervention (gain score) in all three groups. The greatest increase was seen in the video followed by the WBM and SOC groups (Table 3). There were significant overall between-group differences (delta) in mean gain score (p<0.001). Participants in the video (delta=2.3, 95% confidence interval [CI]: 1.3, 3.3; p<0.001) and WBM (delta=1.6; 95% CI: 0.5, 2.6; p=0.002) groups had significantly greater gain scores than the SOC group. The mean gain score in the video group was not significantly greater than that of the WBM group (delta=0.7; 95% CI: -0.3, 1.8; p=0.25) (see Table 3). The duration of time that the interventions were accessed in the ED ranged from 8 to 15 minutes for the WBM and 5 minutes to load and view the video. In the WBM and video groups, 86 and 72 participants, respectively, accessed the interventions following discharge from the ED. In the covariate analysis, the mean gain score was not significantly different between WBM and video groups (delta=−0.3; 95% CI: −1.4, 0.8; p = 0.54).
Table 3 Mean (SD) knowledge and gain scores (maximum score of 21)
N/A=not applicable; SD=standard deviation.
* Difference between pre-test and post-test score. Value was obtained by subtracting the pre-test from the post-test score for each participant then calculating the mean.
Secondary outcomes
Greater than 60% of caregivers reported being very confident in their ability to manage their child’s pain at home (Table 1). Roughly, half of caregivers reported that their child missed at least some school, and more than half reported difficulty sleeping presumably due to pain. Twenty-seven percent to 45% of caregivers reported some impact on their child’s diet, and 41% to 44% reported missing work to take care of their child. There were no overall between-group differences in functional outcomes (see Table 1) even after removal of participants who did not access the WBM and video post-discharge (caregiver confidence, p=0.41; school absence, p=0.39; sleep, p=0.85; diet, p=0.1; work absence, p=0.98). There was no significant effect of duration that the WBM and video were accessed and overall group differences in caregiver confidence (p=0.54), school absence (p=0.2), sleep (p=0.65), diet (p=0.2), and work absence (p=0.57).
Participants lost to follow-up
Demographic and outcome-specific details of participants who did not complete study procedures can be found in Table 4. Overall, there were no differences in demographic features between participants who did and did not complete the study.
Table 4 Characteristics of participants who did not complete study procedures
N/A=not applicable; SD=standard deviation.
* Percentage of total in column.
† Difference between pre-test and post-test score. Value was obtained by subtracting the pre-test from the post-test score for each participant then calculating the mean.
DISCUSSION
This randomized, open-label trial of the effectiveness of digital media educational interventions among caregivers whose children sustained nonoperative fractures demonstrated that an interactive WBM and video provided superior knowledge acquisition to SOC verbal instructions. Furthermore, functional impairments across the entire sample were prevalent. Our findings suggest that digital media may provide an effective, standardized way to deliver discharge education in the busy ED environment.
Both the WBM and video were associated with a significantly greater gain score compared to the SOC by a margin that exceeded our MCID at the upper bound of the CI but not the lower bound. This suggests that, while our results were statistically significant, they may not be clinically significant if one considers the most conservative estimate of the between-group differences. However, our results parallel a growing body of literature in which multimedia technology has shown benefit when delivering discharge instructions in the ED. In previous work by our group, an interactive WBM and read-only website were associated with significantly greater knowledge acquisition than written and verbal information among caregivers of children with fever.Reference Hart, Nedadur, Reardon and Sirizzotti 26 Although it did not reach statistical significance, it was not surprising that the greatest gain score was associated with the video, because literacy has often been cited as a barrier to the comprehension of discharge instructions.Reference Lukoschek, Fazarri and Marantz 27 Atzema et al. found that online videos led to significantly greater understanding of diagnoses and care among adult ED patients for a wide range of diagnoses, including fractures.Reference Atzema, Austin, Wu and Brzozowski 28 Video discharge instructions in the ED have been associated with significantly greater knowledge acquisition in caregivers of children with gastroenteritis,Reference Wood, Harrison, Trickey and Friesen 29 bronchiolitis,Reference Wood, Harrison, Trickey and Friesen 29 fever,Reference Wood, Harrison, Trickey and Friesen 29 , Reference Ismail, McIntosh, Kalynych and Joseph 30 head injury,Reference Ismail, McIntosh, Kalynych and Joseph 30 and antibiotic use.Reference Schnellinger, Finkelstein, Thygeson and Vander Velden 25 In terms of knowledge retention, Bloch et al. found that video discharge instructions provided to caregivers of children with wheezing, fever, vomiting, or diarrhea improved knowledge up to 5 days post-discharge.Reference Bloch and Bloch 31
In our study, participants across all three groups had a correct response rate of just over 60% on the pre-intervention knowledge questionnaire. This underscores the need for caregiver education on pain management and is consistent with ample evidence that caregiversReference Abou-Karam, Dube and Kvann 32 and patientsReference Engel, Heisler, Smith and Robinson 10 , Reference Engel, Buckley, Forth and McCarthy 11 , Reference Makaryus and Friedman 33 , Reference Hwang, Trickey, Lormel and Bradford 34 often lack a complete understanding of discharge instructions. Despite a relative lack of baseline knowledge, gain scores across groups were modest. Even the most effective intervention, the online video, exhibited only a 12% increase in knowledge score. This suggests either a need for more effective educational strategies or, more likely, ensuring that families receive discharge education, an environment that is more conducive to knowledge retention than a busy ED. To ensure that study participants did not leave the ED prior to their completion of the second knowledge questionnaire, the interventions were administered during the ED visit rather than at discharge. However, the noise level, distractions, and associated stressors in the acute care setting may have been a barrier to optimal information processing and knowledge retention.Reference Saidinejad and Zorc 24 Although the home environment, together with repeated viewing of the Web-based interventions, may have led to greater knowledge acquisition, we did not measure knowledge acquisition post-discharge. Instead, we focused on functional outcomes because we believed them to be more salient to the clinical application of our findings.
The success of educational interventions is ultimately predicated upon an improvement in functional outcomes. Our study was not powered to detect between-group differences in functional outcomes. Although the absence of benefit may have been due to lack of statistical power, another possibility is that our 5-day survey may not have been sufficiently sensitive to change. Nevertheless, a large proportion of children experienced deficits in school attendance, sleep, and diet, consistent with the findings of Drendel et al. in their two studies of post-discharge fracture pain in children.Reference Drendel, Gorelick and Weisman 20 , Reference Drendel, Brousseau and Gorelick 35
The practicality of digital media educational interventions for caregiver education lies in their accessibility, consistency of information, and the ability to easily incorporate new information. Digital media can also be self-administered, making them less resource intensive than verbal discharge instructions. Caregivers and children are reportedly motivated to use Web-based resources, trust the information provided, and use interactive features to manage pain at home.Reference Stinson, McGrath and Hodnett 16 Additionally, websites from a physician or medical association appear to be most often accessed, suggesting that caregivers have a preference for information from health care professionals.Reference Bianco, Zucco, Nobile and Pileggi 19 Our study has established that digital media educational interventions improve caregiver knowledge. However, to definitively establish their clinical utility and support their cost-effectiveness, future studies should be powered to detect clinically important improvements in a wide range of functional outcomes.
LIMITATIONS
Our sample included caregivers who were highly educated, proficient English speakers. Therefore, our findings may have limited generalizability to a non-English speaking population. We chose not to standardize the SOC intervention, and the knowledge questionnaire likely contained items that were not addressed by the SOC. Although this may have inflated the effect size, we feel that this approach was a more accurate comparison between the Web-based interventions and the discharge teaching that a family actually receives in contrast to what they would ideally receive if the SOC were standardized. Furthermore, unlike the WBM and video groups, participants in the SOC were not asked to avoid seeking out other educational materials. A validated scale was not used to measure functional outcomes leading to the possibility of measurement bias. Although such scales exist, items were either not applicableReference Plint, Gaboury and Owen 36 , Reference Msall, Diguardio, Duffy and LaForest 37 or the scale was developed in a post-surgical population.Reference Ewing-Cobbs, Bloom, Prasad and Waugh 38
CONCLUSIONS
We have demonstrated that a WBM and video are associated with greater caregiver knowledge acquisition over SOC verbal instructions with respect to managing children’s pain following a fracture. Although the differences may not be clinically significant, these interventions may provide standardized and efficient caregiver education, and our findings are an important initial step in their further development. However, a large proportion of children experienced deficits in school, sleep, and diet, and there was no evidence of benefit to the digital media interventions. Further study is needed to determine the best approaches to reducing functional limitations due to pain following non-operative fractures in children.
Acknowledgements: We would like to acknowledge Keri Hainsworth, PhD; Steven J. Weisman, MD; Dana Mueller, MD; Shaun Summerill, MD; Jill Keyes, MD, MS RN; Jeff Surges; and Brian Herteen for their role in the development and production of the video intervention. Prior presentations include Canadian Paediatric Society, June 2017, Vancouver, BC. This study was funded through a resident research grant by the Department of Paediatrics, Western University.
Competing interests: None declared.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2017.414