CLINICAL SCENARIO
A 60-year-old female presents to the emergency department (ED) with a 3-day history of fatigue and mild breathlessness. She has a history of lung cancer. Her vitals indicate shock with a heart rate of 140 bpm, a systolic blood pressure (SBP) of 65 mmHg, a respiratory rate of 28, with an oxygen saturation of 90% on 100% a nonrebreather mask, and a normal temperature at 36°C. Her electrocardiograph (ECG) shows sinus tachycardia. She appears mottled and pale.
KEY CLINICAL QUESTIONS
- 1.
How should I use focused cardiac point of care ultrasonography (PoCUS) in shock?
Several algorithms or protocols have been proposed to organize how to perform sonography in hypotension and cardiac arrest (SHoC) including “RUSH” and “ACES” among others.Reference Atkinson, Bowra, Lambert, Lamprecht, Noble and Jarman1 Whichever you follow, it can be useful to think of the Five F's as an approach to PoCUS in shocked patients (see Figure 1). Look for Fluid (Is there a large pericardial effusion or pleural effusion?); Form (Is the heart enlarged or small? What is the right to left ventricular ratio? Are the valves thin or thickened?); Function (Is the myocardium thickening? Are both ventricles contracting? Are the valves opening fully? In other words, is the pump functioning effectively?); Flow (Is there unidirectional flow across the valves as seen on color flow doppler? Is there adequate cardiac output?); Filling (What is the inferior vena cava [IVC] size and respiratory variation? Are there multiple B lines in both lung fields?). The goal being to identify a physiologic diagnosis to guide resuscitation while a work up for the precise etiology is underway.
- 2.
Are there any cautions or contra-indications for using PoCUS in shock states?
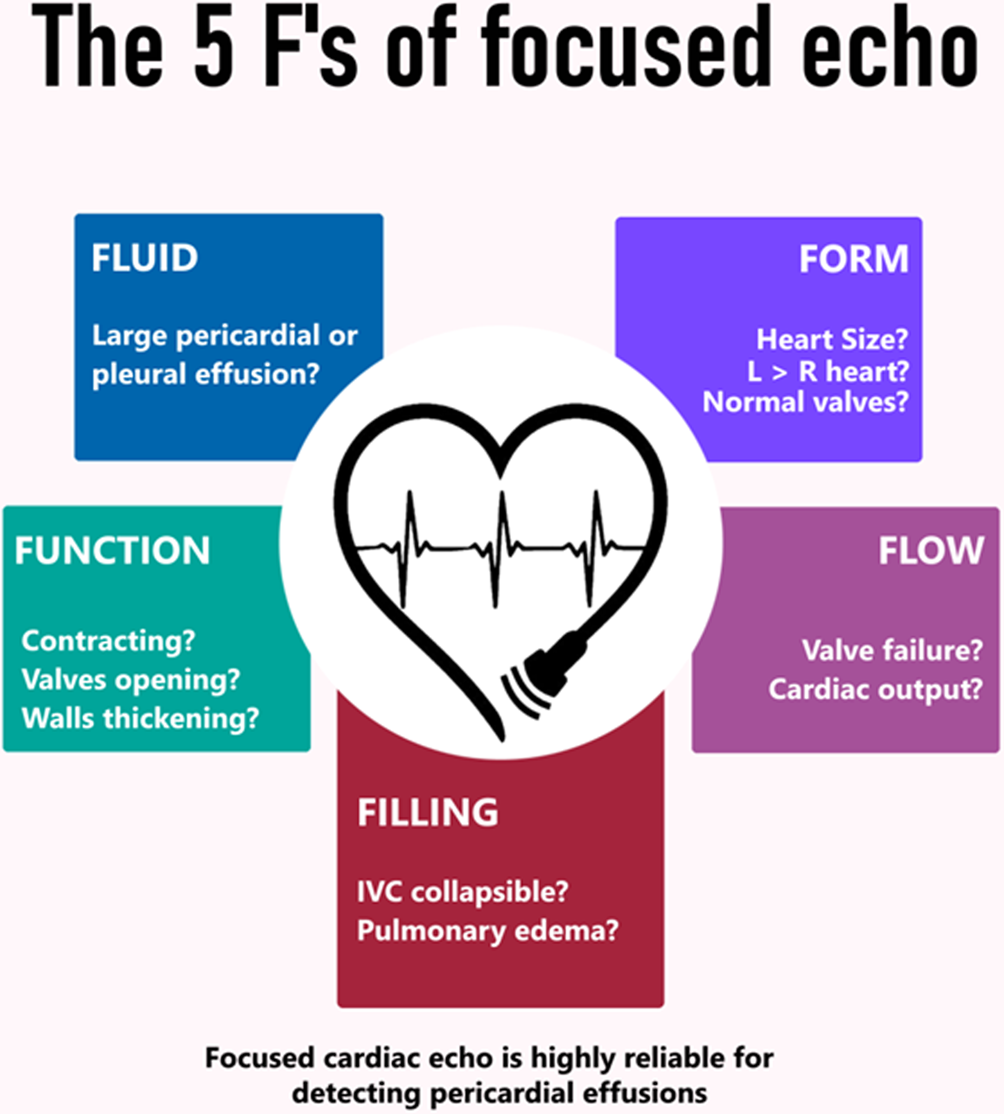
Figure 1. The Five-F's approach to focused cardiac echo in a hypotensive or arrested patient.
It is essential that PoCUS not delay or distract from key interventions. In the cardiac arrest setting, there is evidence that the use of PoCUS can lead to increased “off chest” pauses in cardiopulmonary resuscitation (CPR).Reference Huis in't Veld, Allison and Bostick2 Although there is no strong evidence that PoCUS provides any survival benefit in shock,Reference Atkinson, Milne and Diegelmann3 certain reversible causes of cardiac arrest or shock are extremely difficult to diagnose rapidly without PoCUS. This includes pericardial effusions, massive volumes of pleural or peritoneal fluid, abdominal aortic aneurysms, and distinguishing low flow states from true arrest, among others. Therefore, it is advisable to look for reversible causes in a rapid focused manner (the Five F's), while ensuring that chest compressions and other evidence-based interventions are not delayed.
- 3.
How accurate is PoCUS in identifying the underlying diagnosis?
Focused cardiac PoCUS is highly reliable in detecting or excluding pericardial fluid. It has also been shown to reduce the number of potential diagnostic etiologies in nontraumatic shock patients.
Pooled positive likelihood ratios for determining the underlying cause of shock vary from 8.3 in hypovolemia to 40.5 in obstructive shock, making it a good diagnostic tool in the right circumstances. Negative likelihood ratio values ranged from 0.13 to 0.32 in the same study.Reference Stickles, Carpenter and Gekle4
There is a need for a comparative study of PoCUS-based diagnosis v. standard care to assess the potential impact on diagnostic accuracy. Do not rely on PoCUS to rule out pathology, such as pulmonary embolism, and do not overcall this diagnosis in the cardiac arrest or peri arrest setting based on right ventricular size alone.
You are on your way to grab the ultrasound machine to complete your focused five F's exam when a code blue is called – it is your patient. CPR is ongoing.
- 4.
Can PoCUS help with interventions during resuscitation of the critically ill patient?
In addition to diagnostic benefit, there are multiple ways in which PoCUS can help in the management of critically ill patients. This includes confirmation of endotracheal intubation and bilateral lung ventilation; improved success and reduction in complication rates by use in guidance for vascular access, pericardiocentesis, or thoracentesis. The use of PoCUS during cardiac arrest has been shown to increase rates of intervention and prolong resuscitation efforts. (For more information, see Atkinson et al.Reference Atkinson, Bowra, Harris, Jarman and Lewis5) However, pioneer work is being done by emergency physicians in the country to incorporate transesophageal echocardiography into resuscitation protocols, which could potentially alleviate these issues.
- 5.
Other than the heart, what should I scan during cardiac arrest or shock?
The approach to scanning will depend on the clinical setting, including the stability of the patient. In most situations, it is advisable to begin by scanning the heart to assess for the Five F's, followed by consideration of lung and IVC scans. Additional questions can be addressed by scanning other systems and areas, depending on the clinical question and a priori risk for common etiologies. For example, scanning the abdominal aorta is important in an older male with hypotension. In a young female, focusing on the abdomen and pelvis for free fluid and assessment of the uterus is more appropriate. In a breathless patient with a history of cancer, scanning for evidence of DVT. The SHoC protocol outlines this Bayesian approach to prioritizing scanning in critical illness.Reference Atkinson, Bowra, Lambert, Lamprecht, Noble and Jarman1
CASE RESOLUTION
You start with a focused cardiac scan during a rhythm check, which reveals a large pericardial effusion (see online Appendix Figure 1). A combined sonographic and clinical diagnosis of cardiac tamponade is made. PoCUS is then used to guide pericardiocentesis in the left parasternal area. Removal of 40 mL of fluid leads to return of spontaneous circulation (ROSC) and further care under the cardiology team (see online Appendix Video 1).
KEY POINTS
For unstable patients, use the Five-F's approach for focused cardiac PoCUS.
• Fluid: Look for significant pericardial and pleural fluid.
• Form (shape): Look at right and left chamber sizes and ratios.
• Function: Is the pump working? Are the walls thickening, chambers contracting, and valves opening?
• Flow: Add color Doppler to check the direction of blood flow.
• Filling: Check IVC size and collapse for right sided filling, check lungs for B lines and signs of pulmonary vascular overload.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.440.





