INTRODUCTION
North American emergency medical services (EMS) attend to 134 cases of out-of-hospital cardiac arrest (OHCA) per 100,000 adult citizens annually,Reference Nichol, Thomas and Callaway 1 , Reference Go, Mozaffarian and Roger 2 with survival ranging from 3%-16%.Reference Nichol, Thomas and Callaway 1 , Reference Go, Mozaffarian and Roger 2 Emerging data have suggested that extracorporeal cardiopulmonary resuscitation (ECPR), a form of veno-arterial extracorporeal membrane oxygenation (ECMO) implanted during cardiac arrest, may improve survival in certain patients with refractory OHCA.Reference Morimura, Sakamoto and Nagao 3 - Reference Stub, Bernard and Pellegrino 6
Several centres have described ECPR experiences; although inclusion criteria—chiefly, younger patients with both rapid arrest recognition and initiation of cardiopulmonary resuscitation (CPR)—have been similar, outcomes have varied.Reference Wang, Chou and Becker 4 - Reference Kim, Jung and Park 12 Positive outcomes appear to be strongly correlated with the time from arrest-to-ECPR initiation: survival is rare if this number exceeds 75 minutes.Reference Wang, Chou and Becker 4 , Reference Leick, Liebetrau and Szardien 5 , Reference Haneya, Philipp and Diez 7 - Reference Kim, Jung and Park 12 In ECPR studies comparing in-hospital arrests with OHCAs, patients in the latter group—despite often demonstrating better prognostic characteristics such as a younger age and higher proportion of shockable rhythms—demonstrate significantly worse outcomes than their hospitalized counterparts,Reference Haneya, Philipp and Diez 7 , Reference Avalli, Maggioni and Formica 8 likely in part because of the substantial increase in the time to ECPR initiation.
While the community is the most likely place for a sudden unexpected cardiac arrest in a previously healthy patient, the ideal ECPR candidate, there are logistical challenges in optimizing arrest-to-ECPR intervals for out-of-hospital patients with refractory arrest. At our institution, we recognized that in the small number of OHCAs that were treated with ECPR, the times required to initiate ECMO were prolonged. Further, as our prehospital system prioritizes on-scene resuscitation, with patients in refractory arrest uncommonly transported to the hospital, few could be considered for this therapy. For this reason, we developed a formal regional clinical ECPR protocol for OHCAs, the first of its kind in Canada, to improve the access and efficiency of ECPR initiation. The protocol included prehospital and hospital integration for early identification and transport of ECPR candidates, with rapid ECPR initiation upon hospital arrival for those who remained in refractory arrest. To achieve this, we instituted an intensive educational and quality improvement program, involving all members of the ECPR initiation team from each phase of care, to optimize time metrics. The primary goal of the ECPR service was to achieve expedited initiation of ECPR for appropriate patients; the aim of this study was to measure the change in times to ECPR initiation after protocol implementation.
METHODS
Study design and setting
This study was an observational before-and-after design examining the performance of a clinical protocol, which took place in a single health region including the cities of Vancouver and North Vancouver and the district municipalities of North Vancouver and West Vancouver, in the province of British Columbia (BC). The total land area is approximately 380 km2 and contains a population of approximately 800,000 (73% between the ages of 15 and 65) 13 and four emergency departments (ED). The study hospital is St Paul’s Hospital, a regional cardiac referral centre, which includes 24-hour access to cardiothoracic surgical services and cardiac catheterization, as well as cardiac transplant and ventricular assist device programs. The cardiovascular surgery program has provided ECPR services at St. Paul’s Hospital since 2000 on a case-by-case basis, but with no formal protocol prior to the protocol described in this manuscript.Reference Lamarche, Chow and Bédard 14 The ED treats approximately 85,000 patients annually.
This study protocol was submitted to and reviewed by the University of British Columbia (UBC)/Providence Healthcare Research Ethics Board but was deemed exempt from the requirements for researcher ethics approval both in accordance with UBC Policy and the provisions of the Tri-Council Policy because it was a classified as a quality improvement project.
Prehospital care
In BC, coordinated EMS is provided by municipal fire departments (FD) and the provincial Ambulance Service (BCAS). FD first responders are trained in basic life support (BLS)Reference Kleinman, Brennan and Goldberger 15 including automated external defibrillators (AED). There are approximately 20 BLSReference Kleinman, Brennan and Goldberger 15 paramedic teams and four advanced life support (ALS)Reference Grunau, Reynolds and Scheuermeyer 17 paramedic teams on-duty at any given time; the latter attend to approximately 98% of OHCAs. 18 BCAS policy requires that all patients treated by EMS must undergo resuscitative efforts for at least 30 minutes prior to termination unless contrary to family wishes or a “do not resuscitate” order is identified.Reference Grunau, Scheuermeyer and Stub 19 Transport of patients who do not regain a pulse (ROSC) in the prehospital setting is rare. 18
Development of hospital-based care protocols
In January 2014, discussions commenced regarding the establishment of a regional ECPR service for OHCA based at St. Paul’s Hospital. It was acknowledged that ECPR services were already being utilized for OHCA, but quite infrequently and on an ad hoc basis, that there was no established eligibility criterion and that ECMO initiation times were prolonged. A committee was created involving administrative and clinical representatives from the health authority’s senior leadership team, emergency medicine, cardiac surgery, perfusion services, cardiac anesthesiology, interventional cardiology, and critical care. The feasibility, potential benefits, resource utilization, and costs of such a formal program for OHCA ECPR application were discussed, and analyses were developed and published.Reference Grunau, Reynolds and Scheuermeyer 20 , Reference Kern, Thomas and Hughes 21 The committee endorsed the proposal, which was approved by the hospital administration in June 2015. Over the next six months, a formal OHCA ECPR hospital-based protocol was developed that commenced in January 2016. The stated overall vision was to improve the proportion of neurologically intact survivors among young previously healthy victims of sudden unexpected OHCA, through rapid identification of appropriate candidates and initiation of ECPR in the ED for a short duration of intensive therapy. The key goal metric of the protocol was time-to-ECMO (TTE) flows within 75 minutes, but preferably within 60 minutes, of initial professional resuscitative efforts. The inclusion and exclusion criterion are described in Figure 1. All required equipment and materials for ECPR initiation, including an ECMO unit, were acquired and housed in the ED resuscitation bay.
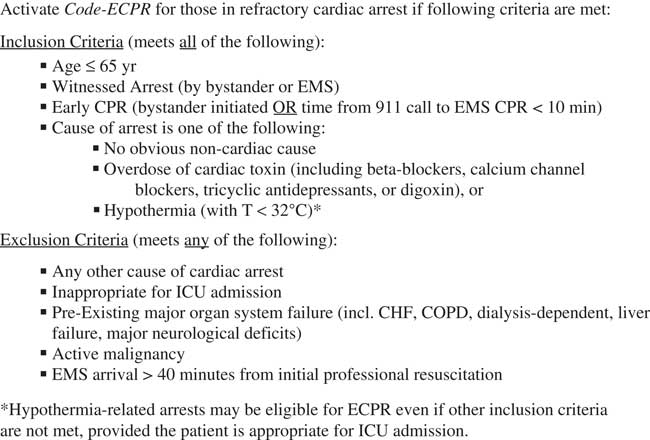
Figure 1 ECPR Criteria.
Development of novel prehospital ECPR protocol
In June 2015, discussions began with the senior leadership at BCAS. As arrests typically run for 30 minutes without transport to the hospital for those who did not achieve ROSC,Reference Grunau, Scheuermeyer and Stub 19 , Reference Kern, Thomas and Hughes 21 this new protocol required a major change. The prehospital phase of the protocol was developed, along with a training program for paramedics in the region, and was based on a six-step Kern approach.Reference Langley, Nolan, Nolan and Norman 22 One Lucas mechanical chest compression device (Physio-Control, Inc., Lund, Sweden) was acquired for each ALS team. The training package was sent to all paramedics: 1) a manual outlining the ECPR protocol; 2) a manual describing the operation of the Lucas device; 3) video instructions for the Lucas device; and 4) hypothetical case examples of potential ECPR patients. In addition, all ALS paramedics underwent: 1) standardized in-person training of the protocol and operation of the Lucas chest compression device; and 2) a test to confirm competency. A Lucas-compatible mannequin was placed in each ALS station for interval training. Pocket cards detailing the inclusion and exclusion criteria, as well as the prehospital portion of the protocol, were given to each paramedic.
The protocol is shown in Figure 2. For all patients meeting the criteria, the ALS paramedic called the on-duty St. Paul’s emergency physician (EP). The criteria were reviewed, and if candidacy was confirmed, the EP activated “code-ECPR.” Paramedics intubated the patient (if not already performed), applied the Lucas compression device, extricated, and then transported the patient to St. Paul’s Hospital with ongoing ACLS resuscitation.
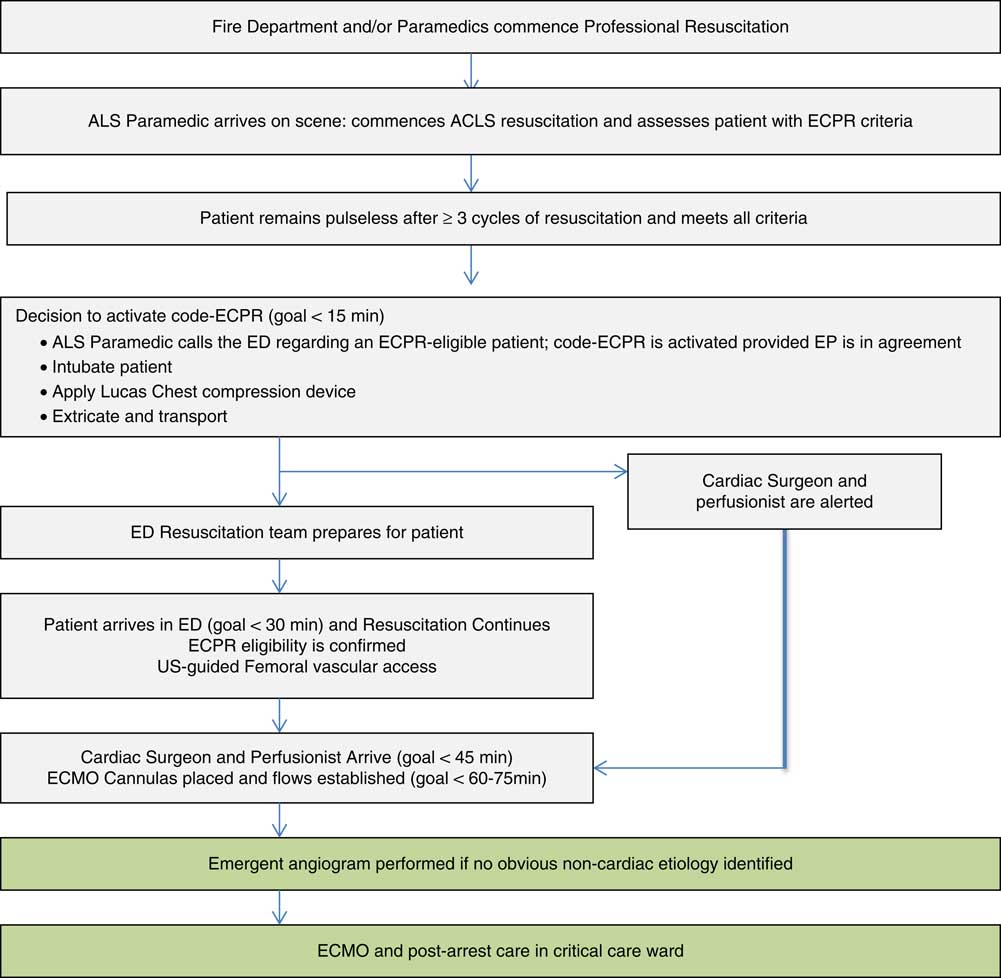
Figure 2 ECPR Protocol Scheme.
ED and hospital-based protocol
Upon receiving a call from an ALS paramedic, the EP completed a standardized form to ensure the patient was appropriately included; if so, the EP initiated “code-ECPR.” The ED unit clerk notified the on-call cardiovascular surgeon and perfusionist (in-hospital from 6:00 a.m. to 6:00 p.m., and within 30 minutes of the hospital at other times), as well as cardiac anesthesiology, intensive care, the cardiac surgery intensive care unit (ICU) nurse leader, and the hospital clinical coordinator. The ED team, consisting of two EPs, four nurses, and one respiratory therapist, assembled in the resuscitation bay prior to patient arrival, and various duties were assigned (Online Appendix 1). Upon patient arrival, the patient was again assessed using the eligibility criteria. One EP began placing single-bore 16-gauge catheters in the artery and vein using US guidance. In addition, a bedside US was performed to assess for reversible OHCA causes. Upon arrival, the cardiovascular surgeon assumed leadership of cannulation, inserting the ECMO cannulas with the EPs assisting and using a bedside US to assist with wire placement. ECMO flows were then commenced. Unless an obvious noncardiac cause was identified, an emergent coronary angiogram was performed. Online Appendix 2 details the strategy for ongoing ECMO management. All patients for whom withdrawal of life-sustaining therapies was planned were considered for donation.
Medical and nursing education
Beginning in June 2015, we organized monthly stakeholder meetings to create a curriculum that was open to feedback and continuous iterative improvements. We sent monthly electronic messages to all ED staff regarding the protocol and invited contributions. At monthly departmental and educational rounds, various committee members gave ten-minute sessions relating to various protocol aspects.
We organized ECPR simulations involving prehospital and ED providers monthly since October 2015 and included ALS prehospital notification, code-ECPR activation, ED preparation and delegation of roles, paramedic arrival (with a mannequin on an EMS stretcher and ongoing mechanical chest compressions) and transfer of care, ED ACLS resuscitation, and US visualization of femoral vessels with US-guided catheterization. New medical supplies were used in each simulation to enhance verisimilitude. We used an adapted mannequin with a custom-made ballistic gel over a tubing insert to cannulate and place ECMO cannulas. At the conclusion of each session, a debriefing session was held, and the simulation director and program leaders provided feedback. Simulations were recorded for further analysis.
Quality improvement model
The Model for Improvement Framework of Deming’s System of Profound Knowledge was utilized to achieve and sustain the primary outcome.Reference Jacobs, Nadkarni and Bahr 23 Real-time data were measured using run charts, with additional analysis to examine any particular cause variation noted. Reference Jacobs, Nadkarni and Bahr 23 We attempted to interview all participants after the ECPR activations, including all involved physicians and surgeons, nurses, perfusionists, and respiratory therapists.
Report cards
A designated quality and safety team was constructed to perform a standardized, detailed review of all “code-ECPR” activations that included interviews of participants, a synopsis of the event, calculation of time intervals, areas of success, and areas for improvement. We assembled template report cards (see Online Appendix 3) and sent them to all stakeholders and all ED staff members.
Selection of participants and analysis groups
This study included consecutive patients with nontraumatic refractory OHCA who had ECPR initiation attempted in the ED. Patients were excluded if sustained ROSC was achieved prior to ECPR initiation attempt.Reference Perkins, Jacobs and Nadkarni 24 We dichotomized patients based on whether they were treated prior to or after protocol implementation. We included patients who were treated up to two years prior to and within the first seven months of the commencement of the ECPR protocol.
Outcome measures and variable definitions
The primary outcome was the TTE, defined as the time of first professional resuscitative efforts to the commencement of ECMO flows. All cases were included in the analysis, regardless of whether adequate ECMO flows were achieved. In addition, we described the outcomes of the ECPR-treated patients at hospital discharge: 1) favourable neurologic outcomes defined as a cerebral performance category 1–2; and 2) survival.Reference Morrison, Nichol and Rea 25
Data collection
All prehospital data including commencement of first EMS CPR, patient characteristics, Utstein variables,Reference Morrison, Nichol and Rea 25 and treatments were recorded on standardized BCAS template charting (in use since prior to the pre-protocol period). Perfusion services have used a standard template form for all ECMO initiations since before the pre-protocol time period; this template includes data entry for the time ECMO flows were first initiated. We collected data from these sources onto a standardized Excel spreadsheet, which was used to populate the ECPR report cards (Online Appendix 3). The overall number of OHCAs in the region was determined using the BC Resuscitation Outcomes Consortium OHCA Registry.Reference Rubertsson, Lindgren and Smekal 26
Data analysis
We used Microsoft Excel 2008 (Microsoft Corp, Redmond, WA, USA) and R version 3.2.4 with the “exactRankTests” package (Foundation for Statistical Computing, Vienna, Austria) for data entry and analysis. QI Macros for Excel 2013 (KnowWare International, USA) and statistical process control charts were used for quality improvement monitoring. We compared the median TTE for patients in the two groups using the Wilcoxon signed-rank test.
RESULTS
Characteristics of study subjects
The overall number of adult nontraumatic EMS-treated OHCAs in the region prior to and after the protocol implementation was 953 and 353, respectively. There were four and nine ECPR cases attempted prior to and after protocol commencement, respectively. The median age was 44 (IQR 35-58); two (15%) were female, and 62% had initial shockable cardiac rhythms (Table 1).
Table 1 Patient characteristics and treatment data of ECPR attempts
ACS=acute coronary syndrome; CABG=coronary artery bypass graft; CPR=cardiopulmonary resuscitation; ECMO=extracorporeal membrane oxygenation; EMS=emergency medical systems; PEA=pulseless electrical activity; VF=ventricular fibrillation.
* One protocol period patient who had an unwitnessed arrest was treated with ECPR; he fell out of a boat with companions and then arrested soon afterwards; he was considered a hypothermia-related arrest and thus was not required to meet all criteria; and he was a nonsurvivor.
† Patients for whom adequate ECMO flows were unable to be established were excluded from this statistic.
Main results
Patient characteristics are shown in Table 1. Of the pre-protocol patients, all had adequate ECMO flows established, and one (25%) survived (Table 2). One patient in the pre-protocol phase was transported to a different ED within the region and then transferred with ongoing CPR to St. Paul’s hospital for ECPR initiation. After protocol implementation, ECPR was attempted in nine patients (all transported directly to St. Paul’s), seven of whom had adequate ECMO flows established and two of whom survived. Of the two patients who could not have adequate ECMO flows established (thus precluding ECPR treatment), both were found to have aortic dissection on autopsy. All survivors had favourable neurological outcomes at hospital discharge. Two patients, both in the protocol group, were determined to be organ donation candidates; for one, an appropriate recipient was identified, and organs were donated (two kidneys, pancreas, and liver).
The median TTE flows prior to protocol implementation was 136 minutes (IQR 98-196 minutes), in comparison to 60 minutes during the protocol period (IQR 49-81 minutes, p=0.017) (Table 2). The difference remained significant after removal of the one patient who was not transported directly to the ECPR-performing institution (p=0.027). A run chart can be seen in Figure 3. The median door-to-ECPR time pre-protocol was 104 minutes (IQR 53-138), and after the protocol implementation, it was 28 minutes (IQR 20-45, p=0.011).
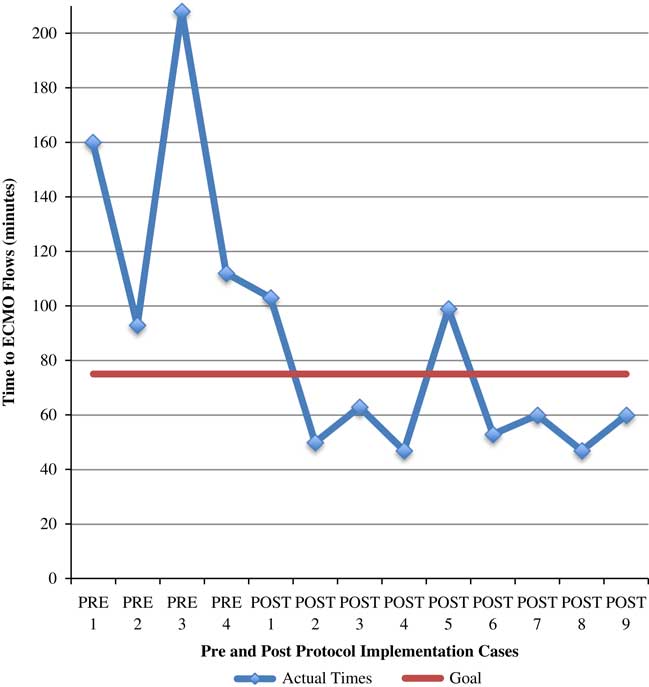
Figure 3 Run-Chart of ECPR Attempts in the Pre- and Post- Protocol time periods demonstrating Time-to-ECMO metrics.
Table 2 Patient outcomes
DC=discharge; ECMO=extracorporeal membrane oxygenation; ECPR=extracorporeal membrane oxygenation cardiopulmonary resuscitation.
The median duration of ECMO treatment among survivors and non-survivors (excluding those for whom adequate ECMO flows were not established) was 1.10 days (IQR 1.02-2.77) and 0.86 days (IQR 0.37-3.07 days), respectively. The median duration of the total hospital stay for survivors and non-survivors was 9.38 days (IQR 4.25-120.9) and 0.91 days (IQR 0.03-5.78), respectively.
DISCUSSION
We sought to improve outcomes from refractory OHCA in our region, specifically focusing on young victims of sudden unexpected cardiac arrest. We developed and implemented a structured formal multidisciplinary ECPR protocol involving prehospital resuscitation, prehospital-hospital coordination, pre-rehearsed ED management including the establishment of extracorporeal membrane oxygenation, standardized post-arrest management, and ongoing education; the goal of this protocol was to achieve ECMO initiation in under 75 minutes from first paramedic contact. We found that there was a large decrease in the elapsed resuscitation duration to the establishment of ECMO flows after our protocol implementation. Importantly, during the pre-protocol period, when patients received unstructured care, the median 136-minute TTE exceeded a reasonable time frame that patients might be expected to survive; conversely, the median 60-minute TTE under the organized protocol is more likely to lead to positive outcomes. Our protocol, including the educational aspects and the description of the development process, might assist other hospitals in determining the feasibility of achieving required time metrics to provide ECPR therapy to patients with OHCA.
During the pre-protocol time, few OHCAs were treated with ECPR, likely because of the following: 1) the lack of a formal protocol; 2) the prehospital resuscitation paradigm focused on on-scene resuscitation; and 3) the infrequent intra-arrest patients transported to the hospital were sent to the closest hospital as opposed to one where a protocol would be developed. During this time, ECPR was only considered after failed ED resuscitative efforts that made acceptable TTE metrics virtually impossible, especially during times in which non-ED personnel were not in the hospital. While comparing time metric differences in the prehospital and hospital phases of care, it appears the greatest decrease was in the hospital phase. However, an essential component of this hospital-based improvement was prehospital activation of the protocol that allowed critical preparation to occur and mobilization of non-ED personnel to attend the ED—an especially key component as the majority of cases occurred outside of daytime hours in which non-ED personnel were offsite.
We previously reported an estimate of the number of potential ECPR candidates in our region and found that of those with initial shockable rhythms, the outcomes were already excellent, with 87% surviving to admission to a hospital ward.Reference Grunau, Reynolds and Scheuermeyer 20 Acknowledging these data, we were cognizant of the risk of worsening this high survival rate while building the protocol. Our examination of time-to-ROSC survival curves determined the optimal transport time to mitigate harm to patients who might have good outcomes with conventional resuscitation.Reference Kern, Thomas and Hughes 21 To achieve the benefit of ACLS therapies both on-scene and during transport, we required that ALS paramedics attend to patients prior to transport for ECPR. This might have delayed hospital transport; however, we believed this would mitigate the risk of worsening baseline outcomes by maintaining all elements of our current conventional treatment algorithm at the scene and during transport. Our reliance on ALS-concentrated decision-making placed the experience with fewer but more experienced personnel, reducing training time and resources. In addition, we made mechanical CPR a prerequisite for transport and thus outfitted each ALS team with a mechanical chest compression device. While there is no evidence that mechanical chest compression devices are superior to manually performed CPR if applied to all OHCAs,Reference Fox, Fiechter and Gerstl 27 these devices have been shown to perform superior CPR quality during ambulance transport.Reference Lyon, Crawford, Crookston, Short and Clegg 28 , Reference Dalle Ave, Shaw and Gardiner 29
The low volume of ECPR candidates is a threat to developing and maintaining competency in an ECPR protocol for OHCA within prehospital and ED settings. Our educational and simulation program sought to develop and maintain team-based familiarity with the procedure. Volumes may be higher in other settings with less strict inclusion criteria, those with existing outcomes including fewer patients who achieve ROSC, or those with differing population demographics or density.
Although not the primary objective of our efforts, our data indicates that the application of ECPR for OHCA in Canada may result in additional opportunities for organ procurement; this has the potential to benefit additional patients, and the cost-benefit of transplantation might offset the resource-intensive nature of ECPR therapy. In addition, the opportunity to donate, which would not otherwise be possible, may be an important source of consolation to bereaved families. Consistent with any patient with severe brain injury, our program incorporates the consideration of organ donation only after the decision of patient disposition as part of comprehensive end-of-life care. In contrast to OHCA ECMO programs in which ECMO is initiated with the primary purpose of supporting organ function for uncontrolled donation after cardiac death,Reference Manara, Dominguez-Gil, Pérez-Villares and Soar 30 , Reference Ortega-Deballon, Hornby, Shemie, Bhanji and Guadagno 31 we believe that our donation practice does not represent conflict of interest.
Overall, our proportion of positive outcomes among those treated with ECPR was 27%. These data are consistent with previous reports.Reference Aufderheide, Nichol and Rea 32 Acknowledging the low sample sizes of ECPR-treated cases series, the undifferentiated mix of cardiac arrest patients with varied etiologies and baseline characteristics, and clinician selection bias, confidence in estimates of true effectiveness in terms of survival and comparisons with other sites or between different time periods are difficult to ascertain. The inclusion of non-shockable rhythms in our protocol also likely influenced our outcomes. Whereas those with refractory arrest after initial shockable rhythms might be better candidates, we elected to include patients with initial non-shockable rhythms as we hoped this therapy would be a way to improve the poor prognosis of this group. Overall, we found that non-survivors had modest impacts on resource utilization in terms of ECMO treatment durations and overall hospital stays.
LIMITATIONS
This is a single-region protocol, conducted from a single hospital with extensive experience in cardiovascular emergencies and prior ad hoc ECMO experience, but no previous formal in-hospital ECMO protocol. As such, our protocol, patients, and results might be difficult to replicate. In addition, our prehospital system, with long-standing experience in new protocols,Reference Nichol, Leroux and Wang 33 - Reference Stiell, Nichol and Leroux 35 might differ from other settings. However, we offer a description of our experience and a template upon which other interested sites might build to accommodate the various demands of their individual EMS, region, EDs, and hospitals. It is possible that eligible patients were not correctly identified and not treated with the protocol. Although the outcomes of this study might be compared with outcomes of similar patients treated with equal durations of attempted conventional resuscitation,Reference Kern, Thomas and Hughes 21 this study is unable to make conclusions about ECPR efficacy.
From an analytic standpoint, our small sample size might limit enthusiasm. However, the post-protocol improvement in TTE is so profound that it is difficult to conceive what is because of chance alone. Patients with a 136-minute TTE are unlikely to have meaningful recovery after ECPR treatmentReference Haneya, Philipp and Diez 7 , Reference Le Guen, Nicolas-Robin and Carreira 9 ; the 60-75 minute zone is likely an appropriate benchmark.
CONCLUSIONS
An organized clinical and educational protocol to initiate ECPR for patients with OHCA is feasible and significantly reduces the key benchmark of time-to-flow.
Acknowledgements
We would like to acknowledge the contributions of the following to our protocol: Cindy Lawlor, Pat Munro, Sarah Hooper, David Byres, Navreet Johal, Melissa Pearson, Demetrios Sirounis, Jade Munro, Helen Connolley, Tanya Campbell, Marianne Lesage, Laurie Fraser, Robert Schlamp, Jennie Helmer, Booby Lee, Jessica Blackbourn, John Merrett, and the St. Paul’s Hospital Senior Leadership Team.
Competing interests: None declared. Funding support was provided by Providence Healthcare Research Institute, St. Paul’s Hospital Foundation, Cardiac Services BC; Lucas chest compression devices were provided (on loan) from Physio-Control, Inc., In-Kind Support from BC Emergency Health Services, and In-Kind Support from St. Paul’s Hospital.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2017.376









