The assessment of violent behaviour and its association with mental disorder is at the core of clinical practice in forensic psychiatry. It is the main clinical skill that a forensic psychiatrist needs to develop. This chapter will concentrate on the evidence for the association between psychotic illness and violence. Most persons referred for assessment of violence to a forensic psychiatrist in the UK present with psychotic illness, mainly schizophrenia, and to a lesser extent personality disorders and sexual deviation. However, this does not reflect violence in the UK general population but a system of referral and gatekeeping of patients and clients assessed in what is a relatively small tertiary care service. Although forensic psychiatrists should be experts in the assessment of violence among people with mental disorder, it is essential to develop expertise with those who have no evidence of mental disorder. Paradoxically, these cases are often the most challenging to understand and evaluate.
Training in UK forensic psychiatry is based primarily on an ‘apprenticeship’ model and does not require passing additional examinations after becoming a specialist in psychiatry. This means that it is essential to obtain further specialist training in assessment techniques and to have some understanding of criminology. It is also important to have as much experience as possible of the different healthcare and prison facilities for violent individuals and at different levels of security. For many psychiatrists, Broadmoor, Ashworth and Rampton high-secure hospitals represent the most severe level of risk for violence, but in fact there are a group of individuals contained in special prison units who represent an ongoing level of risk for violence that cannot be contained within a high-secure hospital, some with severe mental illness.
Assessment of violence will sometimes require courage and the ability to monitor one’s personal safety based on observation, experience and training. It also requires an ability to remain objective and detached from the personal feelings that can interfere with giving a sound and helpful opinion. With experience, one’s own personal response to a potentially violent individual can be highly important in an assessment. What is it that makes one uncomfortable around or even afraid of the patient? Why is it that the patient appears to have a good relationship with one member of the clinical team but no-one else? This means learning to be aware of and overcoming the strongly negative feelings held by most persons when encountering violence and violent individuals. It helps if a forensic psychiatrist has a natural interest in violence. If not, it will be necessary to develop one.
This chapter is intended for trainees in forensic psychiatry but may be of help to more experienced practitioners because it is based on personal clinical experience, as well as involvement in research into violence. The aims are, first, to help trainees refine forensic assessments of offender patients so they can give advice to courts in determining an offender’s legal responsibility for a criminal act. Second, the chapter aims to help increase understanding of the motivation for violent offending and the pathways to violence. This is not only necessary for giving expert evidence in courts but is also essential in choosing the treatment that should be offered to a patient and the level of security required in which to deliver treatment, and in some cases it may be relevant to the likelihood of a successful response to the treatment. Third, the chapter shows that associations between criminal behaviour and mental disorder may be highly important in the assessment of risk for future reoffending, although this chapter does not deal with risk assessment as currently operationalised in many North American and European forensic services. Finally, and most importantly, the chapter emphasises that a good forensic assessment should concentrate on the future management and prevention of further violence.
Evaluating Research, Risk Assessment and Considering Causation
This chapter covers a wide-ranging area of research and clinical observation and should be considered as an overview. When considering research, it is important to evaluate the current literature on mental disorder and violence, what it means for the practice of forensic psychiatry and why some is highly limited and even unhelpful. The chapter also aims to give some indication of future directions for research into violence for forensic psychiatrists.
This chapter will not consider risk assessment for violence, which is covered in Chapter 6 and by means of specific training. However, the assessment of violence for planning a treatment intervention or giving evidence to court should not be confused with an assessment of future risk for violence. For example, many current research limitations derive from an overemphasis on research methods used to develop instruments which aim to predict violence. Some disciplines have even come to confuse assessment of violence with assessment of risk. There is no reason not to carry out both forms of assessment. From the perspective of the assessment of violence, a numerical score of future risk can be helpful in a limited sense by categorising individuals based on their previous behaviour and demography. However, these predictions stand a good chance of being wrong in the narrow sense of estimating future likelihood of violence.
There is no current high-grade research evidence which demonstrates that a structured clinical risk assessment instrument or an actuarial risk instrument can prevent an act of violence following discharge from hospital or release from prison. The only randomised controlled trial to date which tested a structured professional judgement instrument against management as usual failed to show a significant reduction in violence following hospital discharge [Reference Trochette, van den Brink and Beintema1]. There are two randomised controlled trials which demonstrate a significantly reduced count of violent acts among patients in hospital who were assessed for short-term risk by nurses [Reference Abderhalden, Needham and Dassen2, Reference van de Sande, Nijman and Noorthoorn3]. However, closer examination reveals these risk assessments were tied to the requirement by clinical teams in the intervention arm of these studies to select, then carry out, active interventions based on a score of risk.
These findings indicate that it was very likely that the clinical preventative intervention was the active and effective component resulting in reduction of violence and not the risk assessment. Clinical experience with violent patients soon reveals a range of different chance events and circumstances that can interfere with one’s predictions of future behaviour. The most important clinical use of risk assessments should therefore be to determine the necessary treatment and management options to prevent future violence rather than categorising patients according to risk scores, or speculative notions of future risk based on a training session in structured clinical judgement. No risk instrument can consider all possibilities and the increasing proliferation of these instruments for different forms of violence emphasises these clinical limitations. No new statistical development or advance in machine learning can substitute for professional experience. However, they can help as an important aide-memoire and ensure that key areas are not forgotten in an assessment.
Multiple limitations of violence research are shown when attaching too much importance at the individual level to results from surveys and, most importantly, to case register studies – no matter how large the sample size and despite claims the sample represents the entire population of a country. It is important to question whether the published research has any bearing on forensic clinical practice. The forensic psychiatrist should have multiple sources of information before conducting an assessment, and experience soon shows that most epidemiological studies are remarkably short of the key variables that determine violence. These studies are important in suggesting avenues for future research and creating new hypotheses. However, interpretations such as violence being substantially determined by genetic factors, while a possibility, cannot be relied upon in studies that use data that was never intended for the purpose of genetic study and that depend entirely on sparse data on siblings and criminal records to determine genetic association.
Forensic psychiatrists should have a healthy scepticism of studies where the statistics are so dense and complex that they are incomprehensible to the average clinician. There have been a series of studies of violence using the Scandinavian case registers where patients – sometimes all patients in a country captured by the register with a psychiatric diagnosis who have had contact with hospital and out-patient/community services – are linked with police records. Apart from the fact that neither register was designed for the study of either complex criminal acts or mental illness and that both are merely administrative registers to record the performance of services, criminal records are a poor indication of violence in a population and convictions and arrest records represent the last stage along the criminal pathway in which mentally ill persons are disadvantaged at each stage. Most Western countries now rely on self-report surveys of victims of crime to get a picture of crime trends and do not rely on official police statistics alone. But more importantly, the presence of a categorical diagnosis in a register does not mean that symptoms of mental illness or intoxication from drugs or alcohol were actually present at the time the violence occurred.
This key data is simply not available in the Scandinavian case registers. Closer examination shows that this is an unsubstantiated assumption on which to base conclusions such as that depression causes violence, drugs and alcohol cause violence among persons with schizophrenia (but not their schizophrenic illness), a substantial proportion of all violence in a population is genetically determined and so on. If the data does not include the social circumstances and other potential social determinants of violence and whether symptoms of mental illness were present at the material time, together with observational effects of those symptoms on the violence, it cannot be determined whether any of these factors had any impact or whether unknown confounders not included in the register were the key drivers.
Epidemiology of Violence
Violence, according to the World Health Organization [Reference Krug, Dahlberg, Mercy, Zwi and Lozano4], is ‘the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment, or deprivation’. Although violence is a criminal behaviour, before it is formally deemed a crime the violence must have been observed and reported to the police, the individual must be arrested, a decision must be made to prosecute, and the offender must appear at trial in court before a final conviction. The verdict may be ‘not guilty’. It is therefore important to remember that the overwhelming proportion of violence in all countries is not reported to or detected by any official agency. Criminologists refer to the ‘dark figure’ of crime: that which is not reported in official criminal statistics, which only represent the ‘tip of the iceberg’ of actual crime in a population. This means that when evaluating epidemiological research evidence, it is essential to be fully aware of the limitations of the measures of violence in the research study.
Psychiatric studies of violence are bedevilled by poor measures of violence. If a study relies entirely on criminal convictions, this means the majority of violent events in the population have been missed and cannot be included in the study. It is estimated that 95% or more of all violent events will not be reported to the police. Although it is argued that if more serious crimes such as homicide are studied, then more violence will be included, it still has to be remembered that even in Western countries with resources to conduct careful investigations, a proportion of offenders will never be arrested or convicted. In countries with exceptionally high homicide rates, such as in Central and South America, nearly half of offenders may never be arrested. Most importantly, persons with mental illness are more likely to be detected, arrested and convicted than other offenders. Furthermore, for those who are violent in hospital, the violence may not be reported to the police unless serious injuries occur. In the UK, however, this is changing as staff become less able to respond to and less willing to accept violence from patients, particularly in community-based services.
Homicide and Mental Disorder
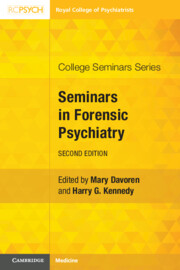
It is important to place violence in the UK in an international context. The most extensive information for comparison purposes is recorded for homicide. Rates vary greatly between world regions [5]. Homicide is considered the best comparator for international purposes because it is seen as the most serious violent offence and more time, effort and financial expenditure is invested in its investigation. However, not all deaths are accurately identified as homicides or the perpetrators identified. Overall, less than 1% of all global deaths are due to homicide, but in some countries this is as high as 10% and a leading cause of death. Rates are highest in Central and South America and South Africa and lowest in certain East Asian countries and western Europe (see Figure 1.1).
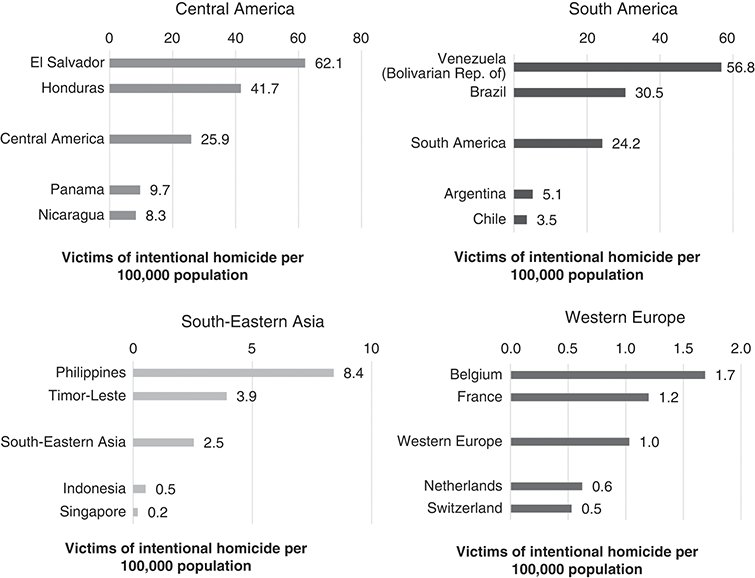
Figure 1.1 Countries with the highest and lowest homicide rates in selected subregions, 2017.
Figure 1.2 shows the number of deaths internationally by cause for all ages. Homicides are not the leading cause of death. However, if the histogram includes younger persons aged 15–49 years, it rises to the ninth most common cause. If the data is applied to Venezuela in 2017, homicide was the third, in Honduras the fifth and in Guatemala the sixth most common cause of death. Looking at younger adults aged 15–49 years in Latin American countries, homicide is the highest-rated cause of death.

Figure 1.2 Causes of death.
Homicide rates appear to have fallen in all regions over the last quarter century. But because the global homicide rate is calculated as a proportion of the population, it has declined only because the global population has risen. The overall number of people killed worldwide in homicides actually increased from 1990 to 2017. During this same period, homicides due to criminal activity caused as many deaths as armed conflicts and terrorism combined. Women and girls account for a far smaller share of victims of homicide in general than men. The majority of all homicides involve young men, both as perpetrators and victims. However, women bear by far the greatest burden of family-related and intimate partner homicide as victims.
Rises and falls in homicide rates in most countries are largely explained by changes in rates among young adult males with no mental illness. Pinker has argued that there has been a dramatic fall in homicide since the Middle Ages, measured largely in Europe and more recently North America, and that humans are becoming less violent and more altruistic [Reference Pinker6]. However, not all academics agree in that violence changes in its form and fluctuates over time. For forensic psychiatrists, a key issue is whether violence has fluctuated over time among the severely mentally ill. However, there is little evidence to indicate change over time using homicide statistics, which may be the best data available but are dependent on processing through the criminal justice system; also, different jurisdictions differ in how they deal with mentally disordered offenders. If this data can be relied upon in England and Wales, homicide rates for the mentally ill appear to have remained the same, while those for other offenders have changed over time [Reference Coid7].
To understand violence in a single country, it is necessary to observe fluctuations in rates rather than relying on cross-sectional surveys and case register studies, which take measures over short time periods – although these often represent the only detailed data available. Changes in exposure to risk factors affecting this subgroup of the population include the availability of firearms, gang involvement, changing involvement in criminal activity (particularly drug trafficking and sales) and the consumption of alcohol. The impact of these social and environmental factors means that the public health problem of violence has to be considered. Forensic psychiatrists should be aware of local, population-based factors in their catchment-area populations and when giving opinions on cases in other jurisdictions. Changes in homicide rates involving women rarely make an impact on fluctuations or changes in national homicide rates. For example, the homicide rate for Scotland became the highest in western Europe by the 1990s, but then fluctuated. Further rises and subsequent falls in homicide rates in Scotland between 2000 and 2014 were entirely accounted for by men. Meanwhile, women showed a small, progressive decline over the same period.
There is also no current evidence that changing rates of homicides are explained by persons with mental illness. Although it may make complete sense to a forensic psychiatrist that the closure of the mental hospitals and shift of patients into the community should have led to an increase of recorded violence by mentally ill persons, this has not been convincingly established and study findings remain controversial. In 1939, English mathematician, geneticist and psychiatrist Lionel Penrose hypothesised that the numbers of psychiatric hospital beds and sizes of prison populations were inversely related. The hypothesis fell out of favour in the 1980s, by which time bed closures had become a more accepted aspect of ongoing changes in psychiatric provision in most of Europe and North America. The hypothesis was revived by the work of Mundt and colleagues more recently in South America, showing that the prison populations in 17 Latin American countries had substantially increased and that they had increased more where more psychiatric beds were removed [Reference Siebenforcher, Fritz and Irarrazaval8]. These findings held up when introducing per-capita income and income inequality as co-variates. However, it remains unclear and controversial whether serious violence by persons with severe mental illness has increased as a result of bed closures.
An earlier study in England and Wales [Reference Taylor and Gunn9] observed the overall rise in homicide rates in England and Wales but demonstrated that court adjudications, resulting in successful diminished responsibility and insanity defences, had remained remarkably stable over a 30-year period, during which the overall rises had occurred. Subsequently, it was claimed there had been a rise and then a fall in homicides attributed to mental disorder over a 50-year period, the fall coinciding with a fall in the overall homicide rate [Reference Large, Smith, Swinson, Shaw and Neilssen10]. However, these observations were dependent on small numbers of cases each year and, most importantly, processing through the criminal justice system to identify the mental disorder. The change was more likely due to a change in the willingness of psychiatrists giving evidence in courts to recommend defendants for a defence of diminished responsibility and offer a hospital bed, particularly for those with personality disorder, rather than a true rise and fall in homicides involving mental disorder. It is worth reflecting that in Western countries, particularly in Europe, where there are few homicides, a larger proportion (but not rate) with mental disorder will make it appear that there is a large problem of violence by the mentally ill. In countries with very high rates of homicide, homicides by the mentally ill may appear to be negligible. Paradoxically, stigmas involving the mentally ill are often similar in both locations.
A key unresolved question is whether rates of homicide by mentally ill persons are the same or differ between different countries. An early study showed that they were apparently very similar, but this was based on countries with low overall homicide rates [Reference Coid7]. A later study criticised this argument and suggested that if countries with higher overall rates were included, then the rate among the mentally ill would correspond to the overall rate [Reference Nielssen and Large11]. This would imply that in countries with high overall rates, with specific risk factors influencing these high rates such as firearm availability, persons with mental illness would be proportionately influenced by these same risk factors – in the same way that persons without illness are affected. In a country such as the USA, with ready availability of firearms, rates should therefore be higher for persons with severe mental illness than in the UK. However, this possibility ultimately remains unresolved due to a lack of data from countries with high homicide rates. Countries with the highest homicide rates tend to have low clear-up rates or do not routinely screen for mental disorder. In countries with multiple unsolved murders, drug cartels and readily available firearms, mental illness is simply not considered a likely or relevant factor in the overwhelming majority of cases. This is an important consideration in countries with low homicide rates. If media attention and public opinion does not keep these issues in perspective, concern can arise that homicide by the mentally ill is a major problem when it is in fact exceptionally uncommon. It is therefore essential not to confuse percentages of the total number of homicides with age-standardised population rates.
A key epidemiological finding with regard to psychotic illness and homicide is that, for schizophrenia, it is the prodrome and during a first episode of psychosis (often the period of greatest symptomatic disturbance over the lifespan) that is most strongly associated with homicide – a relatively short timespan over the entire life course. In a meta-analysis, approximately 30% of homicides in a range of countries were found to have occurred prior to ever receiving treatment. The risk during this period was 12 times that during the rest of the lifespan following a diagnosis of schizophrenia [Reference Nielssen and Large11]. As the first episode of psychosis is relatively short compared to the total duration of the illness, the risk of homicide during a first episode is therefore considerably greater than the annual risk among individuals with treated psychosis. This confirms that a first episode is a medical emergency and suggests that reducing the duration of untreated psychosis might save lives. However, because many individuals committing homicide during a first episode will not be known to mental health services, this may be difficult to achieve. Furthermore, the illness may only be identified as a result of the homicidal behaviour.
In a national nested case–control study of previously admitted male patients diagnosed with schizophrenia in England and Wales, those who were convicted of homicide were statistically more likely to be non-adherent to their treatment plan; had lost contact with services prior to the offence; had a history of violent criminality, comorbid personality disorder or drug use disorder; had been admitted to hospital multiple times; and belonged to a black and minority ethnic group. Homicide perpetrators were less likely to have had recent routine contact with services and to have been recently discharged from hospital [Reference Baird, Webb, Hunt, Appleby and Shaw12]. It was subsequently argued that these findings showed that much of the risk of serious violence in schizophrenia is related to comorbidity with alcohol or drug misuse, corresponding to previous research, with similar conclusions to the national Scandinavian case registers study and a related meta-analysis [Reference Fazel, Gulati, Linsull, Geddes and Grann13, Reference Fazel, Langstrom, Hjern, Grann and Lichtenstein14]. However, none of these studies had information on whether psychotic offenders were actually intoxicated or had even taken any drugs or alcohol at the time of the violence to confirm this assumption and rates for schizophrenia in England and Wales were not standardised to be able to tell if there had really been a trend over time. They did, however, show that 90% of homicide offenders with schizophrenia had psychotic symptoms at the time of the killing, meaning that intoxicated or not, psychotic symptoms may have driven the homicide in a proportion of cases. Substances may have interacted with the acute psychotic process at the time, but no data was available to confirm this.
This is an important study with important epidemiological findings, but methodological limitations make it difficult to interpret the implications of substance misuse for homicide by persons with schizophrenia. The uncertainties of these study findings directly impact on clinical forensic practice because it is the role of a forensic psychiatrist to be absolutely sure when giving an opinion to the court whether psychotic symptoms were a causal factor at the material time of the homicide, and to give a precise opinion on the role of substance misuse. Such opinions cannot rely on a comorbid diagnosis of substance misuse at some undefined time in the past. Furthermore, when giving opinions on treatment and management, ensuring compliance with treatment and follow-up is highly important in preventing future violence in persons treated for schizophrenia. Patients who abuse substances are more likely to be non-compliant with medication and follow-up and thereby are at greater risk of relapse.
Non-lethal Violence
Homicide is an unusual violent crime with particular characteristics. The overall level of violence in a population can be obtained from non-lethal violent crimes which are recorded by the police, but many countries also record self-reported violence using surveys carried out at regular time intervals. These can give a different picture. For example, an earlier study of crime rates in the USA and England and Wales covering 1981–96, comparing New York and London, showed a considerably higher homicide rate in New York, whereas common assault and robbery were somewhat higher in London [Reference Langan and Farrington15]. A fuller picture can be obtained if these statistics are further supplemented with hospital episodes, where violence victims are registered at hospitals. However, definitions of violent offences vary between countries due to legal differences and statistical recording methods. Useful comparisons may be adversely affected by these differences. Violent crime in England and Wales is measured using two different sources: the British Crime Survey (BCS) and police-recorded crime. Police-recorded crime is a good measure of trends in well-reported crime and also of less common but more serious crimes. However, the BCS provides the most reliable measure of victimisation and national trends over time and is not affected by whether the public report crime or by changes in the way the police record crime. It is essential to be aware of the context of these trends over time when carrying out an assessment, as well as when evaluating research. From the epidemiological perspective, it can then be questioned whether psychiatric morbidity has any impact on these trends. Apart from changes in patterns of drug and alcohol misuse, there is little evidence that it does.
Crime in England and Wales, including violent crime, increased between 1981 and 1995, after which it fell sharply but then stabilised, according to the BCS, with a fall in violent crime of 41%, or half a million fewer victims, after 1995. This was accounted for by large falls in both domestic and ‘acquaintance’ violence, whereas stranger violence remained stable. Those most at risk of violence are young men aged 16–24 years and unemployed people. The risk of violence varies according to lifestyle characteristics, reflecting differences in social interaction. For example, people who visit pubs and bars are more at risk of violence than those who do not. Figures for 2000 onwards showed a progressive fall in violence using police-reported incidents, the BCS and hospital-treated injuries [Reference Sivarajasingam, Page, Green, Moore and Shepherd16]. However, during the period after 1995, a steady rate of violence was observed in certain UK inner-city areas, particularly London. These observations are important because they show that violence in a population can both rise and fall over time and clinicians should be aware of whether they are in one of these time periods. There is no convincing evidence that severe mental illness has an impact on rises or falls in violence, but this must be considered in the context of studies not yet carried out to test this possibility and where many studies are conducted in countries with good data, social stability and consequent low rates of violence.
Violence is a highly social activity and patterns of self-reported violence in England and Wales during the COVID-19 pandemic were influenced by government instructions to limit social contact. Although there was no change in the total number of violent incidents, the total number of victims of violent crime decreased by 28% in the year ending March 2021 compared to the year ending 2019. The number of homicides fell by 16%. A fall in violent crime was driven by decreases in violence where the offender was a stranger, corresponding to a fall in violence in public spaces. However, when considering the effects of COVID-19 on violence, it is important to also consider the international perspective. Violent crime in the USA had also shown a progressive fall over a similar time period, as shown in Figure 1.2. However, for the year 2020, homicide showed the sharpest increase in certain states and among poorer persons and minorities for many years.
An alternative source of information regarding the prevalence of violence is self-reported violence obtained from national surveys. The national survey of psychiatric morbidity among adults living in households in the UK in 2000 was the first in the UK to include questions on violent behaviour and to compare violent behaviour with psychiatric morbidity in a representative sample of the population [Reference Singleton, Bumpsted, O’Brien, Lee and Meltzer17–Reference Coid, Yang and Roberts20]. Figure 1.3 demonstrates the prevalence of self-reported violence among adults in the UK aged 16–74 years over the previous five years, in a survey in 2000 and 2007. This shows findings repeatedly found in international studies, indicating violence decreases with age and is less prevalent among women. Figure 1.4 compares reported victims of violence, according to the sex of the respondent. It confirms that the primary public health problem among the British household population is violence from men towards strangers or other persons known to them. These patterns are partly reflected in the national homicide statistics, as described earlier. Violence outside of the home and involving strangers can be thought of as just one among a series of hedonistic and negative social behaviours (including hazardous drinking, drug misuse, sexual risk-taking and non-violent antisocial behaviour) exhibited by a subgroup of young men [Reference Shepherd and Farrington21].
However, Figure 1.4 also shows another unexpected and controversial finding. Using self-report data, women report more violence towards an intimate partner than men and more violence towards a child than men [Reference Yang and Coid22]. These observations contrast with victim reports which suggest that intimate partner violence (IPV) is experienced more by women. However, most studies show that reporting injury is more likely when the victim of IPV is a woman. Considering these findings, the primary public health problem of most countries is not IPV but male-on-male violence among young men. Furthermore, self-report data from UK national surveys indicates that a minority of men who are violent to their partners are only violent to their partners, and that men who perpetrate IPV tend to be generally violent with more than one type of victim [Reference Yang and Coid22]. This epidemiological finding has major implications for treatment interventions and prevention of IPV, suggesting that focussing on IPV alone will be ineffective for the majority of these men.
Violence by Women
Men are more violent than women. Sex differences in aggression are thought to be explained by greater male physical strength and testosterone, as well as socialisation in childhood to be more aggressive. A key issue is whether psychiatric morbidity has an impact on violence by women relative to men. Population studies show that men are more likely to abuse alcohol and be dependent on drugs and alcohol, and to have antisocial personality disorder (ASPD), conditions associated with violence in general population studies. Women are more likely than men to receive ‘no psychiatric diagnosis’ or a diagnosis of affective or anxiety disorder; the latter is associated with somewhat higher risk but at a level lower than other diagnostic categories. One study [Reference Yang and Coid22] found that although ASPD was more common in men at the population level, when it occurred in women it posed a greater risk of violence than in men, although this might be because it was more likely to be comorbid with anxiety and affective disorders, including borderline personality disorder, than in men. However, the ‘threshold of risk’ (gender paradox or group resistance) hypothesis argues that females who develop antisocial behaviour have a higher threshold of risk than males and that violent females are more severely afflicted with mental disorder than males. The female threshold is presumed to be raised by the gender-role socialisation against aggression of women at the level of culture. The push over this threshold is presumed to come from psychobiological or developmental factors at the level of the individual. If more severe aetiology is found for women, then the inference is made that a higher threshold for women therefore exists. A population study found that women who were violent experienced more severe anxiety, affective disorder and personality disorders than men who were violent [Reference Yang and Coid22].
Public Health Implications of Psychiatric Morbidity and Non-lethal Violence
Using the British National Household survey, psychiatric diagnoses that had relatively high prevalence in the population, such as affective/anxiety disorder and personality disorder, accounted for a large proportion of all violent incidents. Hazardous drinking, which involves intermittent bouts of heavy drinking, was associated with half of all incidents. In contrast, people who screened positive for psychotic illness constituted a very small percentage overall of people with psychiatric morbidity and accounted for a very small percentage of all violent incidents. However, people with alcohol dependence, drug dependence and ASPD, while having a relatively low prevalence in the population, did account for a relatively high proportion of all incidents [Reference Coid, Yang and Roberts20].
One approach to measuring the impact of a disease at the population level is to calculate the population attributable risk (PAR), which is the incidence of a disease in a population associated with (or attributable to) exposure to the risk factor and is used by epidemiologists to consider which preventative interventions should be used, particularly whether these should be targeted towards individuals or at the population level. This is often expressed as a percentage. Using Swedish case register data, Fazel and colleagues [Reference Fazel, Langstrom, Hjern, Grann and Lichtenstein14] estimated that 1 in 20 persons with schizophrenia and associated psychoses diagnosed by clinicians and included in a national case register were convicted of violent crimes in Sweden. Looked at differently, this means that if the risk exposure of severe psychosis could be eliminated in Sweden, there might be 5% fewer violent convictions in Sweden. However, reliance on criminal records data means that the overall impact of psychotic illness on violence may be greatly overestimated. Using self-reported violent behaviour but using a screen for psychosis (a less robust diagnostic measure), the PAR for violence was only 0.7% in a representative population sample of England, Scotland and Wales [Reference Coid, Yang and Roberts20]. Furthermore, persons who screened positive for psychosis only accounted for 2% of all self-reported violent events over a five-year time period in this population. This difference may have been partly due to the diagnostic measures used. However, it was more likely due to an underestimation of the overall level of violence using criminal records and where persons with severe mental illness are more likely to be convicted.
In contrast, hazardous drinking (a pattern of intermittent bouts of excess drinking) was found among 27% of the British population with a PAR of 47%, and with over 50% of all violent events over the past five years self-reported by this population. Drug misuse was found among 10% of the population (most frequently cannabis) and showed a PAR of 37%, with drug users accounting for 42% of all violent events. Overall, these findings do not suggest that targeted interventions for people with major psychosis would have a large impact on the overall level of violence. A reduction by 5% might include a large number of violent incidents across an entire country. But this needs to be considered in the context of a country such as Sweden with a relatively low rate of serious violence and in the context of the measure of violence used in the case register study – violent convictions in a criminal court. If the aim were to reduce a larger amount of violence using a population approach, then limiting access to alcohol and reducing alcohol consumption among hazardous and harmful drinkers is likely to have the largest impact nationally, particularly among young men. The figures also suggest that reducing drug consumption may have a major impact. However, when using PAR measures to estimate the impact of interventions, it is important to consider their main limitations. A PAR assumes that the condition being eliminated from the population has a direct causative effect on the violent behaviour. This cannot be assumed for factors such as drug misuse, where associations are highly complex and can include reverse causation.
Overall, the largest public health impact on serious and repetitive violence was exerted by hazardous drinking. The relationship between drinking and violence was strong among young people and those who conducted a high percentage of their drinking in bars. These findings indicate that public health population approaches involving risk reduction programmes to encourage healthy drinking and control of outlets, particularly those associated with drunken disorder, many within the ‘night-time economy’, are the most appropriate preventative interventions.
The position with regard to ASPD differed from that of alcohol. Despite a relatively low prevalence in the population, individuals with ASPD make a substantial contribution to violence and serious violence. Eliminating exposure to this disorder would have reduced the proportion of individuals who reported injuries to other persons by almost a quarter. This indicates a subgroup suitable for targeted (or secondary and tertiary) prevention strategies. This group were more likely to injure victims and their violence was repetitive. They assaulted multiple different victims and in different locations. However, targeting this group poses logistical and moral problems. They represent approximately 2% of the population in different Western populations. This is a substantial number of individuals, far beyond the scope of mental health and criminal justice services for interventions such as selective incapacitation [Reference Davoren, Kallis, Gonzalez, Freestone and Coid23]. There is also no intervention that is currently known to be successful with this subgroup. Furthermore, if reliance were placed on the diagnosis of ASPD to identify these individuals, despite a high prevalence of violence among this subgroup, half were not found to have been violent in the past five years despite living an otherwise highly antisocial lifestyle [Reference Singleton, Bumpsted, O’Brien, Lee and Meltzer17–Reference Coid, Yang and Roberts20].
Psychosocial Risk Factors and Mental Illness
It is correct to say that certain social characteristics of an individual are often more strongly associated with future involvement in violence than the presence of mental illness [Reference Bonta, Law and Hanson25]. However, this argument was based on simple statistical associations in a literature review. This review is sometimes used to incorrectly claim that it is psychosocial risk factors and not the mental illness that causes violence among the mentally ill. It is indeed correct that there are strong interactions between different psychiatric conditions and the psychosocial circumstances of people with mental illness. A good forensic assessment will disentangle these components. Unfortunately, few research studies investigate these interactions. This has also led to simplistic claims that it is rare that the presence of a mental illness will provide a causative explanation for an act of violence [Reference Monahan, Steadman, Dvoskin, Skeem, Novaco and Douglas26, Reference Skeem, Kennealy, Monahan, Peterson and Appelbaum27]. Careful examination of this research shows it was based on an earlier misunderstanding of the associations between risk factors in statistical models used to create predictive models for future risk for violence. Mental disorder appeared to come out worse in the models in terms of its relative predictive power when the usual measure of a mental disorder was a diagnostic label which paid no attention to whether symptoms of the disorder were present or absent at the time of the violence. In most of these studies, the diagnosis had been made well in advance of the violence. These risk prediction models are seriously flawed, as described earlier, and did not consider the possibility that mental disorder could be causal, as in the case of when symptoms are present at the time and drive the violent behaviour.
More recently, it has become more important in research to consider whether symptoms of mental disorder were actually present at the time of the violence to be directly relevant to the violence, and this is a key requirement in a forensic assessment. Forensic psychiatrists should not engage in an ‘either/or’ debate as to whether it was the mental disorder or the psychosocial circumstances that caused the violence. Both are likely to be important. Unless symptoms of mental illness can be ruled out as being present at the material time, a more sophisticated analysis involves understanding how psychosocial factors influenced mental disorder, and vice versa, along the pathway to violence. Nevertheless, it is rare to find that psychosocial factors had no impact on mental illness to result in violence. Mental disorder, particularly severe conditions like schizophrenia, tends to be found among persons of lower social class and living in areas of higher socioeconomic deprivation. Persons with severe mental illness tend to drift down the social scale, with difficulty managing finances, debt, housing instability and increased likelihood of homelessness. They often live in social environments where there is increased risk of being preyed upon by others, resulting in violent altercations and where the violent incident may not have had a direct association with their symptoms, apart from the symptoms making them more likely to be identified as a target of violence by others. At the same time, they are often socially withdrawn and come into contact with fewer persons, mainly carers, who may be at risk from them during episodes of psychosis. A forensic assessment of an individual should not be influenced by overarching statements based on the theoretical position of a discipline striving for dominance in the field of violence studies and stick to the facts of the case at hand.
Causation
At the heart of a good assessment is an understanding of the cause or causes of the violence by the forensic psychiatrist to be able to prepare a report and give useful advice to colleagues in second opinions. Courts expect psychiatrists to be able to explain the violent offence and assume that psychiatry has something special to offer that other disciplines do not. Courts will rigorously test expert evidence if they say the defendant has a defence at law for their behaviour due to a mental illness. Colleagues will expect a forensic psychiatrist to be able to explain why a patient under their care does not respond to their interventions, why they continue to be violent and what to do about it. They will want to know whether the patient is in the correct level of security for the protection of staff and other patients.
In clinical practice, there will seldom be a single cause for violence. It is important to be able to assemble the multiple factors leading directly to violence, together with the factors that did not cause the violence but made it more likely to occur when it did and where it did. It is helpful to consider a pathway to violence. Although focussing on psychiatric morbidity, it is important to remember that situational factors are of considerable and often prime importance, sometimes involving unique and unexpected occurrences in an individual’s social environment. There is also usually more than one motive for violence that can be identified and it is important to be clear about whether violence is driven by symptoms of mental disorder, whether there are elements of intoxication with disinhibition, whether there is mood disturbance such as irritability and anger, whether the violence was provoked by the behaviour of others or triggered by certain key factors, and whether there was evidence of planning beforehand. Experienced forensic psychiatrists typically put together a causal chain, or pathway, as a mechanism to understand violence, considering the above and multiple other factors they identify during a good-quality assessment. In assessing previous violent behaviour, the psychiatrist is examining a process of what are usually multiple causes in the past and effects which lie in the future in terms of time and space (or place). In the case of assessment of disturbed and violent inpatients, these causal factors may be directly observable during the examination of the patient and in the patient’s physical environment, such as the hospital ward, together with the social interactions between the patient and other patients, friends, and relatives and staff. Problems arise, however, when attempts are made to extend the assessment to future behaviour if no causal associations can be established as a target for intervention.
Many statistical predictors of future violent behaviour such as young age, number of previous convictions and so on, typically used in a risk assessment which uses actuarial scores to determine future risk based on statistical models, are not amenable to clinical intervention. Using a statistical ‘predictive’ model of future behaviour, these have stronger statistical power because past behaviour is a reasonably recurring statistical predictor of future behaviour – but with considerable limitations in the real world. More importantly, few are causal factors for violence and, paradoxically, causal factors are often poor predictors in statistical models. If the intention is to effectively intervene and prevent violence, then it will be necessary to identify the factors which are causal, even if the causal factor does not appear to currently be in operation. The art of assessment is to understand the causal chain and determine whether it is likely to re-occur and to understand if and when there should be an intervention. If the individual has multiple previous violent convictions, this gives some strong indication statistically of future risk but little indication of causation.
However, if each of these offences were against victims who had been incorporated into delusions of persecution, typically occurring when the patient ceased to take medication and the symptoms re-occurred, this would give some indication of the cause or causes of the violence and a possible solution to future prevention. But the latter would then involve assessment of whether the individual responded to treatment for delusions, whether they were likely to cooperate with treatment again in the future and how this might be assured, and multiple other factors based on extensive clinical experience that cannot be packaged into a course on risk assessment by trainers who are not clinically experienced and licensed to administer certain treatment options such as medication. Having said this, clinical assessment of violence can and sometimes should include a structured assessment of future risks. However, this is peripheral to the main task of understanding why an individual has been violent and most importantly what has caused the violence. Despite an earlier, negative commentary on the standard method of medical history-taking when assessing potentially violent persons for an assessment of future risk [Reference Krug, Dahlberg, Mercy, Zwi and Lozano4], forensic psychiatrists should ignore this and continue to use the standard approaches they have been taught during their medical training, and ignore spurious criticisms from other disciplines of the ‘medical model’.
Research into violence and mental disorder remains short on studies that attempt to establish causation. Using a predictive approach in what are usually pseudo-longitudinal designs, research studies have typically used ‘lagged’ statistical models. For example, a factor occurring in the past six months is used to predict violence occurring in the subsequent six months (or over a longer period). In a temporal proximity or causal model, both the predictor and outcome are measured in the same time window (e.g. the same six months, or more ideally during shorter time periods). The former, lagged or ‘predictive’ model is used in all studies which attempt to create new risk assessment instruments and also to validate these instruments. However, this model cannot evaluate causation for violence because the factor found associated with and sometimes incorrectly thought to have caused the violence may not have actually been present at the time the violence occurred. A good example is the Swedish case register studies which concluded that violence in schizophrenia was due substantially to substance misuse [5, Reference Pinker6]. However, having drawn this conclusion, closer examination shows that it is impossible to conclude, firstly, that symptoms of schizophrenia were present at the time of a violent offence and, secondly, that persons diagnosed with schizophrenia had taken drugs or alcohol at the material time the violence occurred.
Symptoms of psychosis fluctuate, sometimes on a day-to-day basis, and it is necessary for a forensic psychiatrist to have a considerable degree of certainty that they were present at the time of the violence when giving evidence in court, otherwise their evidence will be discredited. The best example of the confusion that can occur in research is shown in the re-analysis of the MacArthur study data [Reference Coid7] where it had originally been asserted that delusions did not either cause or predict violence [Reference Siebenforcher, Fritz and Irarrazaval8]. Most experienced forensic psychiatrists will find such assertions counter-intuitive and not based on their clinical experience. Patients with schizophrenia frequently explain their violence on the basis of their delusional beliefs. Depositions and sometimes witness statements will reveal assertions by a patient that violence was due to a delusional belief. In this context, re-analysis of the same MacArthur data using a causal model, aiming to demonstrate causality, revealed that the predictive model had missed the fact that the delusions were strongly associated with violence, but that only certain delusions caused violence, and that angry affect due to the delusions had to be present for violence to occur. Because the delusions had fluctuated in severity over a one-year follow-up period, unless the measures were taken at frequent intervals over this time period and a statistical method was used to test whether symptoms and violence coincided during a narrowed timespan, the statistical association between the two would be totally missed. Interestingly, the re-analysis found that it was entirely correct that if an observation of delusions was made at the time of discharge from hospital and then tested to see if they statistically predicted violence over the follow-up, delusions could not accurately predict violence occurring at either 6 or 12 months later using a lagged model. Delusions did indeed not predict future violence among released psychiatric patients. However, using a causal model, delusions were found to have caused violence.
These criticisms of existing research are important for clinical assessment. For example, violence among persons with schizophrenia can occur at times when no symptoms are present and when the patient is intoxicated. It is unlikely a defence can be established in court if no symptoms were present, and courts are not sympathetic to excuses of intoxication for violence. Intoxication and repeated episodes of substance misuse can precipitate symptoms of psychosis in predisposed individuals, but it will be necessary to give supporting evidence that it was the symptoms that caused the violence and not the intoxication. When giving evidence, that may be hard to achieve. Correspondingly, it would be poor clinical practice to conclude that because an individual had a history of substance abuse in the past, violence during an acute psychotic episode when there was no evidence of substance misuse was primarily due to the latter. Because establishing associations between violence and psychosis is so important, the present mental state at interview should never be relied on alone when forming an opinion. It is important to seek all sources of information prior to and following the violent act from case records and from witnesses, or their statements, and to get the client’s account of the symptoms’ progress over time and how they think they influenced the violence, then come to their own opinion. The most relevant information in the case of a serious offence may be the police interrogation because it is close in time to the offence and the individual is under pressure to give an explanation. It is particularly helpful to have training in using standardised research instruments, which include a comprehensive series of questions to elicit psychotic symptoms such as the World Health Organization’s Schedules for Clinical Assessment in Neuropsychiatry (SCAN), but also to know how to elicit lifetime diagnoses using instruments such as the World Health Organization’s Composite International Diagnostic Interview (CIDI). During assessment, it will be necessary to focus on whether they were experiencing these symptoms at the time of the offence and elicit whether symptoms motivated or ‘drove’ the behaviour.
Research into Causal Effects of Psychotic Symptoms on Violence
A clinical diagnosis is a construct created for research and clinical purposes and is unhelpful and can be misleading when applied to the study of violence, apart from grouping patients into broad categories. Surprisingly, there has been only limited study of the associations between violence and psychotic symptoms, even though clinicians need to establish that symptoms were present at the material time of the violence and explain how they cause violence. Sadly, at the time of writing this chapter, there has been only limited progress in this area, probably because these studies are difficult to conduct and require more complex statistical analyses and study methods that can be difficult to set up. They also require face-to-face interviews with patients and cannot rely on existing datasets such as cross-sectional surveys and case registers. However, cross-sectional surveys can be a starting point to establish the direction of future study and whether symptoms apply differently to categorical diagnoses at the population level. For example, a meta-analysis of seven UK general population surveys measured psychotic symptoms of hypomania, thought insertion, paranoid ideation, strange experiences and hallucinations. It also created a categorical diagnosis of ‘psychosis’, using a cut-off to compare with other studies [Reference Coid, Ullrich, Bebbington, Fazel and Keers28]. Using the categorical construct, psychosis was not found to be associated with violence after controlling for confounding from demography and comorbid conditions such as ASPD, substance dependence and anxiety disorder. This is similar to findings from case register studies. Depressive disorder also showed no association after adjustments. However, one symptom, paranoid ideation, showed strong independent associations with more serious violence where a perpetrator or victim had been injured, repetitive violence, violence involving the police and where victims were more likely to be strangers. The other four symptoms showed no associations after adjustment including adjustment for other symptoms.
These findings appear supportive of the notion that paranoid ideation could cause violence but a cross-sectional survey cannot establish causation. The five symptoms are surprisingly common in the general population and do not necessarily mean a person reporting them is psychotic. What about in the case of established clinical psychotic illness? To study this, a first episode study of psychosis in East London, UK was used which measured psychosis using face-to-face, structured clinical interviews administered by psychiatrists and with questions to establish whether violence had occurred in the year before the interview [Reference Coid, Ullrich and Kallis29]. Most patients were psychotic at the time of the interview and many were in a psychiatric hospital in the first or second week of admission. They were also administered questionnaires to establish whether they were impulsive, had state or trait anger, and had psychopathic traits, and to test their reactions to a wide range of delusional beliefs and other symptoms established from the structured interview. Importantly, any patients who did not have psychotic symptoms at the time of the violence were excluded from the analyses. The study found a strong, independent relationship between delusions and violence in the year prior to first contact. This effect was greater for more serious violence. The association was not confounded by other psychotic symptoms, psychopathy or trait anger. The structured clinical interview included 32 possible delusions but only 6 were associated with angry affect: being spied upon, familiar people impersonated, persecution, conspiracy, threat/control override and misidentification. Most importantly, mediation analysis established that violence was dependent on whether the delusion made the patient angry.
The East London study findings were replicated in a re-analysis of the US MacArthur dataset, a prospective longitudinal study of violence among patients discharged from hospital and interviewed face-to-face at baseline before discharge and on five subsequent occasions in the community [Reference Ullrich, Keers and Coid30]. Nine of 15 delusions showed strong associations with violence, following adjustments, and included being spied upon, being followed, being plotted against, being able to hear others’ thoughts, being under the control of a person/force, thought insertion, strange forces working on them and having special gifts/powers. As with the East London study, being spied upon, being under external control and thought insertion were mediated by angry affect due to the delusions, suggesting a different, indirect pathway to serious violence. There was a direct pathway between certain symptoms and violence, but in these cases the violence was less serious.
A further UK study of patients discharged from medium-secure services to the community measured symptoms and violence at baseline (pre-discharge) and at 6 and 12 months in the community [Reference Coid, Kallis, Doyle, Shaw and Ullrich31]. The aim was to look at shifts in symptoms over time. The study found that an overall shift in positive symptoms was associated with violence. The larger the symptom shift, the more likely that violence would occur. Negative symptoms appeared to shift in the same direction as positive, corresponding to an overall increase in severity of illness. However, closer examination indicated that negative symptoms exerted protective effects. But there was no clinically observable effect because the protective effect of increasing negative symptoms was overwhelmed by the positive symptoms and, most importantly, the shift to increasing anger which accompanied the positive symptoms, particularly delusions. There was a relationship between stable paranoid delusions and violence but also between intensifying delusions accompanied by intensifying anger. Shifts and instability in the psychotic process were themselves causally associated with violence.
A final study in this series, which aimed to investigate causal links between symptoms and violence, included a prospective longitudinal study of prisoners released from prison and followed up in the community at a mean of 39 weeks later [Reference Keers, Ullrich, DeStavola and Coid32]. A subgroup had been diagnosed as suffering from schizophrenia, delusional disorder or drug-induced psychosis by researchers (but not necessarily the healthcare staff of the prison who were unaware of certain cases) prior to release. First examination of the data showed that prisoners diagnosed with schizophrenia did not have higher rates of violent behaviour than those with no mental disorder, including criminal reoffending once they returned to the community. However, when the data was re-examined to identify those who had not received any treatment for psychosis in prison, this subgroup were highly likely to become violent again. Untreated schizophrenia was associated with the emergence of persecutory delusions at follow-up, which were in turn associated with violence. Mediation analyses confirmed the effects of the persecutory delusions on the violence.
Using a causal approach in data analysis and concentration on symptoms rather than studying whether violence is associated with a diagnostic category resulted in new findings to guide future research. This approach corresponds to clinical experience and a forensic clinical assessment of psychosis and violence. Persecutory delusions appear to be the key symptoms, but these need to be accompanied by angry affect and/or anger for violence to occur. Although delusions were of prime importance, it is likely that other symptoms played a part. Although anxiety symptoms did not exert effects in the models in these studies, clinical experience shows that anxiety does have an effect in some cases, contributing to violence. The other aspect indicated by this work was that the intensity of the psychotic illness was of considerable importance, and also when symptoms were shifting or fluctuating, a key feature of an acute and severe episode of psychosis. It is also clear that prevention of relapse leading to further violence is dependent on maintaining anti-psychotic treatment and mental stability, and that the key preventative strategy is to avoid the re-occurrence of delusions associated with violence. The importance of associated anger with the delusions questions whether targeting anger as an associated affect should be the primary strategy for treatment intervention in future.
Violence Pathways
Forensic assessments of violence typically include two types of pathway analysis: firstly, an understanding of the life-course development of the individual from childhood to the violent incident or incidents under investigation, typically in adult life, together with examination of corresponding factors that may have had an impact and are known from research and experience to be strongly associated with future violence; and secondly, a painstaking forensic examination of the key components of the violent acts leading to a referral for a professional opinion. For example, this might be the prosecution case against the defendant in depositions and statements, or a series of worrying assaults on other patients and nurses by a patient detained in hospital, based on reading documented accounts, asking nurses for their account and interviewing the patient for their account and explanation. In clinical practice, opinions are usually presented in written form, with the recent pathway to the presenting events coming first and the lifetime understanding of the antecedents to the violence coming later in the report to establish links. It is usually necessary to set a starting timepoint and clarify the context of the assessment, such as who made the referral and why, the information available and the nature of the examination conducted to form an opinion. The life-course analysis is then used to support the opinion based on the recent violence and how this corresponds to or in some cases diverges from it.
A man has a history of life-long antisocial behaviour and repetitive involvement in violence, starting with childhood maltreatment in his family of origin and being taken into care, then childhood conduct disorder and persistent criminality in early adulthood, before developing schizophrenia in his mid-20s, subsequent refusal to cooperate with aftercare between episodes, frequent relapses, and a criminal history suggesting acquisitive offences such as theft and burglary together with assaults, where it is not always possible to be sure whether these are driven by the underlying antisocial personality or psychosis. However, it is apparent that some offences have been followed by hospital admission in an acute state of psychosis requiring treatment. Witness statements indicate that for some violent offences in public places, the individual has been acutely psychotic, but also intoxicated with both drugs and alcohol at the same time. He is currently charged with a serious wounding of another man in a bar with a beer glass where he got into an altercation due to his bizarre and provocative behaviour towards the victim. Other drinkers have given witness statements describing him as talking to himself, shouting at them and making threats of violence for no apparent reason.
Vignette 2
In a contrasting case, a man in his early 30s is charged with the attempted murder of his next-door neighbours. He has no previous convictions and had ceased working at a bank and become socially isolated over a one-year period. He had developed schizophrenia following the death of his mother 18 months earlier and has lived alone in the family home, unemployed but caring for himself, with no previous criminal convictions or contact with mental health services. He had recently made a complaint to the police regarding the behaviour of his neighbour which was found to have no basis in fact and no action had been taken. He had bought knives and an axe and had made a determined homicidal attack on his neighbour when the latter returned in the evening from work. He described an elaborate delusional system of persecution by his neighbour and his family, including the belief they had built a machine on behalf of the government, which was now causing damage to his internal body organs in a medical experiment. Police found detailed writings suggesting plans for the offence, but with multiple biblical references and scientifically unrelated research findings regarding experimentation on animals.
Using an actuarial measure of future risk, the first case will score higher on an actuarial measure of risk of future violence, leading to an expectation of prioritisation by services responsible for him. It can be argued that he has shown a lifetime of high risk of violence towards others. There is considerable scope for rejection of the first man from mental health services on the grounds he has ASPD and polysubstance abuse, and because experts are arguing over whether he was psychotic at the time of the latest episode of violence. However, experience demonstrates that many cases of schizophrenia with similar features can show considerable improvement with sustained pharmacological treatment over time, starting in a secure hospital setting, and continued medication, together with regular court-ordered follow-up in the community. In contrast, the second case shows a high risk of extreme violence towards others of a homicidal nature. Relapse of the illness in future and re-appearance of similar delusional beliefs (which cannot be accurately predicted) would render him a clear and immediate danger to persons in the local proximity. Both patients require long-term surveillance and monitoring for the safety of others. But for each, the risk assessment using a pathway model and future process of risk management are very different.
A Theoretical Model of Risk Pathway to Violence
A model that can be incorporated into clinical practice is based on empirical research and clinical experience [Reference Coid, Ullrich and Kallis33]. It is based on a longitudinal approach that aims to capture the evolution of risk over time, typically from when an offender is released from custody or a patient is released from hospital. This type of assessment might at first appear more useful for the first of the two examples given in the vignettes, both for the assessment of the latest criminal charge of violence and for the purpose of managing the risk of future violence, although it is equally applicable to the second. A typical actuarial risk assessment instrument using a score based on previous behaviours would suggest the first case is considerably more dangerous than the second, but this would be incorrect.
The clinical risk assessment using this model would proceed through each of the of the five stages shown in Figure 1.5. This would be based on previous behaviour and a full assessment of the individual’s previous history, including current circumstances and reason for the assessment, detailed assessment of previous and more recent violent and criminal behaviour, family history, and developmental history from childhood to the present day. Although Figure 1.5 shows that the first stage of the assessment is to make a diagnosis, most clinicians would correctly point out that this is usually completed towards the end of a clinical assessment. However, research has shown that pathways to violence and other offending are different according to different diagnoses in clinical forensic practice [Reference Coid, Yang and Ullrich34]. The model therefore differs from psychological assessments which do not always recognise the considerable differences in pathways determined by diagnosis and include diagnosis as one among multiple risk factors. (It is not recommended that forensic psychiatrists adhere to this simplistic approach. Clinical experience will soon reveal that different psychiatric conditions have very different pathways to violence.)
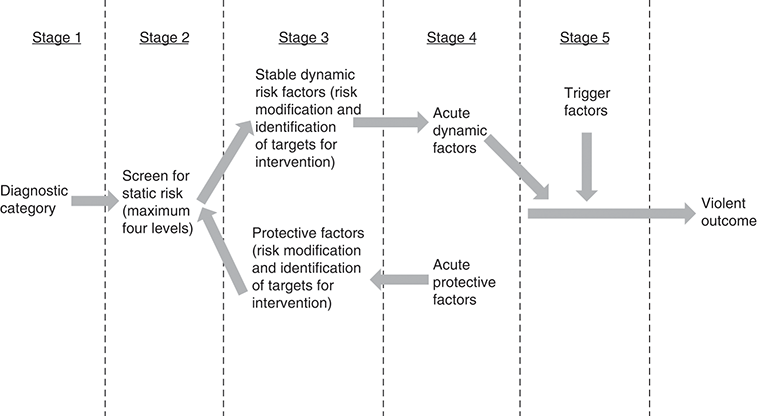
Figure 1.5 Theoretical model of risk pathway to violence.
The model is similar to a risk assessment in that it includes a series of stages in which risk factors could potentially be measured quantitatively using risk assessment instruments and was used in a research study to test the accuracy of these measures. However, that was not its primary intention, which was the formulation of a risk management plan or alternatively a retrospective analysis of an offence pathway according to the impact of exacerbating and protective factors over time. It would include assessment of current and previous mental state to obtain a formal diagnosis, and would include personality disorder and substance misuse, for example as in the first vignette, as well as schizophrenia. These further diagnoses would add to the complexity of the model. The figure also forms the basis of a risk formulation which follows from the full clinical assessment. If the patient is already known to services or if the forensic psychiatrist is approaching a case with a considerable body of knowledge and information available, this model may be particularly helpful.
Stage 1: Figure 1.5 begins with establishment of a psychiatric diagnosis at the outset together with (Stage 2) the level of static risk for future violence, based on actuarial measures. We have already referred to the considerable problems of the actuarial approach using static measures but believe they have some limited value as long as they are combined with an in-depth analysis of dynamic risk factors. A clinician may want to know a score for risk based on previous offending and this may be helpful in a more in-depth profiling of qualitative as well as quantitative aspects of previous offending. But it should not be the basis for major decisions such as release from hospital or prison. It is also of some help in indicating when an in-depth clinical assessment is required. It will be of little or no use in formulating a treatment plan. For the two case vignettes, it is the second which may concern many forensic psychiatrists most of all because of the risk of future homicidal violence towards others. However, when combined with dynamic factors, a static or actuarial measure of risk can provide a more clinically helpful assessment, which can then be used to formulate factors for risk management that will be targeted in a future intervention.
Stage 3 requires an assessment of ongoing dynamic risk factors. These are changeable and should be targets for future intervention if the aim is risk management or if they are identified as having an impact on the violent events in an assessment for court. An interaction can occur between dynamic risk and protective factors whereby the protective factors reduce risk or whereby risk is seen to increase when the protective factors are no longer present. Examples include alcoholism, mood disorder, moving into the vicinity of a group or class of previous victims, reducing the level of supervision by professionals and social support, refusal to take medication, and attitudes which condone violence or other hate crimes. There is debate over the extent to which dynamic risk factors can truly be considered causal factors for violence but can be considered as contributing to the violence to varying degrees and by different means. These have also been referred to as ‘criminogenic needs’ by psychologists with the theoretical question of whether the offence would have occurred if the ‘need’, or what had been lacking, had been redressed. Few of these factors are directly related to a violent act in terms of constituting an immediate, demonstrable cause. But they are nevertheless major contributing factors which make the violence more likely to occur.
In Stage 4, the individual may encounter acute dynamic risk factors that have a direct influence on subsequent behaviour; for example, acute intoxication, being involved at the time in a group or gang, sudden removal of social support, or sudden loss of a close relationship. These have a more immediate bearing in time on the violent outcome than ongoing or chronic risk factors. Descriptions of the effect of these factors by the patient or witness statements indicating change in behaviour or emotional presentation are important in formulating an assessment of causal effects on violence. For example, intoxication with alcohol could not be considered to have a direct, causal effect on violence. However, when combined with other factors such as provocation by the victim, intoxication may greatly increase the likelihood of a violent response through factors such as cognitive impairment, disinhibition and so on.
At Stage 5, certain trigger factors which have an immediate and causal effect on the violent outcome may be encountered. These are very common in reactive, impulsive acts. Alternatively, the violence may have been planned for some time, although a sudden triggering factor can sometimes occur in cases where planning may have been present and determine the time and place when the violence occurred. Trigger factors are factors which, like the trigger on a gun, cause something to happen and can be an event or situation that causes something to start – in this case, a violent retaliation. The key definition which distinguishes a trigger from a dynamic risk factor is the timing of the event in terms of its occurrence before the violence and the direct relationship between the trigger and the violent act. There should be a very short period before the occurrence of a triggering factor and the violent act, where anything more than 1 hour is likely to be considered as occurring after a ‘cooling-off’ period in a court and would strongly suggest planning. Research with recidivists indicates that the majority are highly impulsive and do not consider or plan their next behaviour any more than 15 minutes before the criminal act [Reference Zamble and Quinsey35].
A study proposed that trigger factors exist that could be considered ‘super-acute’ risk factors that have an immediate, moment-to-moment impact in precipitating a violent incident [Reference Freestone, Ullrich and Coid36]. These are best referred to as ‘situational variables’ and conceptualised as external environmental effects that have an immediate effect on the appraisal of a situation. They correspond to reactive aggression in response to frustration or threat and are unlikely to be present in most cases of instrumental aggression, where there is more likely to be forethought or planning before the aggressive act. In this study of violent prisoners, external triggers were found to be random events that could not be predicted by either static or dynamic risk factors but were linked to specific psychological characteristics of the violent offender, for example features of their personality disorder. The personality features rendered the individual more likely to respond violently to the trigger, but the causal factor was the trigger itself.
There should not be any confusion between triggers and the dynamic risk factors which are incorrectly defined as ‘triggers’ in a Scandinavian case register study [Reference Sariaslan, Lichentstein, Larsson and Fazel37]. These included exposure to violence, parental bereavement, self-harm, traumatic brain injury, unintentional injuries and substance intoxication in the week before the violent act rather than on the day of the act, which excludes them as trigger factors. Immediate retaliation to an assault or becoming involved to help a friend being assaulted may be triggers if occurring very close to the violence, but it is unclear how self-harm and death of a parent can trigger violence if it occurred up to a week before. These did not appear to be credible or sufficient ‘triggers’ in themselves to result in violence. Forensic psychiatrists will not fare well when giving evidence in court if they attempt to mitigate previous violent behaviour as a ‘causal’ factor for violence and even less so for a bout of intoxication. These findings would be best described as dynamic factors that increased risk for a subsequent violent act rather than a ‘trigger’.
Violence: Impulsive/Reactive and Targeted/Predatory Dichotomy
The model in Figure 1.5 does not take into account specific qualities of the violent action being assessed. Aggression is complex and heterogeneous, which often explains the limitations of both epidemiological studies which have minimal data to differentiate between different types and biological studies which combine more than one type. There are different typologies and a single individual can show different types at different times. However, a longstanding system for codifying aggression is the impulsive/reactive and targeted/predatory (the latter including instrumental aggression) dichotomy, with differing pathways. The two cases of schizophrenia described in the vignettes will fit into differing categories using this dichotomy. With experience, however, trainees will find that violent acts will sometimes fit into both categories. Nevertheless, being aware of this dichotomy is useful; firstly, because it is thought there may be different underlying neurobiology which explains these pathways [Reference Rosell and Siever38]; secondly, a full understanding of the different components of each give a more nuanced picture of the patient’s diagnosis and the links to their behaviour and will help formulate a treatment plan; and thirdly, because it has been used for the development of threat assessments for future harm reduction.
Impulsive/reactive aggression is driven by internal emotion, it tends to be reactive, the violence is likely to be immediate, it is likely to be triggered by an external event which occurs only a short time before the violent act (typically minutes or seconds), and it is carried out against perceived threats where the goal is threat reduction, primarily defensive, aiming for rapid displacement of the violence with the reaction being time-limited.
In contrast, targeted/predatory aggression is less reactive and emotional, it is planned and purposeful, it is thought out in advance (often with a decision made well before the violent act), it has a specific target, it is carried out to achieve a goal or goals, it is cognitive and attack orientated, and it is not time-limited. Targeted violence is rarely impulsive or random and most individuals think through and plan out the violence so that it is much easier to discern and follow a ‘pathway’ to the violent act. Figure 1.6 shows a US Homeland Security Pathway stepwise model which applies to the targeted/predatory pathway and was developed from experience with mass killings in the USA with the aim of disrupting or getting potential offenders off the pathway to violence [Reference Calhoun and Weston39, 40]. Features of this model can be considered within forensic assessments and apply equally to psychotic offenders as to those with no mental disorder. Most steps of the model apply to the second case of schizophrenia described in the vignettes.
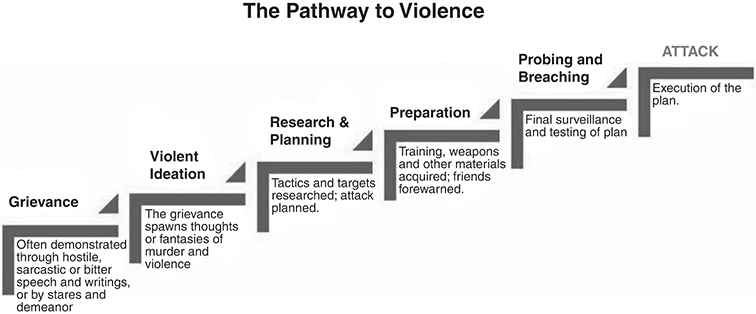
There can be multiple reasons for an individual embarking on the pathway; for example, a grievance due to problems needing to be solved, drawing attention to a cause, personal pain and anguish, an unresolved or unresolvable grievance, paranoid delusions, no longer wanting to live, and so on. In studies carried out after mass killings, most perpetrators were actively suicidal or at a point of desperation prior to their attacks. Figure 1.6 shows how the grievance progresses from violent ideation to research and planning followed by subsequent preparation, including access to weapons and other equipment needed for the attack. The preparation stage is often short before the person engages in violence. In terms of prevention, the first question is whether it is possible to identify that a person is on a pathway to violence. Secondly, and if so, how far down the pathway are they in terms of idea, plan, preparation or implementation? Thirdly, why are they on the pathway and resorting to violence? And fourthly, is it possible to divert them to a better path?
Retrospective observations show a change in identification behaviour, such as joining right-wing or other terrorist organisations, but also what enforcement agencies refer to as ‘emotional leakage’, with many actually stating that they will do it or posting threats in some form online in over 60% cases. Less than 20% directly threaten victims in mass killings, but in many cases of violence in psychosis the victim may have been threatened or even been a victim of violence on a previous occasion, particularly relatives. Probing and breaching includes ‘try-outs’ of the eventual violent act, sometimes with visits to the planned location. Try-outs are also a particular component of serious sex offences when there is a sadistic motive [Reference MacCulloch, Snowden, Wood and Mills41] and where this may be the only overt indicator of the future behaviour, which is otherwise concealed within an undisclosed sadistic fantasy. There may also be examples of ‘short-term’ behaviour such as closing bank accounts or ominous texts of farewell to close persons. There are occasional last-resort warnings, but the perpetrator may no longer expect this to have any effect. The timing of an attack may be brought forward when it is thought that the victim may no longer be in the location or soon inaccessible. In psychotic patients, increasing symptoms such as hostility and anger, threat perception, grandiosity and dysphoria may be seen in cases where there has been treatment non-adherence.
Criminal Records – Criminal Careers
A criminal career has a beginning (onset), an end (desistence) and a career length in between (duration) [Reference Farrington42]. Criminal records are essential for a forensic assessment of violence and may reveal multiple pathways. It is important to go through a criminal record with the offender during an assessment, particularly when alternative sources of information are unavailable. Typically, convictions represent only a fraction of the offences committed by an offender and better research in the field includes self-report data, so it is important to ask the patient about other violent events over the lifespan. Individual offenders tend to commit offences at a fairly constant frequency during their criminal careers. However, those first convicted at a young age have more prolonged careers. Furthermore, when looking at an entire population, a minority account for the majority of all offences. Violent offenders tend not to be specialist offenders in most studies, although these will sometimes be encountered in clinical forensic practice where it is important to understand similarities between individual incidents. Sex offenders tend to be most specialised and fraud offenders most persistent. Most offenders will commit a single offence and not be reconvicted. However, some will be persistent and a subgroup will be chronic offenders.
Chronic offenders are more likely to have histories of maltreatment in childhood and come from families where a member also has a criminal history. Debut offence is important and those who commit a robbery are more likely to go on to commit serious offences such as violence and become chronic offenders. Late-onset offenders after the age of 18 years tend to have been more anxious in childhood with fewer social contacts and with a proportion showing evidence of social decline leading to criminality from alcohol dependence and after developing severe mental illness. Previous studies of these groups in childhood and adolescence showed that childhood-onset delinquents had inadequate parenting, neurocognitive problems, under-controlled temperament, severe hyperactivity, psychopathic personality traits and violent behaviour. Adolescent-onset delinquents were not distinguished by these features.
A New Zealand cohort followed to age 26 years showed that the childhood-onset delinquents were the most elevated on psychopathic personality traits, mental health problems, substance dependence, numbers of children, financial problems, work problems, and drug-related and violent crime, including violence against women and children [Reference Moffitt, Caspi, Harrington and Milne43]. The adolescent-onset delinquents at 26 years were less extreme but elevated on impulsive personality traits, mental health problems, substance dependence, financial problems and property offences. A third group of men who had been aggressive as children but not very delinquent as adolescents emerged as low-level chronic offenders who were anxious, depressed and socially isolated, and had financial and work problems. These findings support the theory of life-course-persistent and adolescence-limited antisocial behaviour among offenders, but also extend it to include other groups.
The first vignette earlier is clearly a case of an early-onset offender and delinquency preceded the development of schizophrenia. Because there are important additional components to early-onset cases which will impact on other psychopathology and behaviour, including behaviour in security while undergoing treatment and after return to the community, it is recommended that when carrying out a forensic assessment this should routinely include assessment for the presence or absence of ASPD using the US Diagnostic and Statistical Manual. This requires three or more criteria to be present before the age of 15 years and three or more after the age of 15 years (see criteria in box). It is generally the case that the earlier the onset, the more severe and persistent the condition. Forensic psychiatrists should not be confused by criterion D which specifies that ASPD should not occur in the context of schizophrenia or conduct disorder. In forensic practice many patients will have comorbid ASPD with a psychotic illness – although it will be necessary to disentangle whether the criminal behaviour being assessed was due to the psychosis or ASPD, which is not always straightforward.
A. Disregard for and violation of others’ rights since age 15, as indicated by one of the seven sub features:
1. Failure to obey laws and norms by engaging in behavior which results in criminal arrest, or would warrant criminal arrest
2. Lying, deception, and manipulation, for profit or self-amusement
3. Impulsive behavior
4. Irritability and aggression, manifested as frequently assaults others, or engages in fighting
5. Blatantly disregards safety of self and others
6. A pattern of irresponsibility
7. Lack of remorse for actions (American Psychiatric Association, 2013)
The other diagnostic criteria are:
B. The person is at least age 18
C. Conduct disorder was present by history before age 15
D. The antisocial behavior does not occur in the context of schizophrenia or bipolar disorder (American Psychiatric Association, 2013)
Conduct Disorder 312.8x (F91.x)
1. A repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated, as manifested by the presence of at least three of the following 15 criteria in the past 12 months from any of the categories below, with at least one criterion present in the past 6 months:
Aggression to People and Animals
1. Often bullies, threatens, or intimidates others.
2. Often initiates physical fights.
3. Has used a weapon that can cause serious physical harm to others (e.g., a bat, brick, broken bottle, knife, gun).
4. Has been physically cruel to people.
5. Has been physically cruel to animals.
6. Has stolen while confronting a victim (e.g., mugging, purse snatching, extortion, armed robbery).
7. Has forced someone into sexual activity.
Destruction of Property
8. Has deliberately engaged in fire setting with the intention of causing serious damage.
9. Has deliberately destroyed others’ property (other than by fire setting).
Deceitfulness or Theft
10. Has broken into someone else’s house, building, or car.
11. Often lies to obtain goods or favours or to avoid obligations (i.e., ‘cons’ others).
12. Has stolen items of nontrivial value without confronting a victim (e.g., shoplifting, but without breaking and entering; forgery).
Serious Violations of Rules
13. Often stays out at night despite parental prohibitions, beginning before age 13 years.
14. Has run away from home overnight at least twice while living in the parental or parental surrogate home, or once without returning for a lengthy period.
15. Is often truant from school, beginning before age 13 years.
2. The disturbance in behaviour causes clinically significant impairment in social, academic, or occupational functioning.
3. If the individual is age 18 years or older, criteria are not met for antisocial personality disorder.
Specify whether:
312.81 (F91.1) Childhood-onset type: Individuals show at least one symptom characteristic of conduct disorder prior to age 10 years.
312.82 (F91.2) Adolescent-onset type: Individuals show no symptom characteristic of conduct disorder prior to age 10 years.
312.89 (F91.9) Unspecified onset: Criteria for a diagnosis of conduct disorder are met, but there is not enough information available to determine whether the onset of the first symptom was before or after age 10 years.
Moffitt proposed that delinquency conceals two distinct categories of individuals, each with a unique natural history and aetiology: a small group engages in antisocial behaviour at every life stage, whereas a larger group is antisocial only during adolescence. According to the theory of life-course-persistent antisocial behaviour, children’s neuropsychological problems interact cumulatively with their criminogenic environments across development, culminating in a pathological personality. According to the theory of adolescence-limited antisocial behaviour, a contemporary maturity gap encourages teens to mimic antisocial behaviour in ways that are normative and adjustive, although this group will mature out of the behaviour by adulthood [Reference Moffitt44].
The appearance of a series of violent offences occurring in later life is unusual and should prompt investigation of the onset of psychiatric morbidity as a causal factor. Heavy use of alcohol is the most common factor associated with late onset, but this group is also associated with more forms of ill-health and hospitalisations [Reference Skinner, Farrington and Shepherd45]. However, it can be seen that the second vignette earlier fits this category. Experience will reveal that a proportion of patients with psychotic illness begin to show recorded criminal offences for the first time following development of a psychotic illness, sometimes with re-admissions to hospital following arrests by the police, and coinciding with re-appearance of symptoms due to failure to take medication and accept follow-up in the community. Hodgins proposed that among violent offenders with schizophrenia, there are three distinct types defined by the age of onset of antisocial and violent behaviour [Reference Hodgins46]. The early starters display a pattern of antisocial behaviour that emerges in childhood or early adolescence, well before illness onset, which remains stable across the lifespan. The largest group of violent offenders with schizophrenia show no antisocial behaviour prior to the onset of the illness and then repeatedly engage in aggressive behaviour towards others. A small group of individuals who display a chronic course of schizophrenia show no aggressive behaviour for one or two decades after illness onset and then engage in serious violence towards, often killing, those who care for them. This typology, while not fitting all cases encountered in forensic practice, does correspond to many a trainee will encounter in the future.
Drug and Alcohol Misuse
The associations between alcohol and drug misuse and violence are probably the most complex on which to give an opinion in forensic assessments. This chapter has explained why current research into the relationship between psychosis and substance misuse has been unhelpful and misleading. It has also suggested a new approach to the study of symptoms of psychosis and violence. However, in the latter, there has been no investigation of the effects of substances on symptoms leading to violence and this will be important in future research. It is therefore important to look at previous research findings and see to what extent these can guide a forensic assessment. Forensic psychiatrists will frequently be required to decide whether substances were relevant to violent behaviour and should be well acquainted with criminal law in relation to intoxication.
White [Reference White, Stoff, Breiling and Maser47] describes three basic explanatory models for the relationship between alcohol/drug use and violence: (a) substance use causes violence; (b) violence leads to substance use: (c) it is spurious, or coincidental, being explained by a set of common causes. These need to be considered when evaluating epidemiological research findings, but also when considering individual cases in a forensic assessment.
Causal Relationships
There is more than one causal model. The first is due to psychopharmacological properties of intoxication which can include disinhibition, cognitive-perceptual distortions, attention deficits, bad judgement and neurochemical changes. In addition, chronic intoxication may result in withdrawal, sleep deprivation, impairment of neuropsychological functioning or exacerbation of personality disorders, including borderline personality disorder leading to violence.
The second model is economic motivation to obtain income to buy drugs, typically robbery. The third systemic model argues that a system of drug distribution and use is inherently connected with violence. This includes violence for territory where drug sales take place, particularly involving street gangs, enforcing rules, punishments for non-payment of debts, arguments during transactions, robberies from drug dealers or buyers, and where dissatisfied parties cannot go to the police or courts to resolve disagreements. A key public health consideration is that drug markets can create community disorganisation, which in turn affects the behaviour of others in the community and increases violence among many other persons.
A final model is that drug and alcohol misuse are part of a causal pathway leading to violence which is mediated by symptoms of mental disorder. For example, persons with schizophrenia who abuse drugs such as stimulants, hallucinogens and cannabis can relapse into an acute psychotic episode or their symptoms may be exacerbated, leading to violent behaviour. Similarly, patients who chronically abuse drugs and alcohol may fail to take medication, leading to relapse. However, it is the symptoms of psychosis that have a direct causal effect on the violence and not the drugs or alcohol, and where the latter may not be directly and immediately relevant at the time of the violence. However, if both symptoms which had a causal relationship with violence are present at the same time as intoxication, it can be difficult to disentangle the effects of each separately. In most cases, it may be possible to differentiate the symptoms as having a causal effect and the substances as further disinhibiting behaviour driven by symptoms or exacerbating the symptoms. However, it is important to be aware of the law regarding intoxication. Voluntary intoxication leading to exacerbation of symptoms which in turn leads to violence may not convince a court that there is a defence against conviction, despite clear evidence of symptoms, for example R v Quick in a defence of insanity.
Forensic psychiatrists will occasionally be asked to give an opinion as to whether an individual showed an abnormal violent reaction to a prescribed drug when there have been similar adverse drug reports. These cases are best argued in court together with an expert in psychopharmacology. It is important to be aware that the relationship may not be causal and that evidence may be produced to attribute a motive and to challenge evidence in court, requiring a careful assessment of the circumstances and the individual’s history. However, factors indicative of an adverse reaction include cases when there appear to be more reports than would be expected for a particular drug considering the number of prescriptions in the populations (proportional reporting ratio), unusual demographics (older and female), early onset of psychiatric symptoms (usually within a few days), a senseless act of aggression/violence directed at anyone who happened to be nearby, and resolution of the symptoms upon discontinuation of the drug.
Violence Leads to Substance Misuse
Individuals who are aggressive are more likely to become involved in situations and subcultures in which drug and alcohol use are encouraged. This can include a professional criminal lifestyle. Aggressive individuals are also more likely to use drugs to self-medicate, for example cannabis to make violence less likely and to calm themselves. However, it can also be used to give individuals an excuse or courage to act aggressively.
Spurious Relationship
Substance use and violence are related coincidentally because they share common causes, for example genetic or temperamental traits and ASPD, and consequently there is no causal relationship. White [Reference White, Stoff, Breiling and Maser47] describes the ‘routine activities’ perspective where violence occurs most often when and where people are drinking, particularly in certain bars where social controls are weakened. Similarly, it can occur in subcultures where violence and heavy drinking are considered proof of masculinity, which would spuriously inflate the relationship and where situational factors increase violence risk.
A spurious relationship needs to be considered in certain epidemiological studies of violence which assert that conditions such as schizophrenia do not cause violence and that the association is due to substance misuse. This is a common conclusion using case registers and some surveys where drug misuse is recorded in case files or a comorbid diagnostic category of drug misuse disorder is recorded as well as a diagnosis of schizophrenia. In some studies, statistical adjustments are then made for the substance misuse disorder and the odds of association with schizophrenia are then attenuated, leading to the conclusion that the association was confounded. However, unless it can be established when the drugs had been used and whether this coincided with the violence, and also whether symptoms had been present at the material time, these conclusions cannot be drawn. Taking the case of the first vignette earlier with a comorbid diagnosis of ASPD, it is likely that many violent events, probably the majority over the patient’s life course, had occurred at times when the patient was not psychotic. However, that does not necessarily mean that psychotic symptoms had never had a direct causal effect on the patient’s violence. Because of downwards social drift and because schizophrenia is more common among the poor, persons with schizophrenia often reside in communities with high levels of crime and drug misuse, where violence is more common, and as a result of their illness they also misuse drugs which are more freely available to them in these areas.