EDITOR:
A challenge in the management of patients undergoing major limb amputations is to provide adequate pain management in the immediate post-trauma and postoperative period [Reference Halbert, Crotty and Cameron1]. After amputation, re-operation is common. Performing a peripheral nerve block on an amputated limb may be difficult because conventional end-points (distal muscle contraction upon electrical nerve stimulation or eliciting paraesthesia) may not be possible. Ultrasonography may facilitate the performance of continuous peripheral nerve blocks in amputee patients and broaden the indications for nerve blocks. We present our experience with ultrasound-guided continuous peripheral nerve blocks in a heterogeneous group of amputee patients, in whom other pain relieving techniques failed or were refused.
Institutional Research Ethics Board approved this study. Eleven ASA I–IV patients who had undergone a traumatic or an operative amputation and in whom a continuous peripheral nerve block for perioperative pain relief was performed were studied. Before the block procedure, visual analogue pain scores (VAS) were noted.
In each case, a 20-G polyamide catheter was placed through an 18-G Contiplex D needle (B. Braun, Melsungen, Germany) using ultrasound guidance with a linear 7–13 MHz ultrasound transducer (Micromaxx, Sonosite Inc., Bothell, WA, USA). In some patients a single injection peripheral nerve block was added. The continuous femoral and sciatic blocks and one brachial plexus block were performed as described by Swenson and colleagues [Reference Swenson, Bay and Loose2]. For the initial bolus injection through the needle 0.3 mL kg−1 ropivacaine 0.75% was used. In order to verify correct catheter placement, an additional injection with 0.1 mL kg−1 ropivacaine 0.75% through the catheter was performed.
The patients who underwent a planned (re)amputation of the limb received general anaesthesia. Multimodal pain therapy including continuous infusion of s-ketamine 5 mg h−1 and morphine 0.1 mg kg−1 at the end of surgery was prescribed. In the post-anaesthesia care unit, paracetamol 15 mg kg−1 and diclofenac 1 mg kg−1 were administered intravenously. According to our hospital’s postoperative pain protocol, on all catheters bupivacaine 0.25% was infused at a rate of 0.1 mL kg−1 h−1 with a maximum of 6 mL h−1. If two catheters were used, the concentration bupivacaine was decreased to 0.125%. The catheters were left in situ for a maximum of 5 days. One hour after the block procedure or awaking from anaesthesia, the pain was evaluated using visual analogue scales. The patients who underwent the block procedure after the amputation were also asked whether heaviness, numbness or paresis of the non-existing limb were experienced before and after the block. Once daily, all patients were visited to record pain scores and whether they were satisfied with the postoperative pain relief (0 = very unsatisfied, 10 = absolutely satisfied).
In five patients, blocks were performed preoperatively (pre-group) and in six postoperatively (post-group). Patient characteristics were similar between the two groups. The pain and satisfaction scores are described in Table 1.
Table 1 Preoperative performed continuous peripheral nerve blocks: pain scores before and after the block procedure and satisfaction scores.
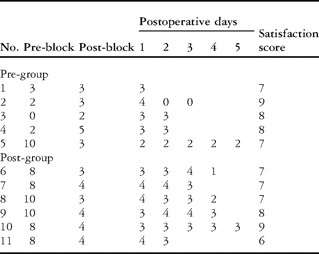
In the pre-group, three patients suffered from mild chronic pain before surgery. One patient suffered from severe chronic pain due to an exacerbation of a chronic infection of the amputation stump. After performance of the block and surgery, the preoperative pain scores decreased in this patient. In the others, pain scores remained unchanged or increased slightly. One of the patients in this group reported altered perceptions in the non-existing extremity after the nerve block. In the post-group, all patients suffered from severe acute and phantom pain. Intravenous analgesia had failed to provide adequate pain relief after amputation. After performance of the blocks, pain scores decreased and were acceptable to all patients. Four of these patients reported altered perceptions or paresis in the non-existing extremity after the block. Overall, all patients reported excellent patient satisfaction scores.
Ultrasonography facilitated the performance of peripheral nerve block procedures in patients in whom other nerve localizing techniques would have been difficult to apply. Nerve localization and eliciting a distal motor response with a peripheral-nerve stimulator for demonstration of correct needle placement was impossible. Although not in the conventional way, the nerve stimulator may be used to block phantom extremities [Reference Klein, Eck, Nielsen and Steele3].
There is little evidence for clear recommendations to guide clinicians how to treat acute pain and to prevent chronic pain after amputation.1 Risk factors for long-term post-surgical pain are pre-amputation pain, lower limb amputation and intensity of acute postoperative pain [Reference Hanley, Jensen, Smith, Ehde, Edwards and Robinson4,Reference Nikolajsen, Ilkjaer, Krøner, Christensen and Jensen5].
After treatment with intravenous or epidural patient-controlled analgesia, the incidence of severe pain is still 7.8% and 10.4%, respectively [Reference Dolin, Cashman and Bland6]. Continuous peripheral nerve blocks may fail in 1.1% [Reference Swenson, Bay and Loose2]. Moreover, epidural analgesia may not be used due to contraindications or patient refusal. For these reasons, we used these blocks for the patients in the pre-group. In the post-group, ultrasound-guided blocks were used because intravenous analgesia was not sufficient for providing adequate pain relief after amputation and epidural analgesia was contraindicated. Phantom sensations are experienced by almost everyone who has undergone a limb amputation and may fade over time [Reference Kooijman, Dijkstra, Geertzen, Elzinga and van der Schans7]. Although this subjective phenomenon may be used for evaluating block success in amputee patients, not all patients will experience altered phantom sensations after successful nerve blocks.
We conclude that ultrasonography facilitated the performance of successful peripheral nerve blocks in amputee patients in whom other pain relieving techniques failed or where contraindicated. The use of ultrasonography broadens the applicability of peripheral nerve blocks in these patients.





