Introduction
Aboriginal and Torres Strait Islander knowledge and wisdom has long recognised the role of social and cultural factors on health and well-being (Bartlett & Boffa, Reference Bartlett and Boffa2001). Aboriginal and Torres Strait Islander holistic health philosophy describes social and emotional well-being as the interconnection of social emotional, spiritual, cultural factors on health and wellness of not just individuals but communities (NAHSWP, 1989). Social and emotional well-being as conceptualised by Gee et al. (Dudgeon et al., Reference Dudgeon, Milroy and Walker2014) recognises the ongoing influence of historical, political and social factors on health and social outcomes (Swan & Raphael, Reference Swan, Raphael, Swan and Raphael1995; Raphael & Swan, Reference Raphael and Swan1997; Dudgeon et al., Reference Dudgeon, Milroy and Walker2014; Paradies et al., Reference Paradies, Ben, Denson, Elias, Priest, Pieterse, Gupta, Kelaher and Gee2015). These social factors (employment, education, housing, income and transport) are internationally described and recognised as the social determinants of health and are estimated to contribute to 34% of the overall burden of disease experienced by Aboriginal and Torres Strait Islander people (ABS, 2013). Both internationally and cross-culturally peer-reviewed literature has established associations, explored pathways and biological mechanisms providing a critical knowledge base on the role of social factors on health (Braveman et al., Reference Braveman, Egerter and Williams2011). Despite these understandings, there is limited evidence on effective intervention strategies that address how these social factors influence health outcomes within the population (Bambra et al., Reference Bambra, Gibson, Sowden, Wright, Whitehead and Petticrew2010; Thornton et al., Reference Thornton, Glover, Cené, Glik, Henderson and Williams2016; Alegría et al., Reference Alegría, NeMoyer, Falgàs Bagué, Wang and Alvarez2018; Luchenski et al., Reference Luchenski, Maguire, Aldridge, Hayward, Story, Perri, Withers, Clint, Fitzpatrick and Hewett2018).
Recent government consultations highlight the importance of self-determined and timely action on the social determinants of health for Aboriginal and Torres Strait Islander communities incorporating system responses that are coordinated, culturally relevant and strengths-based (Andermann, Reference Andermann2016; Commonwealth of Australia, 2017; Frier et al., Reference Frier, Devine, Barnett and Dunning2020; Osborne et al., Reference Osborne, Baum and Brown2013). Health systems face challenges in responding to the complex nature of the social determinants of health with collaborations required across health and social services; nonetheless, the clinical frontline workforce have been recognised as a potential catalyst for change in any systems response (Andermann, Reference Andermann2016). Clinical workforce approaches that include screening clients for social and emotional well-being (which include the social determinants of health) facilitate the early identification and management of needs, planned and coordinated responses and the monitoring of progress and outcomes (Langham et al., Reference Langham, McCalman, Matthews, Bainbridge, Nattabi, Kinchin and Bailie2017).
In a current context, Aboriginal Community Controlled Health Services (ACCHOs) and primary health care services are ‘doing whatever it takes’ to meet the social and emotional well-being needs of Aboriginal and Torres Strait Islander people which includes addressing the social determinants of health in service delivery (CREATE, 2020). Consultations with ACCHOs have highlighted key principles which inform holistic approaches to the social determinants of health including self-determination, accessible and culturally safe care and strong partnerships that support clients to navigate social services (CREATE, 2020). A recent document analysis of 67 ACCHO annual reports found that all services were working to improve clients’ intermediary social determinants of health, specifically material circumstances, biological, behavioural and psychosocial factors (Pearson et al., Reference Pearson, Schwartzkopff, Dawson, Hagger, Karagi, Davy, Brown and Braunack-Mayer2020). Whilst structured and funded Aboriginal and Torres Strait Islander health assessments for preventative care are widely implemented, these assessments are limited by a biomedical focus that inadequately addresses social and cultural factors (Bailie et al., Reference Bailie, Laycock, Matthews, Peiris and Bailie2019). Across organisations there are varied responses depending on the capacity (i.e. workforce, skills, training and resources) of the primary health care service (CREATE, 2020; Andermann, Reference Andermann2018). Furthermore, service delivery protocols for addressing the social determinants of health and more broadly data systems for monitoring their actions are not well established (Golembiewski et al., Reference Golembiewski, Allen, Blackmon, Hinrichs and Vest2019; Osborne et al., Reference Osborne, Baum and Brown2013).
Strengths-based, person centred and empowerment approaches are often used synonymously to describe the delivery of health care for Aboriginal and Torres Strait Islander people. These approaches promote individuals control over their own lives and focus on abilities and resources to enable self-determination (Bovill et al., Reference Bovill, Chamberlain, Bar-Zeev, Gruppetta and Gould2019; Gibson et al., Reference Gibson, Chatfeild, O’Neill-Baker, Newman and Steele2020; Saleebey, Reference Saleebey1996). Aboriginal and Torres Strait Islander people who have increased control and mastery over their lived experiences are empowered in their engagement with social and health services (Tsey et al., Reference Tsey, Whiteside, Haswell-Elkins, Bainbridge, Cadet-James and Wilson2010). Health care services commonly describe intentions to deliver strengths-based approaches, yet the practical and genuine implementation with Aboriginal and Torres Strait Islander people is still emerging in practice (Askew et al., Reference Askew, Brady, Mukandi, Singh, Sinha, Brough and Bond2020; Gibson et al., Reference Gibson, Chatfeild, O’Neill-Baker, Newman and Steele2020). Holistic case management models are well suited for strengths-based practice which focuses on empowering people to take charge of their own lives and to support the identification of existing strengths and resources (Saleebey, Reference Saleebey1996). Case management approaches whilst diverse across disciplines and in different contexts usually include the following core functions; assessment, planning, linking, monitoring, advocacy and outreach services (Huber, Reference Huber2002). Case management approaches in primary health care with Aboriginal and Torres Strait Islander people report improvements in self-rated health status, reduction in depression and improved measures of diabetes control (Askew et al., Reference Askew, Togni, Schluter, Rogers, Egert, Potter, Hayman, Cass and Brown2015). These findings suggest that patient-led case management has the potential to enhance holistic approaches to social and emotional well-being (Askew et al., Reference Askew, Togni, Schluter, Rogers, Egert, Potter, Hayman, Cass and Brown2015).
The effects of colonisation and the continuing social and political oppression and dispossession of Aboriginal and Torres Strait Islander communities have contributed to significant socio-economic and health inequities (Gracey & King, Reference Gracey and King2009). Persistent and disproportionate inequalities experienced by Aboriginal and Torres Strait Islander people highlight the need to better understand and respond to social and emotional well-being needs which includes the social determinants of health. There is a pressing need for coordinated best practice responses to social and emotional well-being screening and management, dedicated resources, training and ongoing monitoring (Langham et al., Reference Langham, McCalman, Matthews, Bainbridge, Nattabi, Kinchin and Bailie2017). Existing evidence has not yet described approaches that collectively inform health care responses for Aboriginal and Torres Strait Islander social and emotional well-being. To address this gap, a pilot program has been designed within a research setting and includes the following key elements: i) identifying unmet needs, ii) strengths-based case management, iii) document and monitoring, iv) culturally relevant supervision and v) evaluation. The aim of this manuscript is to describe and critically explore the program’s key elements from an Aboriginal and Torres Strait Islander perspective as part of strengthening practice-based evidence on social and emotional well-being.
Discussion
Program context
The Cultural Pathways program is implemented by Wardliparingga Aboriginal Health Equity research team in the South Australian Health and Medical Research Institute, Adelaide, South Australia. Wardliparingga undertakes research that is of relevance to South Australian Aboriginal and Torres Strait Islander communities through partnerships, collaboration, respect, reciprocity and for the benefit of community (SAHMRI, 2014). The Cultural Pathways Program is designed and implemented by Aboriginal and Torres Strait Islander people as a response to community identified needs. The program is implemented within an Indigenous methodological framework and from inception to implementation the program has been underpinned by Aboriginal and Torres Strait Islander ways of knowing, being and doing (Rigney, Reference Rigney1999; Martin & Mirraboopa, Reference Martin and Mirraboopa2003; Saunders et al., Reference Saunders, West and Usher2010; Wilson, Reference Wilson2011; Smith, Reference Smith2012). Priority areas for research were established through extensive consultation and engagement with the community (King & Brown, Reference King and Brown2015). All programs of work implemented by Wardliparingga have Aboriginal and Torres Strait Islander leadership and governance, through these structures the community consistently highlighted that more holistic responses, which included the social determinants of health, were required. The research team is predominantly Aboriginal and Torres Strait Islander researchers who bring wisdom and experience to the development of the program approach and implementation ensuring consistent alignment with Aboriginal and Torres Strait Islander ways of knowing, being and doing. The program described in this manuscript was approved by the Aboriginal Health Research Ethics Committee of South Australia (AHREC-04-17-733).
The program approach includes comprehensive screening utilising a specifically developed holistic screening tool to identify unmet social and emotional well-being needs. Following screening, facilitators implement strengths-based case management through goal setting, prioritisation and brokering connections to services. program structures embed documentation and monitoring of the program’s social and emotional well-being responses, actions taken to address needs and outcomes for participants. These elements are underpinned by culturally relevant supervision, reflective practice and evaluation. The program approach critically explores the benefits, cultural relevance and responsiveness of common practices in case management. Through a combined understanding of these approaches, the program seeks to inform the evidence base for strengthened and coordinated responses to Aboriginal and Torres Strait Islander social and emotional well-being.
Program delivery is undertaken by male and female facilitators with workforce roles informed by a navigator approach, to assist individuals’ engagement with the health care system and to overcome any barriers to care (Bernardes et al., Reference Bernardes, Martin, Cole, Kitchener, Cowburn, Garvey, Walpole and Valery2018; Henderson & Kendall, Reference Henderson and Kendall2011; Whop et al., Reference Whop, Valery, Beesley, Moore, Lokuge, Jacka and Garvey2012). Referrals are received from a large-scale population-based biomedical cohort study of Aboriginal and Torres Strait Islander South Australians. As part of the study, all participants receive a comprehensive health assessment that includes questions regarding their social and emotional well-being. Further to this, community engagement and consultations highlighted that post-study follow-up responses for participants would require addressing social and emotional well-being needs such as psychosocial health, financial literacy, food security and material circumstances. Participants are offered a referral to the Cultural Pathways Program, if unmet social and cultural needs are identified during the assessment. The implementation setting replicates real-world service delivery models where presentation may initially be for a physical health need. Upon receipt of referrals from the study team, the Cultural Pathways Program facilitators connect with participants and implement the flexible participant led case management process (Figure 1).
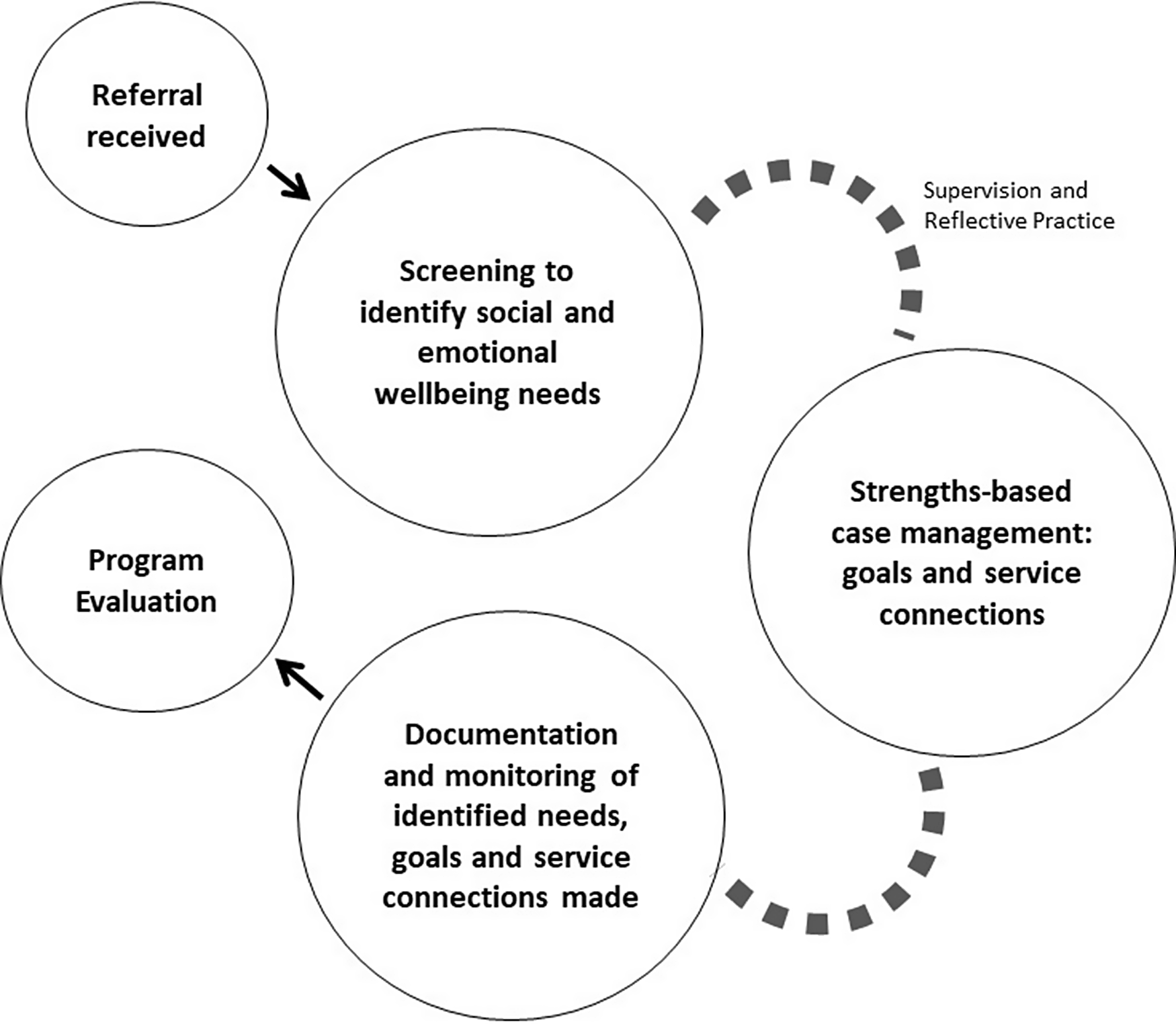
Figure 1. Cultural Pathways Program elements for responding to Aboriginal and Torres Strait Islander social and emotional well-being.
Program elements informing a social and emotional well-being response have been detailed within the following sections, providing the theoretical underpinnings, Cultural Pathways Program approach, embedded Aboriginal and Torres Strait Islander ways of working and opportunities for strengthening practice.
Identifying unmet needs
Screening and assessment is a common first point of engagement in health settings and appropriate screening delivered as part of routine practice can enhance the timely and effective identification of needs and accordingly inform responses or prompt a more comprehensive assessment (Andermann, Reference Andermann2018). Indigenous specific health assessments are associated with improved preventive care for a range of health needs; however, a greater focus is needed on social and cultural factors (Bailie et al., Reference Bailie, Laycock, Matthews, Peiris and Bailie2019; Langham et al., Reference Langham, McCalman, Matthews, Bainbridge, Nattabi, Kinchin and Bailie2017). Cultural Pathways Program facilitators implement a modified Social Needs Screening Tool (Health Leads 2016) to identify unmet social needs of participants. Developed through an Aboriginal and Torres Strait Islander researcher led process, with community input to ensure cultural relevance and responsiveness, the adapted holistic tool covers well-being domains including mental health and cultural and community connection and social domains including financial and food security, transport, employment, housing and social isolation. The process of cultural development ensures the questions are relevant, asked the right way, with cultural meaning and are best able to identify the unique needs of Aboriginal and Torres Strait Islander participants (Brown et al., Reference Brown, Mentha, Rowley, Skinner, Davy and O’Dea2013; Langham et al., Reference Langham, McCalman, Matthews, Bainbridge, Nattabi, Kinchin and Bailie2017). Screening processes for the social determinants must be accompanied by plans for action (Gottlieb et al., Reference Gottlieb, Fichtenberg and Adler2016; Davidson & McGinn, Reference Davidson and McGinn2019), and as part of the program’s case management approach the screening process assists the Facilitator to understand participant needs and enables the identification and prioritisation of participant goals. By implementing a structured and consistent approach, identifying and documenting unmet needs enable the measurement of actions, activities and the monitoring of participant outcomes.
Strengths-Based case management
The program’s case management approach includes goal setting, prioritisation and brokering connections to services. Facilitators work in partnership with participants and tailor responses to individual circumstances and needs. A strengths-based approach to case management ensures facilitators focus on clients’ abilities, talents and resources to enable client’s self-determination skills, develop resilience and the ability to respond or navigate similar situations in the future (Saleebey, Reference Saleebey1996). Goal setting is a common step in the case of management process (Kisthardt et al., Reference Kisthardt, Gowdy and Rapp1992) with theoretical concepts highlighting the importance of collaboration for effective goal setting (Vanpuymbrouck, Reference Vanpuymbrouck2014). An individuals’ sense of control and autonomy influence their willingness to set goals and efforts for achieving them (Vieira & Grantham, Reference Vieira and Grantham2011). The Australian Integrated Mental Health Initiative (AIMhi) is an existing framework that uses strengths based story telling (Nagel & Thompson, Reference Nagel and Thompson2007). The Cultural Pathways Program implements a goal and priority setting framework utilising the AIMhi Pictorial Care Plan (Menzies School of Health Research, 2020) to explore physical, emotional, spiritual, cultural, family, social and work contexts to identify worries, strengths and resources. Consistent with Aboriginal and Torres Strait Islander ways of working, facilitators work in partnership with participants to identify and prioritise issues of most importance that will support improved well-being. As part of the strengths-based, empowerment and person-centred approaches, participants define their own priorities contributing to enhanced autonomy, control and self-efficacy.
As part of the ‘brokering’ approach to case management, facilitators connect participants with services to meet their needs. Making a referral to other services, organisations or agencies are widely implemented in health and social services. Social and emotional well-being and social determinants of health needs span across sectors with often multiple services and agencies involved, this requires coordination to minimise the burden on service users and to enable referrals and connections (Kowanko et al., Reference Kowanko, de Crespigny, Murray, Kit, Prideaux, Miller, Mills and Emden2009). Brokering connections relies on relationships, understandings of what is available across the breadth of health and social needs and understandings of culturally relevant services (McKenna et al., Reference McKenna, Fernbacher, Furness and Hannon2015; Treatment Center for Substance Abuse, 2000). To support this approach, facilitators undertake service mapping exercises to identify the available services and will pro-actively seek the most appropriate service to connect a participant to and reduce barriers to access these services (Huber, Reference Huber2002). Facilitators actively support participants to access services by contacting services on behalf of participants, supporting participants when they contact services themselves and follow up contact with participants to monitor progress. If necessary, facilitators address any challenges or barriers to support the best possible outcome. The active and coordinated approach to brokering connections enhances service access for participants and enables the program to also monitor brokerage outcomes.
Documentation and monitoring
Program monitoring involves measuring and reporting on progress and creates opportunities for continuous quality improvement (Hudson, Reference Hudson2016). Currently, health services rarely systematically collect data about or measure activity on the social determinants of health and require a mechanism to monitor and evaluate the impact of social and emotional well-being services they provide to address health outcomes (Langham et al., Reference Langham, McCalman, Matthews, Bainbridge, Nattabi, Kinchin and Bailie2017; Reeve et al., Reference Reeve, Humphreys and Wakerman2015). Comprehensive understandings of the most appropriate measures for Aboriginal and Torres Strait Islander social and emotional well-being and the social determinants of health are still emerging. Existing national measures of well-being include psychological distress, positive well-being, anger, life stressors, discrimination, cultural identification and removal from natural family (AIHW, 2009). Measures for the social determinants of health as described by the World Health Organization (WHO) Conceptual Framework (Solar & Irwin, Reference Solar and Irwin2010) and outlined in the Aboriginal and Torres Strait Islander Health Performance Framework (AHMAC, 2017) include domains such as connection to country, education, employment, health system, housing, income and transport.
The Cultural Pathways Program combines social and emotional well-being and social determinants of health measures as part of the programs’ monitoring framework. The program utilises REDCap (Research Electronic Data Capture), a secure web platform for managing online databases (Harris et al., Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde2009). The platform collects participant information, demographics and activity data which include when and how people are contacted and the services provided by social/health domain. The program measures factors such as unmet needs, identified goals, whether they have been achieved and the service connections made. The program utilises routine data for ongoing monitoring, quality improvement and as part of funding requirements and obligations. The data collected by the program was informed by Aboriginal and Torres Strait Islander understandings of health and well-being and the wisdom and expertise of the research team and community. The process included the collective development of culturally relevant measures in relation to social and emotional well-being, specifically practical ways to measure progress towards addressing complex social and cultural factors. This process enabled the program to capture information that is useful and relevant for Aboriginal and Torres Strait Islander people. A structured and consistent approach to identifying needs and a specifically designed monitoring framework enables the program to measure progress or outcomes which can be used to understand the needs of service users, to plan responses and to advocate for resources (Harfield et al., Reference Harfield, Davy, McArthur, Munn, Brown and Brown2018).
Culturally relevant supervision
Reflective practice and clinical supervision are recognised by many professions for their role in supporting enhanced clinical practice as well as the health and well-being of the workforce (Koivu et al., Reference Koivu, Saarinen and Hyrkas2012; Scerra, Reference Scerra2012; Thompson & Pascal, Reference Thompson and Pascal2012). This is particularly important for Aboriginal and Torres Strait Islander health workers and practitioners who have complex experiences including burnout and vicarious trauma (Nelson et al., Reference Nelson, Bennett-Levy, Wilson, Ryan, Rotumah, Budden, Beale and Stirling2015). The Aboriginal and Torres Strait Islander health workforce and non-Indigenous workers in Aboriginal and Torres Strait Islander health contexts require access to high-quality cultural and clinical supervision which supports cultural safety, improved practice and well-being (Bainbridge et al., Reference Bainbridge, McCalman, Clifford and Tsey2015; Truong et al., Reference Truong, Paradies and Priest2014). Available frameworks for culturally appropriate supervision with Aboriginal and Torres Strait Islander people include considerations for working with community, looking after self, understanding of roles and professional practice (Koivu et al., Reference Koivu, Saarinen and Hyrkas2012; Nelson et al., Reference Nelson, Bennett-Levy, Wilson, Ryan, Rotumah, Budden, Beale and Stirling2015; Scerra, Reference Scerra2012; Victorian Aboriginal Child Care Agency (VACCA), 2013; Victorian Dual Diagnosis Education and Training Unit (VDDI), 2012). Despite the important role of culturally relevant clinical supervision in enhanced service delivery and the support and retention of the workforce in health care settings (AHCSA, 2020), evidence-based understanding of applied practice models are still emerging in peer reviewed evidence.
The Cultural Pathways Program utilises these existing frameworks as well as the knowledge and experience of program staff to implement a culturally relevant reflective practice and supervision model. An experienced Aboriginal clinician supports facilitators through a range of structures including weekly clinical yarning, one to one yarning and debriefing opportunities as required. Facilitators share perspectives, feelings, challenges, barriers and enablers in relation to both clinical practice as well as system, policy and organisational factors which impact the participant, Facilitator, or the program. Fundamentally, the supervision and reflective practice model are culturally grounded in relationships and yarning to support the cultural safety for Aboriginal and Torres Strait Islander participants whilst also enabling the retention and well-being of the Aboriginal and Torres Strait Islander workforce.
Developmental evaluation
Evaluating health programs and initiatives supports implementation across different contexts utilising insights into how and why they work and whether they have been effective (Lokuge et al., Reference Lokuge, Thurber, Calabria, Davis, McMahon, Sartor, Lovett, Guthrie and Banks2017). There is an increasing recognition of the important role of evidence-based programs featuring high quality and culturally relevant evaluation (Productivity Commission, 2019). The Cultural Pathways Program is underpinned by an Indigenous methodological evaluation framework which utilises Developmental Evaluation, an approach to evaluation that supports innovation and adaptation in complex environments (Fagen et al., Reference Fagen, Redman, Stacks, Barrett, Thullen, Altenor and Neiger2011; Patton, Reference Patton2010), and is consistent with Indigenous methodology and participatory approaches requiring partnerships, trust and shared decision making (Gamble, Reference Gamble2008). The key to developmental evaluation is that the evaluator works with the team in real-time, asking evaluation questions, examining and tracking implications of adaptations and providing timely feedback as the program is implemented and modified or adapted as needed. The evaluator as an Aboriginal woman is immersed in as an insider drawing heavily on reflective practice and utilising the cultural knowledge and expertise of the evaluator as part of the evaluation method. The aim of the evaluation is to understand the process including what was delivered, how it was implemented and the experiences of program participants. The evaluation through reflective and formative methods supports further understanding on the interactions between facilitators, program participants and the broader health and social service contexts. The evaluation framework includes community engagement, governance and approaches which have been purposely selected for their consistency with Indigenous methodologies. This framework ensures that the participation and voice of the community are therefore embedded throughout implementation to support tangible benefits to the community (SAHMRI, 2014).
Conclusions
There is a knowledge to action gap on how to assess and address the social determinants of health within clinical practice to inform the development of coordinated, culturally relevant and strength-based responses to meet the holistic social and emotional well-being needs of Aboriginal and Torres Strait Islander people and communities.
Primary health care services, often as the entry point for accessing health services, are well positioned to implement coordinated health equity responses which include addressing the social determinants of health (Pereira et al., Reference Pereira, Salvi and Verloo2017; Rasanathan et al., Reference Rasanathan, Montesinos, Matheson, Etienne and Evans2011). The absence of a readily applied model creates challenges for the provision of coordinated, resourced and systemic responses to the social determinants of health (CREATE, 2020). Routine screening for unmet needs, implementing strengths-based practice, connecting people to what they need, monitoring service provision and providing clinical and cultural support for the Aboriginal and Torres Strait Islander workforce align to existing practice and are transferable across contexts. Continuous quality improvement and monitoring enables primary health care services to embed new practices into services, systems and routines (Gardner et al., Reference Gardner, Dowden, Togni and Bailie2010).
The ability to implement holistic approaches to Aboriginal and Torres Strait Islander health through the intersection of health and social services requires adequate resources, training and support to clinical workforce (Andermann, Reference Andermann2016), including consideration of roles, responsibilities, scope of practice and readiness to implement strengths-based approaches. These changes cannot be implemented without addressing the ongoing impacts of racism and oppression of Aboriginal and Torres Strait Islander people, allowing for culturally safe systems which are able to meet holistic social and emotional well-being needs (Curtis et al., Reference Curtis, Jones, Tipene-Leach, Walker, Loring, Paine and Reid2019; Durey, Reference Durey2010; Laverty et al., Reference Laverty, McDermott and Calma2017; Muise, Reference Muise2019; Secombe et al., Reference Secombe, Brown, Bailey and Pilcher2019).
The Cultural Pathways Program builds on existing approaches to contribute to practice-based evidence of culturally relevant case management approaches which can be utilised as part of routine care to strengthen the systematic identification and response in primary health care delivery. The combined understandings of the elements outlined in this manuscript provide a framework to inform service planning and tailored implementation which can strengthen social and emotional well-being responses for Aboriginal and Torres Strait Islander people.
Acknowledgements
This work was supported by the Wyatt Benevolent Institution Inc.
Funding
The program is philanthropically funded by the Wyatt Benevolent Institution Inc. TB is funded by an Australian Government Research Training Program Scholarship. AB is funded by an NHMRC Senior Research Fellowship (1137563).
About the contributors
Consistent with cultural protocol we position the contributors to this manuscript:
Tina Brodie is an Aboriginal woman with connections to Yawarrawarrka and Yandruwandha. She is a third year PhD Candidate at The University of Adelaide in the Faculty of Health and Medical Sciences and a Clinical Research Associate in Wardliparingga Aboriginal Health Equity, South Australian Health and Medical Institute. Her Research is exploring Aboriginal and Torres Strait Islander Social and Emotional Well-being, specifically the social determinants of health. Tina has over ten years of experience in Aboriginal and Torres Strait Islander Health in multiple clinical, project and leadership roles working with Aboriginal and Torres Strait Islander children and families. Tina has expertise in Indigenous methodologies and culturally responsive and ethical ways of working and engaging Aboriginal and Torres Strait Islander people and communities in research.
Odette Pearson is a Kuku Yalanji/Torres Strait Islander Population Health Platform Lead in Wardliparingga Aboriginal Research Unit at South Australian Health & Medical Research Institute. Her experience and post-doctoral training in Aboriginal health policy, health systems and inequity comprises a unique comprehensive skillset relevant to existing and emerging complexities of Aboriginal health and well-being. Specifically, Odette seeks to understand how institutional policies and practices drive health and social inequities experienced by Indigenous populations. Her novel approach is the use of community-level information to show and explore the reasons for variations in disadvantage both within the Aboriginal community and between the Aboriginal and non-Aboriginal community. Integral to her research is the inclusion of Aboriginal communities in defining their health and well-being and how Indigenous data can be governed in the future to derive greater benefit for the population.
Luke Cantley has family connections to the Gunditjmara nation of Victoria and is a Research Associate located within Flinders University. Through his research, Luke is determined to solidify Aboriginal culture as a protective factor within the child protection system, whilst exploring the nuances between child safety and cultural safety. Luke holds extensive knowledge on the role unmet social and cultural needs have on positive health outcomes within the Aboriginal and Torres Strait Islander community and holds a strong passion for advocating for increased health care utilisation for health care consumers. Luke has gained extensive experience working as an Aboriginal Health Worker within a strengths-based approach across diverse sectors including Prison health, Primary Health Care, Public Housing and Mental Health Services. Developing expertise in 1) Culturally appropriate and ethical ways of engaging within the community, 2) Health and Well-being assessment methods fostering participatory action research, and 3) Social inequities generated by reduced access to services or resources.
Peita Cooper has a Bachelor of Social Work and currently works within the justice sector. Peita commenced as a Graduate in Wardliparingga Aboriginal Health Equity Theme, at the South Australian Health and Medical Research Institute (SAHMRI). As a Program Facilitator, Peita contributed to the delivery of strengths-based case management and developing culturally responsive practice with Aboriginal and Torres Strait Islander peoples’ and communities. Her previous experience includes working in the disability sector.
Seth Westhead has family connections to the Awabakal and Wiradjuri nations of NSW and is a Research Associate with Wardliparingga Aboriginal Health Equity Theme, South Australian Health & Medical Research Institute. Through his research work, Seth strives to better understand how social and cultural determinants drive health and social inequities within society, particularly as it relates to the Indigenous population. He seeks to better equip communities and young people with tools and evidence for public health advocacy and enable communities to translate health research into meaningful action. Specifically, Seth has expertise in the: 1) conceptual development of Aboriginal specific social determinants and well-being frameworks and tools, 2) implementation of projects involving community engagement and community-led governance structures 2), and 3) undertaking of qualitative research methodologies and community and stakeholder participation interpretation of findings.
Alex Brown is an Aboriginal medical doctor and researcher, he is the Theme Leader of Wardliparingga Aboriginal Health Equity and Professor of Medicine at the University of Adelaide. He grew up on the south coast of New South Wales (NSW) with family connections to Nowra, Wreck Bay and Wallaga Lake on the far south coast of NSW. Over the last 20 years, Alex has established an extensive and unique research program focused on chronic disease in vulnerable communities, with a particular focus on outlining and overcoming health disparities. He leads projects encompassing epidemiology, psychosocial determinants of chronic disease, mixed methods health services research in Aboriginal primary care and hospital settings, and randomised controlled trials of pharmacological and non-pharmacological chronic disease interventions. Alex has been heavily involved in engaging government and lead agencies in setting the agenda in Aboriginal cardiovascular disease management and control and chronic disease policy more broadly. He sits on a range of national committees, and co-chairs the Indigenous Research Health Fund through the MRFF.
Natasha Howard is the Wardliparingga Platform Lead: Implementation Science. The platform incorporates a systems view and privileges Indigenous knowledge to deliver mixed-method inter-disciplinary perspectives which aim to generate policy and practice-based evidence on the social determinants of health. Her experience spans both the health and social sciences, applying population approaches to investigate how the social and built environment enables and promotes cardiometabolic health and well-being, notably for priority populations. She has been active in advocacy and mentoring of the local population health community in both research and practice.
Conflict(s) of interest
None.
Ethical approval
This program was approved by the Aboriginal Health Research Ethics Committee of South Australia (AHREC 04-17-733).






