BACKGROUND
In the emergency department (ED), providers use rapid sequence intubation (RSI) as their preferred method of airway control.Reference Brown, Bair and Pallin 1 RSI involves the simultaneous administration of induction and paralytic agents, which induces favorable intubating conditions and minimizes aspiration risk.Reference Tran, Newton and Mount 2 On the other hand, patient ventilation is interrupted until mechanical ventilation begins. Successful RSI includes the prevention of hypoxia during this apneic period, because hypoxia increases the risk of cardiac arrest and adverse outcomes.Reference Mort 3 One of the primary strategies to avoid hypoxia is preoxygenation prior to intubation.Reference Weingart and Levitan 4 Preoxygenation of the patient creates an oxygen reservoir for the patient to use during the apneic period. Despite preoxygenation, however, hypoxia can still occur.Reference Bodily, Webb and Weiss 5
Apneic oxygenation has been touted as a method to prolong safe apnea time. The technique is performed by leaving nasal cannula on the patient during the apneic period, while an operator performs laryngoscopy and places the endotracheal tube.Reference Weingart and Levitan 4 Apneic oxygenation works because alveoli are able to exchange oxygen even without diaphragmatic movements.Reference Weingart and Levitan 4 When providers give supplemental oxygen to the upper airway, they create a negative pressure gradient between the pharynx and lungs, promoting movement of oxygen into the bloodstream. In the operating room setting, apneic oxygenation prolongs time to desaturation from 3.5 to 5.3 minutes.Reference Ramachandran, Cosnowski and Shanks 6 Apneic oxygenation has received rapid uptake among the emergency medicine communityReference Sakles, Mosier and Patanwala 7 , Reference Sakles, Mosier and Patanwala 8 and has the advantages of being inexpensive, practical, and safe in most patients.Reference Sakles 9
Nevertheless, patients who are intubated in the ED and intensive care unit (ICU) settings are acutely and often critically ill. Benefits of apneic oxygenation in this patient population have been conflicting with some studies showing benefitReference Sakles, Mosier and Patanwala 7 , Reference Jaber, Monnin and Girard 10 and others showing no benefit.Reference Semler, Janz and Lentz 11 - Reference Besnier, Guernon and Bubenheim 14 Oliveira et al.Reference Oliveira, Silva, Cabrera and Barrionuevo 15 conducted a systematic review and meta-analysis to provide clarity on the overall state of the evidence.
POPULATION STUDIED
The study authors included studies in both the ED and ICU setting because those intubations occur on an urgent or emergent basis in a controlled environment. The authors excluded studies in the operating room or out-of-hospital environments. For studies to be included, patients had to receive oxygen during the apneic period, using any technique. Both randomized controlled trials (RCTs) and observational studies were included because there are few studies available.
STUDY DESIGN
A trial protocol was listed on the PROSPERO website prior to the systematic review. A medical librarian performed a comprehensive search of literature for studies on apneic oxygenation from 2006 until 2016 using Ovid MEDLINE, EMBASE, CENTRAL, and Scopus, without language restriction. The authors searched gray literature, ongoing clinical trials, and reference lists. Two investigators independently performed study selection and data extraction. Included studies were described in detail, and reasons for study exclusion were enumerated. The authors assessed risk of bias using standardized tools. They performed a meta-analysis with random-effects models using Review Manager (Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). They used odds ratios (OR) and weighted mean differences with 95% confidence intervals (CI) to measure pooled-effect estimates, as well as the I 2 statistic to judge study heterogeneity. The subgroup analysis included risk of bias. The authors adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.Reference Liberati, Altman and Tetzlaff 16
OUTCOME MEASURES
The authors considered the lowest SpO2 peri-intubation, hypoxemia (SpO2<93%), severe hypoxemia (SpO2<80%), and life-threatening hypoxemia (SpO2<70%). First-pass success was also reported. Furthermore, the authors examined some ICU outcomes, including duration of mechanical ventilation, ICU length of stay, and ICU mortality.
RESULTS
The authors identified 1386 potential studies, eventually narrowing it down to 14 for qualitative and 8 for quantitative analysis. The included studies involved 2023 patients, 369 of which were studied in the RCT context. Six of the studies were done in the ED and two in a mixed ED-ICU setting. Five trials were RCTs, with one done in the ED. The ED trial included only 13 patientsReference Horan, Berns and Malone 17 and was not quantitatively analysed.
The primary sources of heterogeneity were the setting and context for intubation, approaches to preoxygenation, approaches to apneic oxygenation, and proceduralist experience. Outcomes of the meta-analysis are listed in Table 1.
Table 1 Summary of main outcomes of Oliveira et al.’s meta-analysis

During a subgroup analysis, the authors found that, when they exclusively combined studies at low risk of bias,Reference Jaber, Monnin and Girard 10 , Reference Semler, Janz and Lentz 11 , Reference Besnier, Guernon and Bubenheim 14 apneic oxygenation had no benefit.
COMMENTARY
We used the AMSTAR 2 checklist,Reference Shea, Reeves and Wells 18 which rated a high overall confidence in the systematic review. The authors did not perform a funnel plot to evaluate publication bias, which, in this case, is appropriate because the number of studies were few, most studies had few patients, and the overall treatment effect is small.Reference Lau, Ioannidis and Terrin 19
The most significant limitation of the meta-analysis is the overall low-to-moderate certainty in the evidence with small sample sizes among the included studies. Only three studies were deemed to be of low risk of bias, none among the ED population. Furthermore, both ICU and ED settings were combined. The ICU studies primarily used high-flow apneic oxygenation devices, which provide additional physiologic benefits compared to the low-flow devices that are available in most EDs. Therefore, the effect size for low-flow devices is likely more modest than reported in the meta-analysis.
Since the publication of the meta-analysis, the ENDAO trial was performed, the first high-quality RCT comparing apneic oxygenation against usual care among ED patients.Reference Caputo, Azan and Domingues 20 This study enrolled 206 patients and found no difference in the primary outcome of lowest peri-intubation oxygen saturation.
We contacted the lead author of the ENDAO trial, who supplied nonpublished data for lowest peri-intubation oxygen saturation and first-pass success, which we used in a Forest plot with the other RCTs from the Oliveira et al. meta-analysis (Figure 1). The benefit of apneic oxygenation for improving lowest oxygen saturation loses statistical significance, although moderate study heterogeneity is introduced (difference 1.59%; 95% CI -0.90% to 4.08%, I 2 =47%) (see Figure 1). The heterogeneity may be because this was the first high-quality RCT in the ED setting, or perhaps because patients had a mean of only 60 seconds of apnea. Similarly, the benefit of first-pass success is not maintained, without a significant change in heterogeneity (OR 1.13; 95% CI 0.74 to 1.74, I 2 =0%) (see Figure 1).
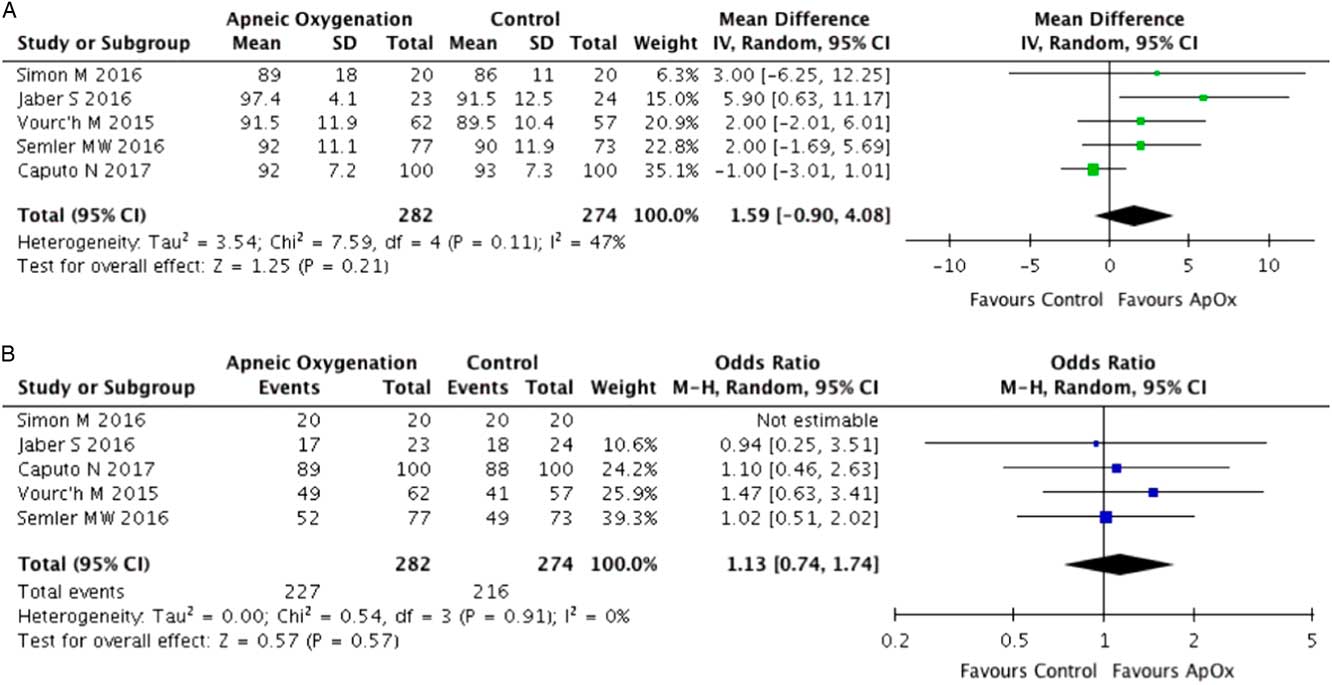
Figure 1 Forest plots of randomized controlled trials from Oliveira et al.’s meta-analysis on periprocedural outcomes, with Caputo et al.’s data added. A) Lowest oxygen saturation (SpO2) peri-intubation. B) First-pass success.
Overall, we caution against over-enthusiasm for apneic oxygenation and agree with the measured conclusion of the meta-analysis, that “apneic oxygenation is a potentially important adjunct for emergency airway management.” To prevent hypoxia, ensuring proper preoxygenation is likely more valuable than apneic oxygenation.Reference Weingart and Levitan 4 , Reference Sakles 9
CONCLUSION
The use of apneic oxygenation may provide incremental benefit to intubation in the ED. Apneic oxygenation does not replace basics in airway management, such as preoxygenation or technical skill. Further studies may help define which patient groups benefit from apneic oxygenation and be powered to examine potential adverse effects.
Competing interests: None declared.
Author contributions: Both authors contributed to the conception, drafting, and revising of the article. Both authors approved the final version to be published and agreed to act as guarantors of the results.






