Introduction
Globally, depression is one of the most common mental health problems and is considered detrimental to an individual’s well-being (Fisher et al. Reference Fisher, Seow and Brazil2014). According to the World Health Organization, depression significantly contributes to the overall disease burden and is a leading cause of disability worldwide (World Health Organization 2020). International prevalence rates for older adults (65+ years) vary, as high as 37% for those with mild symptoms of depression and 9% for those with major depression (Freeman et al. Reference Freeman, Smith and Neufeld2016). Depression is associated with loneliness (Cacioppo et al. Reference Cacioppo, Hawkley and Thisted2010), loss of interest in usual activities, and memory problems in older adults (Cappeliez Reference Cappeliez2014).
While there is literature on depression in various populations, there is limited research focused on depressive symptoms in home care clients. A study conducted in 2014 reported prevalence rates of depression in Canadian palliative home care clients to be 10% (Fisher et al. Reference Fisher, Seow and Brazil2014). However, this is likely an underestimate, given that depression in seriously ill and palliative home care recipients is often underdiagnosed (Mitchell et al. Reference Mitchell, Chan and Bhatti2011). People experiencing depression who do not completely recover from depressive symptoms are at an increased risk of developing depression again and, as a result, may continue to experience negative health outcomes. The prevalence rates of depression for seriously ill and older adults indicate that it is vital to screen for depression in home care settings because it can have adverse consequences on palliative clients. As seriously ill individuals are those who have a life-limiting illness including, but not limited to, dementia, organ failure, and cancer (Harman et al. Reference Harman, Guthrie and Cohen2019), they could benefit from a palliative approach to care to address critical needs such as symptom management, caregiver support, and psychosocial support. The palliative care (PC) approach has extended to include all individuals with serious and life-limiting illnesses and emphasizes an equal focus on psychological, social, emotional, spiritual support, as well as the physical aspect of treatment (Harman et al. Reference Harman, Guthrie and Cohen2019). Furthermore, PC teams work to provide the optimal quality of life for seriously ill and dying individuals at the end-of-life by doing their utmost in managing symptoms and reducing pain while providing support to the person’s family and friends (Health Canada 2018). Depression is particularly important to recognize in seriously ill clients due to its intrinsic burden and significant association with physical symptoms such as pain, sleep problems, and gastrointestinal disorders (Fisher et al. Reference Fisher, Seow and Brazil2014). There are a number of known risk factors associated with depression, including low life satisfaction, being female (Fisher et al. Reference Fisher, Seow and Brazil2014), and expressing a desire to die (Freeman et al. Reference Freeman, Smith and Neufeld2016). Some evidence suggests that low social support from friends and family is the most significant factor predicting a failure to improve in depressive symptoms in a palliative population (Goodwin et al. Reference Goodwin, Lee and Price2011). Therefore, diagnosing and treating depressive symptoms and providing adequate care to individuals with depression is important to improve the overall quality of life for individuals with a serious or life-limiting illness (Freeman et al. Reference Freeman, Smith and Neufeld2016).
Publicly funded home care provides services to support individuals who may need assistance to care for themselves due to varying health conditions and/or functional limitations (Health Quality Ontario 2016). Home care offers health services to people of all ages and incorporates end-of-life care, support, and maintenance for individuals with chronic illnesses and functional impairments and support for family caregivers (Accreditation Canada and the Canadian Home Care Association 2015). Home care is also important to consider as most individuals prefer to receive care in the comfort of their own homes and remain in their homes for as long as possible. Predictors of depression in home care settings included pain, sleep disorders, caregiver burden (Williams et al. Reference Williams, Jamal and Guthrie2018), cognitive impairment, poor self-rated health, and speaking a language other than English or French (Guthrie et al. Reference Guthrie, Theriault and Davidson2015). Identifying and understanding the difference between individuals who experienced improved depressive symptoms compared to those who did not could help service providers and policymakers improve the quality of care for older adults with depression. Currently, little is known about individuals with persistent depression and the potential risk factors in older seriously ill adults receiving home care in Canada. Therefore, the goal of the current study was to examine the key risk factors associated with failing to improve symptoms of depression in a cohort of seriously ill older adults (65+) in Canada.
Methods
Data source
The study was a retrospective cohort study representing secondary analysis of the Resident Assessment Instrument for Home Care (RAI-HC) among clients from Ontario, Yukon Territory, Alberta, Newfoundland and Labrador, British Columbia, Manitoba, and Nova Scotia. The RAI-HC is a standardized assessment currently used in these provinces/territories in Canada for all long-stay clients (i.e., individuals expected to receive 60+ days of home care (Harman et al. Reference Harman, Guthrie and Cohen2019)). The assessment contains approximately 300 items, covering key domains such as functional ability, cognition, mood and behavior, communication, and pain (Guthrie et al. Reference Guthrie, Pitman and Fletcher2014; Harman et al. Reference Harman, Guthrie and Cohen2019) and is completed electronically by a trained health-care professional (e.g., registered nurse) in the person’s home. Completion of the assessment includes obtaining information from several sources, including speaking with the client, their caregiver, and health-care professionals (e.g., primary care physician) and the use of clinical records, as needed.
Study sample
The study sample included seriously ill home individuals aged 65+ years who had at least 1 assessments completed within 12 (n = 8,304) items. The data were de-identified before being shared with the research team. Individuals were classified as being seriously ill if they had a prognosis of less than 6 months to live, a Changes in Health, End-Stage Disease and Signs and Symptoms (CHESS) score of 4 or 5, or one of the goals of care, on admission to the home care program, was PC. Prognosis was determined by a single dichotomous item on the RAI-HC (person has less than 6 months to live [yes/no]). The CHESS scale is 1 of the 6 health index scales embedded within the assessment. The CHESS scale contains 12 items used to measure health instability and to identify those at risk of mortality (Hirdes et al. Reference Hirdes, Poss and Mitchell2014). The scale ranges from zero (no health instability) to five (severe health instability) and has been shown to be a significant predictor of mortality. For every one-point increase on the CHESS scale, there is an almost 2-fold increased risk of mortality (Hirdes et al. Reference Hirdes, Poss and Mitchell2014). The Research Ethics Board at Wilfrid Laurier University reviewed and approved the study (REB#: 6595).
Measures
The main outcome of interest was a failure to improve on symptoms of depression, which was assessed using the Depression Rating Scale (DRS). The DRS, another health index scale embedded within the RAI-HC, is a 14-point summative scale that screens for signs/symptoms of depression using 7 mood and behavior items. There is some evidence of criterion validity against the Hamilton Depression Rating Scale and the Cornell Scale for Depression (Burrows et al. Reference Burrows, Morris and Simon2000). A cut point of 3 or higher was used to indicate moderate to severe depressive symptoms as this has been found to be predictive of a clinical diagnosis of depression (Martin et al. Reference Martin, Poss and Hirdes2008).
Seriously ill clients who experienced depressive symptoms (i.e., a DRS score of 3 or higher) at baseline (time 1 or T1) and had a follow-up assessment within 12 months were included in the study cohort. Individuals were defined as having persistent symptoms of depression if their DRS score did not improve or remained the same at time 2 (T2) (i.e., DRS score continued to be 3 or higher). All others were considered to have some degree of improvement in their symptoms.
Health index scales
There are 5 other health index scales and algorithms embedded within the RAI-HC, which are automatically generated upon completion of the assessment. Across these scales, higher scores indicated a greater degree of impairment.
1. The Instrumental Activities of Daily Living (IADL) Involvement Scale is a 21-point summative scale that measures independence in activities such as housework, meal preparation, and managing medications. A score of 14+ was chosen as a cut point to indicate a greater level of impaired functioning when performing these tasks (Landi et al. Reference Landi, Tua and Onder2000). Criterion validity has been established for this scale as it is correlated with the Lawton Instrumental Activities of Daily Living Scale (Lawton and Brody Reference Lawton and Brody1969).
2. The Activities of Daily Living Self-Performance Hierarchy Scale (ADL-S) is used to characterize functional performance in areas of personal care such as eating and dressing. This scale weights early loss ADLs, such as dressing, lower than late loss ADLs, such as eating. Scores range from 0 (independent) to 6 (total dependence). A cut point of 2 or higher was used to identify clients who needed some assistance to complete these tasks. The ADL-S has been shown to have excellent inter-assessor reliability (Morris et al. Reference Morris, Fries and Morris1999), and there is some evidence of criterion validity against the Barthel Index (Landi et al. Reference Landi, Tua and Onder2000).
3. The Pain Scale is a 4-point scale that measures the intensity and frequency of pain, where a score of 2 or higher indicates pain that is daily or severe. Predictive validity has been established when compared to the Visual Analogue Scale scores (Fries et al. Reference Fries, Simon and Morris2001).
4. The Cognitive Performance Scale (CPS) measures impairment in cognitive functioning based on 4 items including short-term memory, expressive communication, decision-making, and independence in eating. The scale ranges from 0 to 6, and a cut point of 2 or more was used to indicate at least mild impairment in cognitive performance. The CPS scores correlate with those obtained using the Mini Mental Sate Exam (Morris et al. Reference Morris, Fries and Mehr1994) and the Montreal Cognitive Assessment (Jones et al. Reference Jones, Perlman and Hirdes2010).
5. The Deafblind Severity Index (DbSI) is derived from 2 items on the RAI-HC measuring vision and hearing. The DbSI ranges from 0 (no impairment in either sense) to 5 (severe impairment in both senses). A cut point of 3 or higher was used to identify those with at least mild impairment in both vision and hearing (Guthrie et al. Reference Guthrie, Theriault and Davidson2015). Scores on the DbSI are associated with both a greater difficulty interacting with others and a greater difficulty performing IADLs (Dalby et al. Reference Dalby, Hirdes and Stolee2009; Guthrie et al. Reference Guthrie, Theriault and Davidson2015).
6. The Caregiver Risk Evaluation (CaRE) is used to categorize informal caregivers into 1 of 4 independent groups: low, moderate, high, and very high risk of experiencing caregiver burden. There is some evidence of predictive validity as those in the very high-risk group have loved ones who are at an increased risk of long-term care admission (Guthrie et al. Reference Guthrie, Williams and Beach2019).
Other measures
Demographic characteristics examined as potential risk factors for persistent depression included age, sex, marital status, language, and education. The language item is categorized as whether the client spoke English, French, or other (i.e., a language other than English or French). The number of comorbid chronic conditions was also explored (0–3 vs. 4+). Psychiatric diagnosis (e.g., anxiety, depression, schizophrenia, and bipolar disorder) was measured as a dichotomous item (present/not present). Antidepressant medication measured whether the client took the medication in the last 7 days or since last assessment and was examined with a dichotomous item (yes/no). There are several items on the RAI-HC that gather information regarding a client’s social functioning. These include whether the client was at ease interacting with others (at ease/not at ease) or if the client openly expressed conflict or anger with family/friends (yes/no). A change in their social activities was represented by a decline in the client’s level of participation in religious, social, occupational, or other preferred activities compared to the previous 90 days. This item has 3 response options: no decline, decline and not distressed, or decline and distressed. Self-reported loneliness was examined with a single dichotomous item (yes/no).
Analysis
Univariable analysis
Several variables were examined as potential risk factors associated with failing to improve on depressive symptoms based on our research objectives and the existing literature. Chi-square tests were used, at the bivariate level, to analyze differences for categorical variables. In the current analysis, p-values were used to determine important covariates associated with the main outcome of interest but were not the sole means for defining important predictors. Given the large sample size and the fact that there was evidence of type 1 error, we also used the odds ratio (ORs) and 95% confidence interval (95% CI) to identify key predictors. An OR representing an approximately 20% change was chosen to identify variables that appeared to be clinically relevant predictors (i.e., OR ≤ 0.83 or an OR ≥ 1.2). In most cases, the missing data was less than 10%.
Multivariable analysis – model building
A multivariate logistic regression model was created to determine the most important factors associated with experiencing persistent depressive symptoms. Forward selection, backward elimination, and stepwise procedures were useful to identify covariates that were important for further examination. Variables that were statistically significant (2-tailed alpha level = 0.05) in at least one of the stepwise procedures were considered for further analysis. Best subsets selection was also used to help identify important variables to be included in the final model. Several variables were not statistically significant following these procedures, including expressive communication, hearing, and dementia. However, we forced these variables back into the model since they were of interest to our research goals and have been cited in the literature. Ultimately, these variables did not remain in the final model. Model fit was examined using the goodness-of-fit statistic. Multicollinearity was assessed using polychoric correlations for ordinal variables and tetrachoric correlations for dichotomous variables. A cut point of 0.40 or greater was used to identify variables that needed to be removed to avoid multicollinearity (Gadermann et al. Reference Gadermann, Guhn and Zumbo2012). Hearing impairment, expressive communication, antidepressant use, and dementia all exceeded this cutoff and were removed from the model. To explore the effect of potential confounding relationships, stratified analyses were conducted using the Cochran Mantel–Haenszel chi-square test and the Breslow–Day test. Significant chi-square values from this Breslow–Day test were used to identify evidence of confounding, and these variables were then forced into the final model.
All 2-way interactions between age, sex, language, pain, any psychiatric diagnosis, if the person was at ease interacting with others, CPS, self-reported loneliness, self-rated health, CaRE, vision decline, and multi-morbidity were examined. There were significant interactions between loneliness and age (74–84 years) and between language and a few other variables, including pain, CPS, loneliness, self-rated health, and multi-morbidity. For all significant interactions, we performed stratified analyses to better understand the nature of the interaction. All analyses were performed using the SAS software (version 9.4) (SAS Institute Inc 2016). The study followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (von Elm et al. Reference von Elm, Egger and Altman2007).
Results
Of the total sample (N = 8,304), 64% of clients did not improve on their depressive symptoms at T2, while the remainder did. The mean length of time between T1 and T2 was 4.9 months (SD = 3.3). The mean age of the sample was 80.8 years (SD = 7.7), 61.1% were female, 82.1% spoke English as their primary language, and 40.6% were married. The most common diagnoses in the sample were arthritis (47.2%) and hypertension (61.7%; Table 1).
Table 1. Demographic and other characteristics comparing clients who improved and failed to improve in depressive symptoms
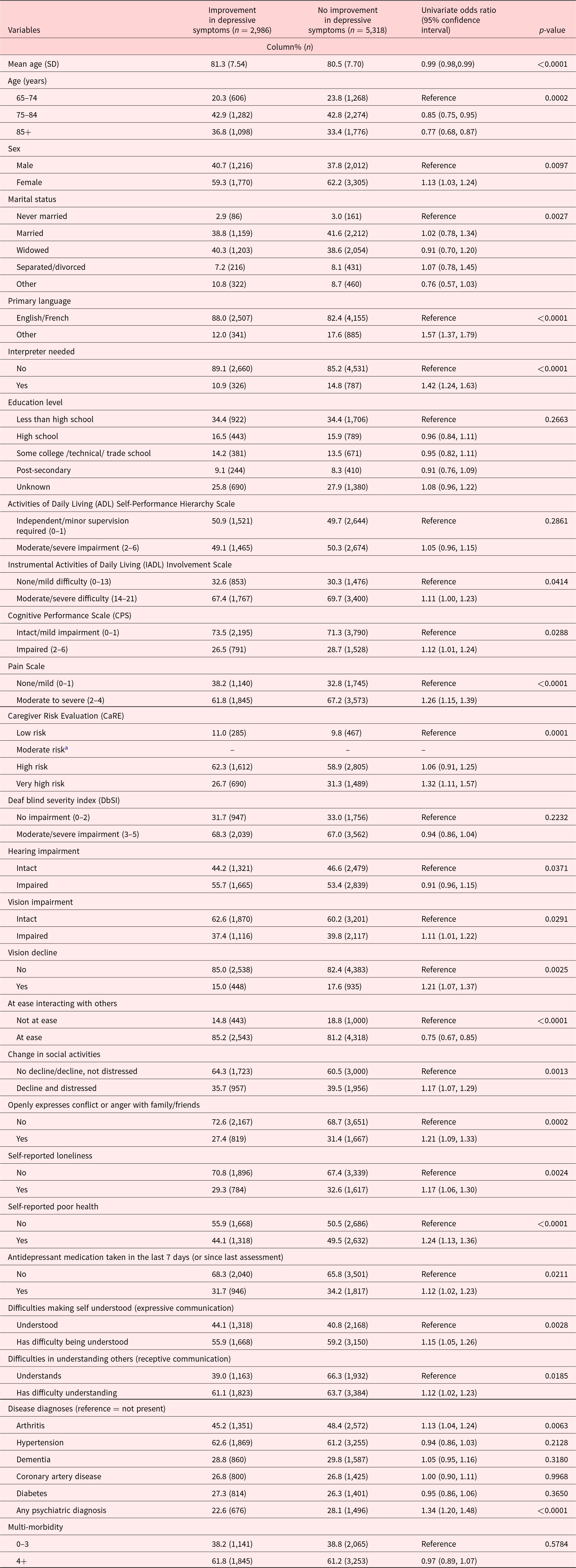
a There were 917 values from the moderate risk category that could not be calculated. This category captures individuals with a DRS score of ≤2, but the participants of the study had to have a DRS score of ≥3 at T1.
Nine variables had univariate ORs that showed an increase in the odds of failing to improve on symptoms of depression. The top 5 with the highest ORs included speaking a language other than English or French (OR = 1.57; 95% CI = 1.37, 1.79), requiring an interpreter (OR = 1.42; CI = 1.24, 1.63), having any psychiatric diagnosis (OR = 1.34; CI = 1.20, 1.48), having a caregiver at very high risk of experiencing burden (OR = 1.32; CI = 1.11, 1.57), and experiencing moderate to severe pain (OR = 1.26; CI = 1.15, 1.39). Conversely, being aged 85+ years (OR = 0.77; CI = 0.68, 0.87) and feeling at ease when interacting with others (OR = 0.75; CI = 0.67, 0.85) were associated with a significant reduction in the odds of persistent depressive symptoms (Table 1). Several variables that were statistically significant remained in the final model, including sex, self-rated poor health, self-reported loneliness, and multi-morbidity; however, after adjusting for all other covariates in the model, these variables were no longer clinically significant.
Multivariable analysis – main effects model
In the process of developing the final main effects model, several steps were taken. For example, several variables seemed clinically significant including sex, self-rated poor health, self-reported loneliness, and multi-morbidity. However, after adjusting for all other covariates in the model, these variables were no longer clinically significant. There was evidence of confounding with CPS (p = 0.0172) and self-reported loneliness (p = 0.0353) for the relationship between language and experiencing persistent depression. Although CPS was initially dropped from the model, it was retained as it was a strong risk factor in the literature for depression among seriously ill older adults. Due to the presence of the confounding relationships, both CPS and self-reported loneliness were retained in the final model (Table 2).
Table 2. Final main effects logistic regression model examining potential risk factors associated with failure to improve on depressive symptomsa
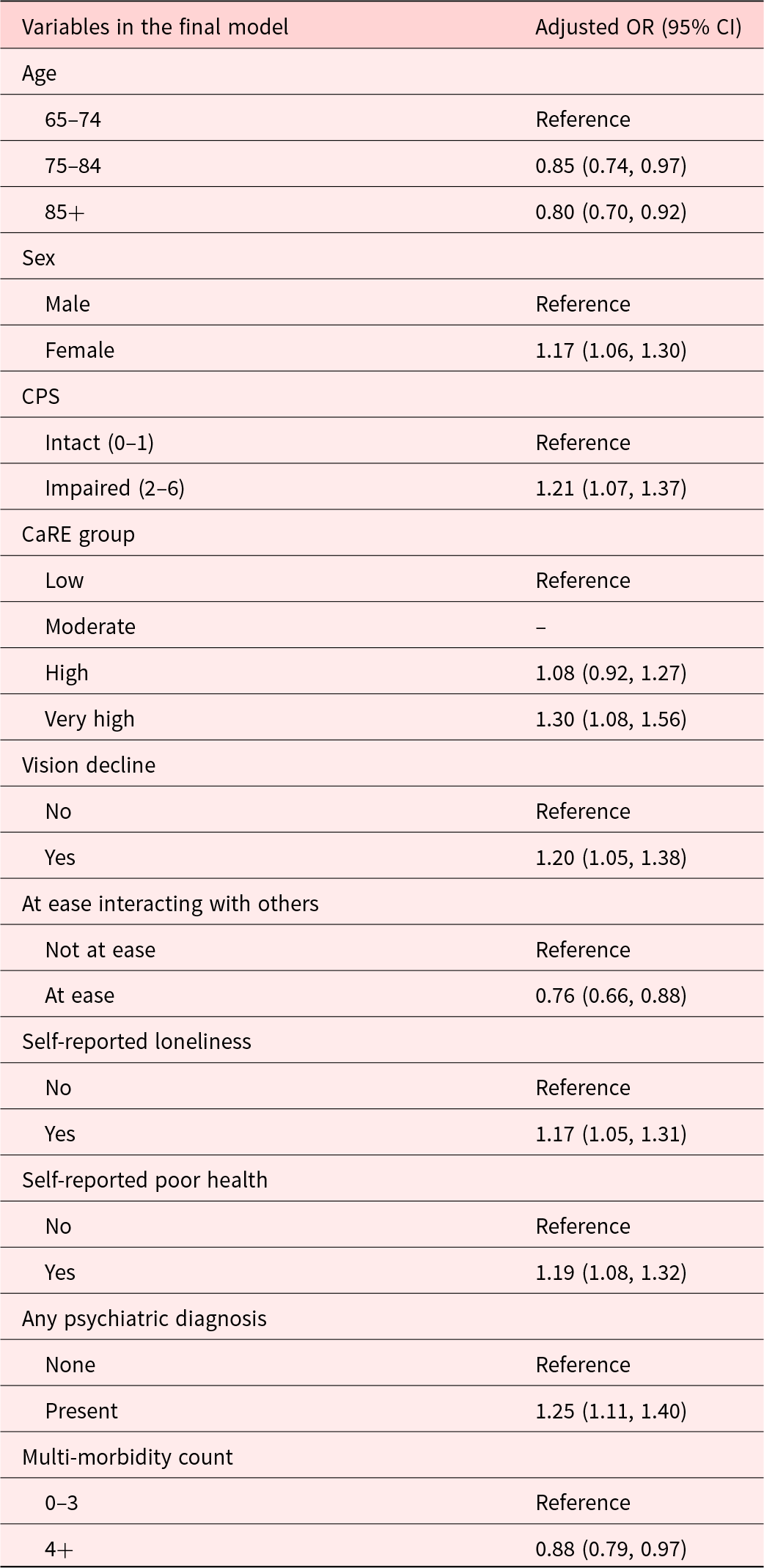
a Represents main effects model without interaction term.
In the final main effects model, having a caregiver at very high risk of experiencing burden (OR = 1.30; CI = 1.08, 1.56), having any psychiatric diagnoses (OR = 1.25; CI = 1.11, 1.40), individuals with impaired cognitive functioning (OR = 1.21; CI = 1.07, 1.37), and vision decline (OR = 1.20; CI = 1.05, 1.38) significantly increased the odds of failing to improve symptoms of depression among seriously ill home care clients. Being aged 85+ years (OR = 0.77; CI = 0.68, 0.87) and feeling at ease when interacting with others (OR = 0.75; CI = 0.67, 0.85) significantly reduced the odds of experiencing persistent depressive symptoms. Table 2 displays the main effects model without the interaction so that all of the adjusted ORs could be reported. However, one significant interaction was present in the multivariable model between speaking a language other than English or French and experiencing moderate to severe pain. To better understand this interaction, the sample was stratified based on whether clients spoke English/French or another language. In the group who spoke a different language and experienced an improvement on their depressive symptoms, 62% had severe pain. Conversely, in that same group, but among those who did not experience an improvement on their depressive symptoms, 75% experienced severe pain (standard difference = −0.27).
Discussion
To our knowledge, this is the first Canadian study to examine seriously ill older adults receiving home care services who experienced a failure to improve on symptoms of depression. In this retrospective cohort study, 64% of individuals continued to experience depressive symptoms on follow-up, within a 12-month time frame. This is an important finding to address because not only do these clients have other comorbidities and life-limiting illnesses but roughly two-thirds are also experiencing ongoing depressive symptoms. The present study found that language, pain, and caregiver burden were the most important predictors associated with a failure to improve on symptoms of depression. Since persistent depressive symptoms can adversely impact the health and quality of life of seriously ill older adults (Cappeliez Reference Cappeliez2014; Freeman et al. Reference Freeman, Smith and Neufeld2016), this research is a critical first step toward understanding these complex relationships.
Canada is officially a bilingual country, and most Canadians (98.2%) speak English or French as their primary language (Statistics Canada 2016). The current study found that language and pain increased the risk of experiencing continued depressive symptoms. Speaking a language other than 1 of the 2 official languages may lead to individuals feeling excluded (Cairney and Krause Reference Cairney and Krause2005) and, as a result, could lead to them feeling isolated (Office of the Commissioner of Official Languages 2013) and at higher risk of continuing to feel depressed (Cairney and Krause Reference Cairney and Krause2005; Ge et al. Reference Ge, Yap and Ong2017). This may be further complicated when an individual has a life-limiting illness and is trying to communicate with health-care professionals. Furthermore, pain is one of the most common symptoms experienced by palliative home care clients (Wilkie and Ezenwa Reference Wilkie and Ezenwa2012) and is associated with the development of depressive symptoms in home care (Fisher et al. Reference Fisher, Seow and Brazil2014; Guthrie et al. Reference Guthrie, Theriault and Davidson2015; Williams et al. Reference Williams, Jamal and Guthrie2018). Clients who speak a language other than English or French may be less able to communicate their needs, and their pain symptoms, and therefore, the most appropriate treatments may not be provided, which in turn could lead to continued poor mental health (Ohtani et al. Reference Ohtani, Suzuki and Takeuchi2015; Bauer et al. Reference Bauer, Chen and Alegría2010; Sentell et al. Reference Sentell, Shumway and Snowden2007). Among individuals who required a language interpreter to complete the assessment, they were 42% more likely to continue to experience symptoms of depression, indicating there may have been additional communication barriers. Based on our results, cognitive impairment and speaking a language other than English or French increased the risk of continuing to experience depressive symptoms. Previous research indicates that memory and communication skills, including comprehension and production of language, are often impaired as a result of cognitive impairment (Johnson and Lin Reference Johnson and Lin2014; Mueller et al. Reference Mueller, Hermann and Mecollari2019). This can make it difficult for clients to receive the care they need, especially those who are already unable to communicate in English. This is where a holistic approach to care like PC that may benefit these individuals as there is equal focus on integrative treatments with psychological, social, and emotional forms of treatment (Ferrell Reference Ferrell2005; Murray et al. Reference Murray, Firth and Schneider2015).
Most Canadians prefer to receive care in their homes for as long as possible and die in the comfort of their own homes (Canadian Hospice Palliative Care Association 2013; Canadian Institute for Health Information 2018). Care is mostly provided by an informal caregiver such as a family or friend. Typically, informal caregivers are often trying to balance many aspects of the person’s care, including the physical, psychological, emotional, and financial aspects of caregiving. The increased demand of caring for someone with a serious illness can lead to the informal caregiver feeling burden in their role (Guerriere et al. Reference Guerriere, Husain and Zagorski2016; Hirdes et al. Reference Hirdes, Freeman and Smith2012; Luymes et al. Reference Luymes, Williams and Garrison2021). In the current study, the risk of caregiver burden increased the likelihood that individuals continued to experience symptoms of depression. We see this reported in other literature, which confirms that when it comes to individual health, the caregiver’s health feeds into that, so it is imperative that the informal caregiver be supported like in PC (Williams et al. Reference Williams, Jamal and Guthrie2018). PC should be holistic in nature and encompass both the individual and their family. It is imperative that informal caregivers caring for individuals with a serious illness have access to proper resources and feel supported in their role.
The present study has several strengths including the large sample size and longitudinal design. The rates of functional impairment and pain across this group of seriously ill individuals are similar to previous studies looking at home care clients who died from cancer (Seow et al. Reference Seow, Barbera and Sutradhar2011) or clients who received palliative home care (Freeman et al. Reference Freeman, Smith and Neufeld2016). A potential limitation of the current study was the selection of using the first 2 consecutive assessments to examine individuals with continued depressive symptoms over time. Although an individual may have experienced symptoms of depression before being admitted to the home care program, we ultimately decided to use the first 2 assessments to capture the beginning of receipt of home care services. While some individuals may have received treatment previously, the RAI-HC assessment does not include the level of detail required to understand how long they had received treatment. In addition, we do not know whether individuals improved over time due to the medications they were taking or how long they had been taking these medications to treat depressive symptoms, as these data are not available on the RAI-HC. We have identified a group of seriously ill home care clients who we anticipate would benefit from a palliative approach to their care. However, we were unable to definitively ascertain if they truly were receiving palliative home care services.
Conclusion
Currently, little is known about the progression of depressive symptoms in seriously ill older adults. A clearer understanding of the complexity and the factors associated with this outcome is an important step toward providing optimal quality of care to clients who are seriously ill, dying, and also experiencing persistent symptoms of depression. Persistent depression is highly prevalent among seriously ill home care clients and, if not treated, may be an indicator of “bad death.” Multiple variables are modifiable including communication barriers and caregiver burden, which makes it critical to recognize these risk factors so interventions may be implemented to better the person’s quality of life throughout the course of their illness.
Acknowledgments
Not applicable.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
Dawn M. Guthrie is a Fellow with interRAI. All authors confirm they have no conflicts of interest to disclose.







