Borderline personality disorder (BPD) is a serious form of psychopathology characterized by a pervasive pattern of instability in the regulation of affect and emotion, dysfunctional interpersonal relationships, disturbed self-identity, and chronic feelings of emptiness (Fossati, Feeney, Maffei, & Borroni, Reference Fossati, Feeney, Maffei and Borroni2014a; Guilé, Boissel, Alaux-Cantin, & Garny de La Rivière, Reference Guilé, Boissel, Alaux-Cantin and Garny de La Rivière2018; Stead, Boylan, & Schmidt, Reference Stead, Boylan and Schmidt2019; Warmingham, Rogosch, & Cicchetti, Reference Warmingham, Rogosch and Cicchetti2020). Symptoms of BPD are also frequently found in both clinical (e.g., depressed patients) and nonclinical samples (Chabrol & Leichsenring, Reference Chabrol and Leichsenring2006; Fossati, Gratz, Maffei, & Borroni, Reference Fossati, Gratz, Maffei and Borroni2014b; Leichsenring, Leibing, Kruse, New, & Leweke, Reference Leichsenring, Leibing, Kruse, New and Leweke2011). Emerging evidence has shown that adolescence is a particularly sensitive period for the emergence of borderline personality disorder symptoms (BPDs) and that BPD constitutes a valid and reliable diagnosis in adolescents, comparable with those in adults. Evidence also suggests that BPDs in adolescence are often precursors to a diagnosis of BPD (Chanen & McCutcheon, Reference Chanen and McCutcheon2013; Kaess, Brunner, & Chanen, Reference Kaess, Brunner and Chanen2014; Sharp, Steinberg, Temple, & Newlin, Reference Sharp, Steinberg, Temple and Newlin2014).
Multiple studies have found that childhood maltreatment (CM) experiences are significant risk factors in the development of adolescent BPD (Ibrahim, Cosgrave, & Woolgar, Reference Ibrahim, Cosgrave and Woolgar2017). Specifically, early traumatic separations, physical and sexual abuse, psychological maltreatment, emotional neglect, low care, and parental loss are associated with an increased likelihood of later BPD (Carr & Francis, Reference Carr and Francis2009; Gratz, Tull, Baruch, Bornovalova, & Lejuez, Reference Gratz, Tull, Baruch, Bornovalova and Lejuez2008; Infurna et al., Reference Infurna, Brunner, Holz, Parzer, Giannone, Reichl and Kaess2016; Porter et al., Reference Porter, Palmier-Claus, Branitsky, Mansell, Warwick and Varese2020). Evidence suggests that these forms of traumatic experiences rarely occur in isolation (Huang et al., Reference Huang, Yang, Wu, Napolitano, Xi and Cui2012; Zanarini et al., Reference Zanarini, Williams, Lewis, Reich, Vera, Marino and Frankenburg1997). Specifically, individuals with psychopathological disorders are more likely to have experienced multiple forms of abuse, such as verbal, physical, and emotional abuse (Ajnakina et al., Reference Ajnakina, Trotta, Di Forti, Stilo, Kolliakou, Gardner-Sood and Fisher2018; Annerbäck, Sahlqvist, Svedin, Wingren, & Gustafsson, Reference Annerbäck, Sahlqvist, Svedin, Wingren and Gustafsson2012; Trotta et al., Reference Trotta, Murray, David, Kolliakou, O'Connor, Di Forti and Fisher2016; Witt et al., Reference Witt, Munzer, Ganser, Fegert, Goldbeck and Plener2016). In light of this, various studies have highlighted the importance of exploring the effects of cumulative experiences of CM (also called complex trauma, polyvictimization, or multiple maltreatment) in relation to BPDs, rather than focusing on one type of maltreatment (Álvarez-Lister, Pereda, Abad, & Guilera, Reference Álvarez-Lister, Pereda, Abad and Guilera2014; Cecil, Viding, Fearon, Glaser, & McCrory, Reference Cecil, Viding, Fearon, Glaser and McCrory2017; Henschel, Doba, & Nandrino, Reference Henschel, Doba and Nandrino2018; VanMeter, Handley, & Cicchetti, Reference VanMeter, Handley and Cicchetti2020).
Despite a significant body of research confirming the deleterious effects of an adverse childhood family environment, the mechanisms through which these experiences might lead to later borderline psychopathology remain unclear, as this link is not always sufficient for the development of BPD (Bornovalova, Levy, Gratz, & Lejuez, Reference Bornovalova, Levy, Gratz and Lejuez2010). Regarding this question, Linehan's biosocial model considered the important role of interactions between biological vulnerabilities and environmental risk factors (Linehan, Reference Linehan1993a). Specifically, this model posits that BPD is a disorder of emotion dysregulation that emerges from interactions between an individual's vulnerability and negative environmental influences, such as an invalidating familial environment (Crowell, Beauchaine, & Linehan, Reference Crowell, Beauchaine and Linehan2009; Gratz, Moore, & Tull, Reference Gratz, Moore and Tull2016). Other models (e.g., Luyten & Blatt, Reference Luyten and Blatt2011), while acknowledging the important role of biological factors in disrupted personality development, posit that certain underlying personality structures within individuals with BPD may act as diatheses that render them particularly vulnerable to the effects of stressors (i.e., the poor quality of the childhood family environment) that are congruent with the underlying personality factors (Gunderson, Reference Gunderson2007; Kopala-Sibley & Zuroff, Reference Kopala-Sibley and Zuroff2014; Kopala-Sibley, Zuroff, Russell, Moskowitz, & Paris, Reference Kopala-Sibley, Zuroff, Russell, Moskowitz and Paris2012; Levy, Edell, & McGlashan, Reference Levy, Edell and McGlashan2007).
In line with this perspective, Blatt's two-configurations model of personality development and psychopathology (Blatt & Zuroff, Reference Blatt and Zuroff1992), starting from psychodynamic and cognitive developmental perspectives (Luyten & Blatt, Reference Luyten and Blatt2011), posits the role of personality dimensions in both mediating the effects of negative effects on psychopathology as well as intensifying the impact of negative events on psychopathology. Specifically, the two-configurations model (Blatt, Reference Blatt2008) argues that personality develops via a synergistic balance between two personality dimensions, relatedness and self-definition. However, disruptive environmental events such as CM may distort this developmental dialectical process, resulting in a rigid preoccupation with one of these dimensions. An overemphasis on issues of relatedness is the basis of a pathological trait that Blatt labeled dependency. In contrast, an overemphasis on issues of self-definition is the basis of a self-criticism trait (Blatt & Blass, Reference Blatt, Blass, Noam and Fischer1996). Dependency is characterized by intense feelings of loneliness, abandonment, helplessness, and weakness. Self-criticism is defined by the tendency to experience intense feelings of unworthiness, inferiority, failure, and guilt, and involves a tendency to adopt a punitive self-stance once standards are not met. A substantial body of evidence has supported this two-configurations models and supported links between self-criticism, dependency, and a range of psychopathologies (Blatt & Zuroff, Reference Blatt and Zuroff1992; Di Stefano, Scrima, & Perry, Reference Di Stefano, Scrima and Perry2019; Shahar & Priel, Reference Shahar and Priel2003).
The link between cumulative CM or poor-quality parenting and self-criticism and dependency has been demonstrated. For example, Campos, Besser, and Blatt (Reference Campos, Besser and Blatt2010) investigated the mediating role of the self-critical and dependent personality vulnerability traits in the link between perceived early experiences and depressive symptoms. They found that early relationships characterized by low levels of caring and high levels of overprotection are associated with higher levels of depression and self-criticism among adults. The results also indicated that high levels of self-criticism mediated the relationship between perceived early childhood experiences with the mother and current depression. Dunkley, Masheb, and Grilo (Reference Dunkley, Masheb and Grilo2010) examined the relations between various forms of CM (emotional, physical and sexual abuse, and emotional and physical neglect) and body dissatisfaction in binge eating disorder (BED) patients and tested a model in which self-criticism mediated the link between childhood maltreatment and body dissatisfaction in BED. Their findings indicated that the relations between childhood emotional abuse and body dissatisfaction in BED patients were fully mediated by the presence of a self-critical cognitive-personality style. Soffer, Gilboa-Schechtman, and Shahar (Reference Soffer, Gilboa-Schechtman and Shahar2008) found that those who experienced CM, such as insults, excessive criticism, or some form of physical abuse, may come to adopt a similarly critical view of themselves based on the behavior of those who criticized them, resulting in a self-critical personality style (see also, Glassman, Weierich, Hooley, Deliberto, & Nock, Reference Glassman, Weierich, Hooley, Deliberto and Nock2007; Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley and Verrocchio2018b). In their review of this literature, Kopala-Sibley and Zuroff (Reference Kopala-Sibley and Zuroff2014) confirmed that adverse childhood experiences, including maltreatment, are associated with elevated levels of self-criticism and dependency.
Although originally formulated as risk factors specifically for depression, self-criticism and dependency are associated with a wide range of mental disorders (Kopala-Sibley & Zuroff, Reference Kopala-Sibley and Zuroff2020). Blatt and Luyten (Reference Blatt and Luyten2009) noted that the form and expression of BPD could be influenced by individual differences in terms of self-criticism and dependency, such that highly self-critical individuals with BPD are more vulnerable to perceptions of inferiority, guilt, and failure, whereas those who are highly dependent are more vulnerable to perceptions of loneliness, abandonment, and emotional insecurity in their interactions with others (see also, Blatt & Auerbach, Reference Blatt and Auerbach1988). Kopala-Sibley et al. (Reference Kopala-Sibley, Zuroff, Russell, Moskowitz and Paris2012) found that more highly self-critical individuals with BPD showed increases in negative affect following perceptions of interpersonal inferiority during interpersonal interactions, while more highly dependent individuals with BPD showed increases in negative affect following perceptions of emotional insecurity during interpersonal interactions. A meta-analysis found that elevated depressive symptoms in BPD are associated with elevated self-criticism (Köhling, Ehrenthal, Levy, Schauenburg, & Dinger, Reference Köhling, Ehrenthal, Levy, Schauenburg and Dinger2015). Similarly, Westen et al. (Reference Westen, Moses, Silk, Lohr, Cohen and Segal1992) found that BPD subjects with and without major depression scored significantly higher in both dependency and self-criticism than subjects with major depression but no BPD, even after controlling for severity of depression. Finally, Levy et al. (Reference Levy, Edell and McGlashan2007) found high levels of dependency in patients with BPD and reported that dependency levels were associated with interpersonal distress, self-destructive behaviors, and impulsivity.
However, little is known about associations of cumulative CM as well as self-criticism or dependency with BPDs in adolescents, and no research has examined whether self-criticism or dependency may mediate or moderate the relationship between cumulative CM and BPDs. The current study aimed to examine, in a mixed sample of nonclinical and clinical adolescents, the relationship between cumulative CM and BPDs, and to examine whether the personality traits of self-criticism and dependency contribute to this relationship. The specific objectives were to: (a) identify vulnerable personality profiles by combining self-criticism and dependency scores; (b) examine whether specific personality vulnerability profiles of self-criticism and dependency might be related both to specific BPDs and multiple forms of CM; (c) test the potential mediating and moderating roles of vulnerable personality profiles in the relationship between cumulative experiences of CM and BPDs. We hypothesized that different profiles of personality vulnerabilities would emerge with high and low levels of self-criticism and dependency; vulnerable personality profiles of self-criticism and dependency would be significantly related both to multiple forms of CM and BPDs and would mediate the relationship between cumulative CM and BPDs. We also tested whether personality profiles moderate this latter association, although this analysis was exploratory given that no prior research, to our knowledge, has examined this issue.
Method
Participants
Two hundred and forty-one nonclinical and clinical adolescents (61.4% female) aged 13–20 years (Mage = 16.37, SD = 1.84) participated in the study. One hundred seventy-four nonclinical participants were randomly recruited from lists of local collaborating schools in central and southern Italy. Sixty-seven clinical adolescents (42 males and 25 females), characterized by having some form of substance abuse or other psychiatric diagnosis, were recruited from private and public therapeutic clinics in central Italy. Demographics for each group and the total sample are displayed in Table 1. Of the clinical sample, 43 (64.2%) were teens in middle adolescence (ages 13 to 17 years), while 24 (35.8%) were in late adolescence (18 to 20 years). Approximately 90% of them had a history of drug abuse (10.4% used no drugs) and nearly all those used cannabis (89.6%) alone (56.8%) or in combination with cocaine (23.9%) or, to a lesser extent (8.9%), with other substances (i.e., amphetamine, ketamine, and heroin). A Diagnostic and Statistical Manual of Mental Disorders (DSM)-based clinical diagnosis characterized 23 of the clinical adolescents (of the total 67 participants). This subsample showed mixed psychiatric disorders. Specifically, nine (39.1%) were diagnosed with a depressive or mood disorder, seven (30.4%) with an impulse control or conduct disorders, four (17.4%) with BPD, two (8.7%) with an anxiety disorder, and one (4.4%) with an eating disorder. Diagnoses were made by psychiatrists with at least 5 years of clinical experience in clinical assessments, by using the Structured Clinical Interview for DSM-5 (First, Williams, Karg, & Spitzer, Reference First, Williams, Karg and Spitzer2016). Approximately 85% of the clinical participants (57) were receiving some form of therapy during the data collection period: 49% participated in individual psychological/psychiatric psychotherapy, 6% in group psychotherapy, 4.5% followed pharmacological therapy, while 40.5% attended socio-educational rehabilitation therapy.
Table 1. Demographics and characteristics for the nonclinical adolescent sample, the clinical adolescent sample, and the total sample

a The proxy of socio-economic status was calculated based on adolescents’ evaluation of family economy and the education level of both parents individually
b The nonclinical subsample had significantly more married or cohabiting parents than the clinical sample, χ2 (1) = 32.90, p < .001
c The nonclinical adolescents were more likely to indicate their birth mother as the reference figure who brought them up in childhood, χ2 (1) = 10.50, p = .001
d The nonclinical adolescents were more likely to indicate their birth father as the reference figure who brought them up in childhood, χ2 (1) = 13.93, p < .001
e The clinical adolescents were more likely to experience parental loss, χ2 (1) = 31.50, p < .001
Procedure
The psychology department's ethics committee at the University of Chieti (Italy) approved this study and its procedures. Data were collected during school time for nonclinical participants or by appointment at the clinic for clinical participants. Parents’ and adolescents’ written informed consent was obtained prior to collecting data.
Measures
Socio-demographics
Participants were asked to indicate their gender, age, ethnicity, marital status, education and occupation, as well as their parents’ education and marital status. For each clinical adolescent, the reference person in the clinic was asked to specify the reasons for visiting the clinic as well as previous and current therapies.
Depressive experiences questionnaire
The Italian version of the Depressive Experiences Questionnaire (DEQ; Blatt, Schaffer, Bers, & Quinlan, Reference Blatt, Schaffer, Bers and Quinlan1992; Falgares et al., Reference Falgares, De Santis, Gullo, Carrozzino, Marchetti, Verrocchio and Oasi2017) adapted for adolescents was used to measure self-criticism and dependency. The DEQ consists of 66 self-reported items yielding factor scores for three primary factors: dependency, self-criticism, and efficacy. In this study, the efficacy subscale was not used as it was not expected to be a potential vulnerability factor associated with both CM and BPDs. Instead, the current study focuses on the subscales of dependency (example item: “I become frightened when I feel alone”) and self-criticism (example item: “I tend to be very critical of myself”) given their robust links to a range of psychopathologies. Items were scored on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). Scores for both dependency and self-criticism were obtained using the original factor score procedure of Blatt, D'Afflitti, and Quinlan (Reference Blatt, D'Afflitti and Quinlan1976). The Italian version of the DEQ showed good internal consistency and validity (see Falgares et al., Reference Falgares, De Santis, Gullo, Carrozzino, Marchetti, Verrocchio and Oasi2017; Falgares et al., Reference Falgares, De Santis, Gullo, Kopala-Sibley, Scrima and Livi2018a). In the present study, Cronbach's α was .81 in the nonclinical sample and .77 in the clinical sample (.81 pooling the samples together) for dependency, and .92 in the nonclinical sample and .90 in the clinical sample (.91 pooling the samples together) for self-criticism.
Borderline personality inventory
The Italian version of the 53-item Borderline Personality Inventory (BPI; Leichsenring, Reference Leichsenring1999; Fossati et al., Reference Fossati, Feeney, Maffei and Borroni2014a, Reference Fossati, Gratz, Maffei and Borroni2014b) was used to assess symptoms linked to BPD. The BPI is a self-report questionnaire based on Kernberg's concept of borderline personality organization (Kernberg, Reference Kernberg1981). Although originally developed to score responses dichotomously (as true or false; Leichsenring, Reference Leichsenring1999), updated versions of this measure score items on a 4-point Likert-type scale ranging from 1 (disagree strongly) to 4 (strongly agree) (Chabrol & Leichsenring, Reference Chabrol and Leichsenring2006; Fossati et al., Reference Fossati, Feeney, Maffei and Borroni2014a, Reference Fossati, Gratz, Maffei and Borroni2014b). The BPI contains subscales for assessing identity diffusion (12 items, e.g., “Sometimes, I feel that people and things around me are not real”), primitive defense mechanisms (eight items, e.g., “My feelings towards other people quickly change into opposite extremes”), impaired reality testing (five items, e.g., “I have seen strange figures or visions when nothing was really there”), and fear of fusion (eight items, e.g., “I feel smothered when others show deep concern towards me”). Each subscale is scored by summing the related items, with higher scores corresponding to greater levels of each BPDs. As suggested by Leichsenring (Reference Leichsenring1999) in the initial BPI validation study, the current study considered these subscales dimensionally (for a total of 33 items) in the main analyses. However, to obtain a descriptive categorial assessment of BPD, a total BPI score including an additional 18 items that measure impulsivity (i.e., problems of impulse control) and self-mutilation (i.e., suicide attempts or self-mutilating acts) was computed (score ranging from 51 to 204). We used this latter approach only to calculate the percentage of adolescents with marked BPDs both in the nonclinical and clinical samples (see Preliminary analyses section). Evidence for reliability and validity of BPI has been provided both in adult and adolescent participants (Chabrol & Leichsenring, Reference Chabrol and Leichsenring2006; Fossati et al., Reference Fossati, Feeney, Maffei and Borroni2014a, Reference Fossati, Gratz, Maffei and Borroni2014b; Leichsenring, Reference Leichsenring1999). In the present study, the Cronbach α values ranged from .72 to .83 for the four subscales across the nonclinical and clinical samples (from .90 to .92 pooling the samples together).
Childhood experience of care and abuse questionnaire
The Italian version of the Childhood Experience of Care and Abuse Questionnaire (CECA.Q; Bifulco, Bernazzani, Moran, & Jacobs, Reference Bifulco, Bernazzani, Moran and Jacobs2005) was used to assess adverse childhood experiences (before the age of 17 years for the older participants). The questionnaire incorporates sections on parental loss and reference figures in childhood as well as parental or reference figures’ lack of care (antipathy and neglect), and psychological, physical, and sexual abuse. Good internal consistency data for CECA.Q have been provided in different contexts, including Italy (e.g., Infurna et al., Reference Infurna, Brunner, Holz, Parzer, Giannone, Reichl and Kaess2016; Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley and Verrocchio2018b; Smith, Lam, Bifulco, & Checkley, Reference Smith, Lam, Bifulco and Checkley2002). A full description of CECA.Q scales and scoring is given elsewhere (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley and Verrocchio2018b). Here, we briefly illustrate the scales’ content and report some additional information about scoring and internal consistency.
Parental loss refers to either parental death or separation of 1 year or more owing to a parent moving and permanently living elsewhere in childhood. Scores range from 0 to 4, with higher scores indicating more severe loss during childhood.
Lack of care refers to mothers’ and fathers’, or surrogate parents’, antipathy and neglect toward their children. In both nonclinical and clinical samples, maternal (α = .82 and .77, respectively) and paternal (α = .81 and .80, respectively) antipathy scores were highly related (r = .44 and .53, respectively) and therefore averaged to provide a single indicator of parental antipathy. Similarly, maternal (α = .79 for both nonclinical and clinical samples) and paternal (α = 84 and .80, respectively) neglect scores were highly related (r = .42 and .40, respectively) and therefore averaged. Parental antipathy and neglect scores (r = .69 for nonclinical sample and .56 for clinical sample) were further averaged to provide a total score, with higher scores indicating more parental lack of care.
Psychological abuse refers to a highly controlling and domineering relationship of parental figures with the child. In both nonclinical and clinical samples, maternal (α = .81 and .86, respectively) and paternal (α = .83 and .86, respectively) psychological abuse scores were highly related (r = .61 and .46, respectively) and therefore averaged to provide a single indicator of parental psychological abuse, with higher scores indicating more parental psychological abuse. The final score, ranging from 0 to 102, was re-scaled using the square root to obtain a new score range of 0–10.10, as reported in a previous study (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley and Verrocchio2018b).
Physical abuse refers to violence toward the child by parents or other caregivers in the household. Scores were dichotomized with a score of 0 for absence of any episode of physical abuse and a score of 1 for presence of one or more of such episodes.
Sexual abuse refers to age-inappropriate physical contact or approach of a sexual nature by any adult to the child. Scores were dichotomized with a score of 0 for absence of any episode of sexual abuse and a score of 1 for presence of one or more of such episodes.
Statistical analysis
Five main steps characterized data analyses. First, we computed descriptive statistics for the key study variables and examined univariate and multivariate normality of the distributions. Second, within a person-centered approach, we identified profiles of dependency and self-criticism by cluster analyses based on factor scores obtained from DEQ subscales. We initially examined whether the best cluster solution was replicable in both the nonclinical and clinical samples. Following Gore's (Reference Gore, Tinsley and Brown2000; see also Aldenderfer & Blashfield, Reference Aldenderfer and Blashfield1984) two-step approach, we conducted hierarchical cluster analyses using Ward's method (Ward, Reference Ward1963) and based on squared Euclidian distances. We compared cluster solutions with two to six clusters on the basis of three criteria: theoretical meaningfulness of each cluster, parsimony, and explanatory power (i.e., the cluster solution had to explain approximately 50% of the variance in both dependency and self-criticism dimensions). Then, distributions of adolescents from nonclinical and clinical samples across the obtained profiles were compared by chi-square test. If both adolescent groups were distributed in similar proportions across the profiles, they were collapsed into a single group and a new cluster analysis was carried out using the same procedure. Ultimately, study participants were grouped by K-means cluster analysis procedures and standardized mean values of the DEQ grouping variables describing the characteristics of each identified profile were calculated. Validity of the final solution was checked via a multivariate analysis of variance (MANOVA) on the two DEQ dimensions by profile. We also tested the replicability of the final solution by splitting the sample into two random halves and reconducting the cluster analyses for each subsample. Levels of agreement were calculated using Cohen's (Reference Cohen1960) kappa.
Third, in order to examine how profiles of dependency and self-criticism were related to BPDs as well as CM, we performed two distinct multivariate analyses of covariance (MANCOVAs) with profiles and group belonging (nonclinical vs. clinical) as independent variables and BPI dimensions in one model, and CECA.Q dimensions in the other, as dependent variable. Age, gender (0 = male 1 = female), parental loss, socioeconomic status (dummy coded: 0 = low-medium; 1 = medium-high), parent's marital status (dummy coded: 0 = cohabiting; 1 = not cohabiting), and parents’ educational level (dummy coded: 0 = at most one of parents with high school diploma; 1 = both parents with at least high school diploma) were entered as covariates.
Fourth, to explore the mediating role of profiles of dependency and self-criticism in the relationship between cumulative forms of CM and BPDs, we conducted a structural equation modeling (SEM) analysis with continuous latent (cumulative CM and BPDs) and categorical mediation variables (see Results section for the specific approach). After reporting bivariate correlations for the main variables, we tested the a priori model linking cumulative CM with BPDs via profiles of dependency and self-criticism. We used the robust weighted least squares estimation method within Mplus 7.2 (Muthén & Muthén, Reference Muthén and Muthén2014). Model invariance across nonclinical versus clinical samples and indirect effects were assessed. We based the model fit evaluation on multiple criteria (see Faraci & Musso, Reference Faraci, Musso, Barbaranelli and Ingoglia2013; Kline, Reference Kline2010). Reasonably good fit was supported when the chi-square (χ2) test value was associated with p > .05, comparative fit index (CFI) value was close to or greater than .95, root mean squared error of approximation (RMSEA) value was close to or less than .06, RMSEA 90% confidence interval (CI) values were below .05 for the lower bound and below .08 for the upper bound, and the weighted root mean square residual (WRMR) value was close to or less than 1.00. For nested model comparisons, the chi-square difference test (Δχ2) was used to test the difference in fit between less restrictive and more restrictive models.
Fifth, to explore the moderating role of profiles of dependency and self-criticism on the relation between cumulative forms of CM and BPDs, we performed a multiple-group SEM analysis with the profiles of dependency and self-criticism as the grouping variable. In this case, the a priori model was tested using the Satorra-Bentler (S-B) robust maximum likelihood estimation method. Fit criteria were the same as for the mediation model, with the exception that the standardized root mean square residual (SRMR) replaced the WRMR and needed to be less than .10.
Results
Preliminary analyses
Physical abuse and sexual abuse showed many observations equal to 0 in the nonclinical sample. This resulted in a not-positive definite covariance matrix in the covariance structure analyses. Thus, physical abuse and sexual abuse were summed to form a composite index of “physical and sexual abuse” ranging from 0 to 2. Furthermore, as there were few missing values in both nonclinical and clinical samples (4.6% and 4.5%, respectively), these were imputed at item level using the regression estimation function in the Statistical Package for the Social Sciences (SPSS) version 24. This approach allowed us to use all the data in analyses. Tables 2 and 3 summarize the descriptive statistics for the entire sample as well as separately for nonclinical and clinical samples. All variables showed univariate and multivariate normality (see George & Mallery, Reference George and Mallery2016).
Table 2. Prevalence of childhood maltreatment and borderline personality disorder (with score range in brackets) calculated as the percentage of participants exceeding the cut-off scores: moderate/marked levels for childhood maltreatment and marked level for borderline personality disorder symptoms

Note: The differences between the percentages of nonclinical versus clinical sample were significant for lack of care, χ2 (1) = 18.96, p < .001, and physical and sexual abuse, χ2 (1) = 21.08, p < .001, but not for BPD psychopathology, χ2 (1) = 1.79, p = .18. BPD = borderline personality disorder; CM = childhood maltreatment
a See Bifulco et al., Reference Bifulco, Bernazzani, Moran and Jacobs2005. For lack of care we considered the lowest cut-off between antipathy (≥25) and neglect (≥22)
b See Fossati et al., Reference Fossati, Gratz, Maffei and Borroni2014b
Table 3. Means, standard deviations, skewness, and kurtosis for the key study variables (with score range in brackets) in the entire sample as well as in the nonclinical and clinical samples

Min. stand. = minimum value of standardized score; Max. stand. = maximum value of standardized score
Profiles of dependency and self-criticism
Based on the a priori criteria, in both nonclinical and clinical samples, a three-cluster solution was the most acceptable. Solutions with two clusters explained less than 50% of variability in both the grouping dimensions, while solutions with four, five, and six clusters violated the principle of parsimony because they included clusters that represented slight variations of other clusters. Findings also indicated that the three-cluster solution that emerged in both nonclinical and clinical samples were highly comparable. Examining the distributions of adolescents from the two samples across the three paired profiles by chi-square test, no significant differences emerged, χ2 (2) = 0.53, p = .77. Thus, in the two samples the adolescents were distributed in similar proportions across the three profiles. We therefore combined data across nonclinical and clinical samples.
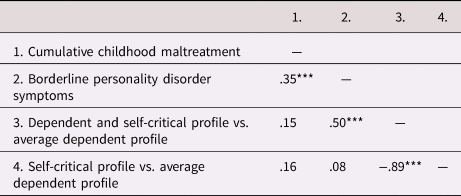
In the combined sample, a three-cluster solution emerged as the most acceptable, closely resembling the solutions found in each single sample. This solution was therefore used to cluster participants into three groups by K-means cluster analysis. The obtained profiles are shown in Figure 1. Using a cutoff of ± 0.30 to distinguish between above and below average mean z-scores (see, for example, Inguglia & Musso, Reference Inguglia and Musso2015), the first cluster (n = 72; 29.9%) consisted of adolescents showing average mean z-scores on dependency and mean z-scores below average on self-criticism. The second cluster (n = 96; 39.8%) was comprised of individuals showing mean z-scores above average on both dimensions. The third cluster (n = 73; 30.3%) was primarily composed of adolescents showing mean z-scores above average on self-criticism and mean z-scores below average on dependency. Thus, we found, in sequence, clusters representing an average dependent and low self-critical profile, a both highly dependent and highly self-critical profile, and a highly self-critical but low dependency profile, which we referred to as the average dependent profile, dependent and self-critical profile, and self-critical profile, respectively.
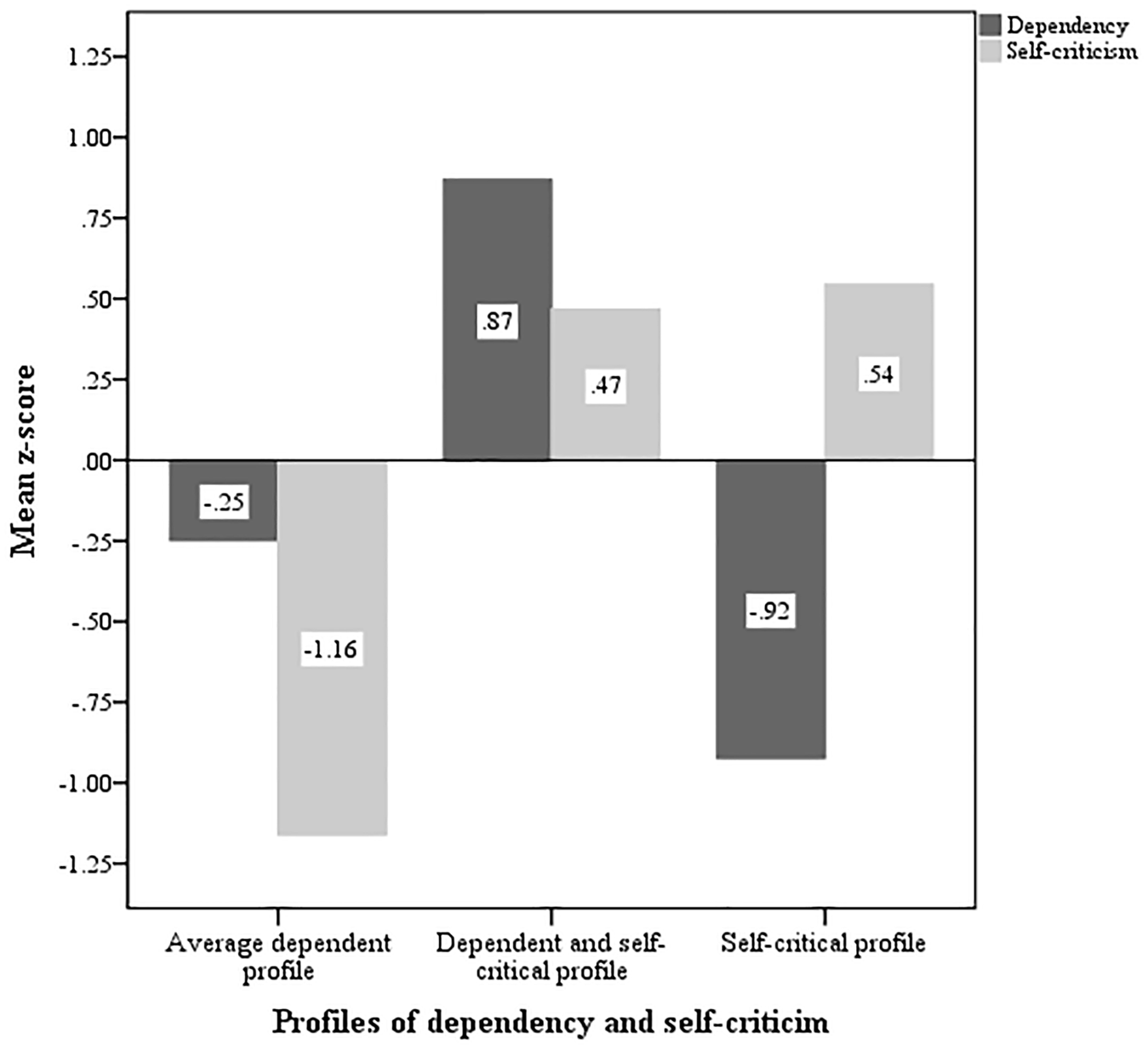
Figure 1. Z-scores for dependency and self-criticism for the three obtained profiles. Note: For descriptive purposes, a cutoff value of ± 0.30 was used to distinguish between above and below average mean z-scores (see, for example, Inguglia & Musso, 2015).
As a validity check on this three-cluster solution, results from MANOVA indicated that the three-cluster solution explained substantial percentages of variance (58% of variability in dependency and 59% in self-criticism). The same three clusters were replicated in each of the two random subsamples previously drawn. Levels of agreement between the classification performed in the total sample and those conducted in both the nonclinical and clinical samples as well as in the two random subgroups ranged from .75 to .81, indicating good reliability. Finally, we again examined the distributions of adolescents from both the nonclinical and clinical samples across the three profiles (see Table 4) with no significant differences obtained, χ2 (2) = 1.27, p = .53.
Table 4. Percentages of participants in the profile of dependency and self-criticism by sample

Associations between BPDs and profiles of dependency and self-criticism
Results from the MANCOVA showed a significant multivariate effect of profiles of dependency and self-criticism, Wilks’ Lambda = .77, F (8, 452) = 7.85, p < .001, η2 = .12. None of the other main and two-way effects were statistically significant. Follow-up univariate analyses indicated that all the dependent variables differed significantly across profiles, except for impaired reality testing (see Table 5). Pairwise comparisons revealed that adolescents in the average dependent profile reported significantly lower levels of identity diffusion, primitive defense mechanisms, and fear of fusion than their peers in the other two profiles. Moreover, adolescents in the self-critical profile scored significantly lower on identity diffusion and primitive defense mechanisms than those in the dependent and self-critical profile. No other significant differences were found.
Table 5. Univariate analyses of covariance and pairwise comparisons for the three profiles of dependency and self-criticism on the borderline personality disorder symptoms

Note: A profile mean is significantly different (p < .05) from another mean within the same row if they have different superscripts (a, b, or c). ***p < .001. MANCOVA = multivariate analyses of covariance
Associations between CM and profiles of dependency and self-criticism
Results from the MANCOVA showed significant multivariate effects of both profiles of dependency and self-criticism, Wilks’ Lambda = .93, F (6, 454) = 2.75, p < .05, η2 = .04, and group belonging, Wilks’ Lambda = .92, F (3, 227) = 7.01, p < .001, η2 = .08. Two-way effects were not statistically significant. Follow-up univariate analyses indicated that all the dependent variables differed significantly across profiles and group belonging (see Table 6). Specifically, pairwise comparisons revealed that adolescents in the average dependent profile reported significantly lower levels of lack of care, psychological abuse, and physical and sexual abuse than their peers in the other two profiles. No significant differences were found between adolescents in the self-critical profile and the dependent and self-critical profile. Moreover, adolescents in the nonclinical group scored significantly lower on lack of care, psychological abuse, and physical and sexual abuse than those in the clinical group.
Table 6. Univariate analyses of covariance and pairwise comparisons for the three profiles of dependency and self-criticism as well as the two groups of belonging (nonclinical vs. clinical) on the different forms of childhood maltreatment

Note: A profile mean is significantly different (p < .05) from another mean within the same row if they have different superscripts (a, or b). *p < .05, **p < .01, ***p < .001. MANCOVA = multivariate analyses of covariance
Mediation of the associations of cumulative CM with BPDs by personality profiles
The theoretical mediation model to be tested is illustrated in Figure 2. Lack of care, psychological abuse, and physical and sexual abuse were modelled to form the latent factor of cumulative CM. Identity diffusion, primitive defense mechanisms, impaired reality testing, and fear of fusion were modelled to form the latent factor of BPDs. BPDs was indirectly predicted by cumulative CM via the profiles of dependency and self-criticism.

Figure 2. The theoretical mediation model.
Because the dependency and self-criticism profile variable was multicategorical, we used a dummy coding strategy to represent the groups in the model (see Hayes & Preacher, Reference Hayes and Preacher2014). Table 7 shows the indicator coding system, where the average dependent profile was not explicitly coded; that is, all the k-1 dummy variables (k denotes the total number of categories) were set to 0 for cases in that group. Thus, the average dependent profile functioned as the reference group in the analysis and parameters interpreted relative to this reference group.
Table 7. Indicator coding system for profiles of dependency and self-criticism

Note: As the reference group, the average dependent profile was not explicitly coded; that is, all the k-1 dummy variables (k denotes the total number of categories) were set to 0 for cases in that group
We initially estimated a SEM specifying all the covariances among the key latent (cumulative CM and BPDs) and dummy variables to obtain bivariate correlations for the entire sample (see Table 8). This model had good fit, χ2 (23) = 26.72, p = .26, CFI = .990; RMSEA = .026 [90% CI = .000–.061], WRMR = .468. Then, we tested the mediation model, inserting the dummy variables as full mediators of the relation between cumulative CM and BPDs and controlling for age, gender, parental loss, socioeconomic status, parents’ marital status, and parents’ educational level. As suggested by both the findings from the MANOVA (see Table 6) and bivariate correlations (see Table 8), we also constrained the pathways from cumulative CM and the two dummy variables to be equal. The model fit was excellent, χ2 (77) = 70.36, p = .69, CFI = 1.00; RMSEA = .000 [90% CI = .000–.030], WRMR = .602. Moreover, the model was invariant across nonclinical versus clinical samples: when performing the analyses within a multigroup SEM framework imposing cross-group equality constraints for all the factor loadings, pathways, and covariances, the fit was excellent, χ2 (183) = 180.18, p = .54, CFI = 1.00; RMSEA = .000 [90% CI = .000–.038], WRMR = 1.044, and not worse than the unconstrained model, Δχ2 (19) = 21.04, p = .33. The final model with standardized parameter estimates is shown in Figure 3. Some parameter estimates exceeded the value of 1. This is because parameters in such models can represent group differences relative to the reference group (Hayes & Preacher, Reference Hayes and Preacher2014).
Table 8. Bivariate correlations among key latent and dummy variables for the entire sample (N = 241), after estimating a structural equation model specifying all covariances among variables
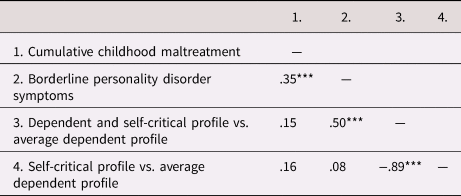
*** p < .001

Figure 3. Estimated mediation model. Note: The key study variables and their related pathways are presented in black. The measurement part of themodel (including observed indicators and factor loadings) as well as control variables and their related significant paths are presented in gray. Solid lines represent significant pathways, dashed lines are nonsignificant. Standardized regression coefficients (betas) are shown. For better visualization, nonsignificant correlations among control variables and residuals are not shown. **p < .01, ***p < .001.
Findings showed that cumulative CM was significantly and positively associated with the two dummy variables, meaning that adolescents in the dependent and self-critical as well as the self-critical profiles experienced more cumulative CM relative to the adolescents in the average dependent profile. The two dummy variables were significantly and positively related to BPDs. That is, adolescents in the dependent and self-critical as well as the self-critical profiles showed greater BPDs compared with adolescents in the average dependent profile. Moreover, the indirect effect between cumulative CM and BPDs through the dummy variables was significant and positive (β = .19, p < .001, 95% CI = .11–.28, through the dependent and self-critical profile vs. average dependent profile variable and β = .16, p < .001, 95% CI = .09–.23, through the self-critical profile vs. average dependent profile variable), meaning that the group differences between the two dummy variables and the reference group mediated the association of cumulative CM and BPDs. Thus, relative to the average dependent profile, higher cumulative CM was linked to a higher probability of belonging to the dependent and self-critical or the self-critical profiles and, in turn, this was associated with higher level of BPDs.
We also replicated the analysis using the self-critical profile as the reference group for the dummy variables. Based on previous results, the pathways from cumulative CM and the two dummy variables were free to be estimated. This model again showed excellent fit, χ2 (76) = 78.04, p = .41, CFI = .995; RMSEA = .011 [90% CI = .000–.038], WRMR = .654, and was invariant across samples, χ2 (182) = 194.92, p = .24, CFI = .973; RMSEA = .024 [90% CI = .000–.048], WRMR = 1.114, Δχ2 (20) = 31.60, p = .05. Cumulative CM was significantly and negatively associated only with the average dependent profile versus self-critical profile dummy variable, meaning that adolescents in the average dependent profile reported fewer cumulative CM experiences than the adolescents in the self-critical profile, while no significant differences emerged between adolescents in the dependent and self-critical profile and those in the reference group in terms of cumulative CM (see Figure 3). A similar pattern was found in relation to BPDs. That is, adolescents in the average dependent profile showed lower BPDs compared with adolescents in the self-critical profile, but no significant differences were found between adolescents in the dependent and self-critical and those in the reference group. Moreover, the only significant indirect effect between cumulative CM and BPDs was through the average dependent profile versus self-critical profile dummy variable (β = .42, p < .001, 95% CI = .05–.78), meaning that the association of cumulative CM and BPDs was mediated by only the group differences between the average dependent profile and the reference group. Thus, relative to the self-critical profile, higher levels of cumulative CM were linked to a lower probability of belonging to the average dependent profile and, in turn, this was associated with lower BPDs, while no significant differences emerged in the dependent and self-critical profile group in the patterns of associations. Thus, participants who were highly self-critical or both highly self-critical and dependent experienced similar amounts of cumulative CM and showed comparable levels of BPDs.
Associations of cumulative CM with BPDs: Moderation by profiles of self-criticism and dependency
The theoretical moderation model to be tested is illustrated in Figure 4. The initial model specifying the pathway from cumulative CM to BPDs for the entire sample had very good fit, χ2S-B(13) = 12.87, p = .46, CFI = 1.00; RMSEA = .000 [90% CI = .000–.063], SRMR = .029. The standardized regression coefficient (β) was .35, p < .001. We then tested the moderation model comparing the three profile groups with respect to this link after controlling for age, gender, parental loss, socioeconomic status, parent's marital status, and parents’ educational level. The unconstrained moderation model, in which cross-group equality constraints were imposed only for the factor loadings, showed an acceptable fit to the data, χ2S-B(203) = 230.88, p = .09, CFI = .949; RMSEA = .041 [90% CI = .000–.065], SRMR = .087. The completely constrained version of this model, also imposing equality constraint for the pathway between cumulative CM and BPDs across the three profile groups, did not significantly differ from the fit of the unconstrained model, χ2S-B(205) = 230.84, p = .10, CFI = .952; RMSEA = .040 [90% CI = .000–.064], SRMR = .088, Δχ2S-B(1) = 0.08, p = .96. These findings showed no significant moderating role of profiles of dependency and self-criticism in the link between cumulative CM and BPDs.

Figure 4. The theoretical moderation model.
Discussion
The present study examined the association between cumulative forms of CM and borderline psychopathology features, thereby contributing to a growing literature that recognizes a distinction between BPD primarily characterized by elevated self-criticism versus dependency or both (Blatt & Luyten, Reference Blatt and Luyten2009; Levy et al., Reference Levy, Edell and McGlashan2007). After identifying three personality profiles by combining self-criticism and dependency, we examined the relationships between these profiles and multiple forms of CM and BPDs. Finally, we tested the mediating and moderating roles of profiles of dependency and self-criticism in the relationship between cumulative CM and BPDs.
Consistent with hypotheses, different personality profiles with high and low levels of dependency and self-criticism emerged. One such profile represented adolescents with average dependency and low self-criticism. A second profile comprised adolescents with high self-criticism but low dependency. A third profile represented adolescents with both high dependency and self-criticism. This last group showed the most severe BPDs as indicated by high levels of identity diffusion and primitive defense mechanisms. This may indicate that being self-critical and dependent is associated with greater or more severe BPDs compared with being only highly self-critical. This is consistent with previous evidence that individuals presenting an elevated polarization with both relatedness and self-definition issues present more severe borderline psychopathological manifestations than individuals that develop only either dependent (i.e., focused on relatedness issues) or self-critical (i.e., focused on autonomy and self-definition concern) traits (Blatt, Quinlan, Chevron, McDonald, & Zuroff, Reference Blatt, Quinlan, Chevron, McDonald and Zuroff1982; Campos, Holden, Baleizão, Caçador, & Fragata, Reference Campos, Holden, Baleizão, Caçador and Fragata2018; Falgares et al., Reference Falgares, De Santis, Gullo, Kopala-Sibley, Scrima and Livi2018aa; Shahar, Blatt, & Ford, Reference Shahar, Blatt and Ford2003).
There were no significant differences between adolescents in the self-critical profile and the dependent and self-critical profile in terms of CM experiences, while the average dependent adolescents reported the lowest levels of CM experiences. It is therefore possible that multiple forms of CM (i.e., lack of care, psychological abuse, and physical and sexual abuse) predict the development of a vulnerability pertaining to self-definition issues that may or may not be accompanied by a preoccupation toward attachment issues. This finding is in line with the concept of multifinality, in that different adverse outcomes may stem from similar developmental experiences (Cicchetti & Rogosch, Reference Cicchetti and Rogosch1996). This finding is also consistent with the conclusions from Kopala-Sibley and Zuroff's (Reference Kopala-Sibley and Zuroff2014) review in which they found non-specific links between a range of adverse parenting behaviors (e.g., criticism, coldness, psychological control, maltreatment) and the development of both self-criticism and dependency.
Further analyses examined whether vulnerable personality profiles mediated the relationship between cumulative CM and BPDs. Cumulative CM was significantly associated with both self-critical and dependent and self-critical profiles. These two profiles were both positively related to BPDs. The two vulnerable personality profiles then mediated the association between CM and BPDs. Thus, relative to the average dependent personality profile, higher levels of CM were linked to a higher probability of belonging to the dependent and self-critical or the self-critical profiles and in turn this was associated with higher level of BPDs. This finding is intriguing because it suggests that exposure in childhood to multiple and cumulative types of maltreatment during childhood may lead to different personality vulnerability profiles both in terms of a tendency to internalize a critical attitude toward the self (self-criticism) and intense feelings of loneliness, abandonment, helplessness, and weakness (dependency). Thus, consistent with Blatt's (Reference Blatt2008) theory, self-criticism and dependency may be considered interrelated given they both stem in part from adverse childhood experiences, co-occur, and confer risk for psychopathology such as BPDs. It is therefore possible that cumulative CM may have disrupted the dialectic interaction between relatedness and self-definition personality domains that may in turn result in an exaggerated or distorted preoccupation with issues regarding one's own identity (self-definition). Since the development in each personality domain is believed to be interrelated (Blatt, Reference Blatt2008), elevated self-criticism may affect individuals’ ability to establish mature forms of interpersonal relatedness, resulting in a tendency towards feelings of abandonment and loss and therefore high dependency (Luyten & Blatt, Reference Luyten and Blatt2011).
Personality profiles, however, did not moderate the effects of cumulative CM on BPDs. This suggests that self-criticism and dependency may be outcomes of CM, rather than independent factors that exacerbate the effects of CM on BPDs. Consistent with Blatt's theory of personality development, self-criticism and dependency are, at least in part, the result of a disruption in a balanced developmental process that is likely related to the quality of early childhood experiences (Luyten & Blatt, Reference Luyten and Blatt2011). Thus, personality characterized by varying levels of self-criticism and dependency may be important to consider in the process of identifying and understanding underlying mechanisms that link maltreatment experienced during childhood to borderline manifestations assessed in adolescence.
Given BPD is increasingly seen as a life-span developmental disorder represented on a dimensional continuum of severity (Kaess et al., Reference Kaess, Brunner and Chanen2014) with stable features in adolescence and adulthood (Chanen, Jovev, McCutcheon, Jackson, & McGorry, Reference Chanen, Jovev, McCutcheon, Jackson and McGorry2008), understanding how personality profiles may intervene in the development of early manifestations in adolescents who reported a single or multiple form of CM may have implications for early intervention. Concerning prevention and treatment for these adolescents presenting BPDs, it is worthwhile to consider early maltreatment, which may not always be examined in everyday clinical practice. When present, trauma-focused therapies may be indicated. Cognitive behavioral therapy (CBT) approaches may be useful in targeting self-critical and dependent personalities. For example, self-criticism has been successfully treated with compassion focused therapy (Kannan & Levitt, Reference Kannan and Levitt2013; Kelly & Carter, Reference Kelly and Carter2015; Sommers-Spijkerman, Trompetter, Schreurs, & Bohlmeijer, Reference Sommers-Spijkerman, Trompetter, Schreurs and Bohlmeijer2018). Schema therapy or CBT that targets maladaptive core beliefs could be useful for targeting self-criticism and dependency as well. When the development of BPDs are rapid and severe (with the possibility of self-harm or suicidal behaviors) dialectical behavior therapy techniques (Linehan, Reference Linehan1993b), including multifamily groups, may also be recommended to target self-definition and relatedness issues. Theoretical and empirical contributions (Blatt & Luyten, Reference Blatt and Luyten2009; Safran & Muran, Reference Safran and Muran2000; Blatt, Zuroff, Hawley, & Auerbach, Reference Blatt, Zuroff, Hawley and Auerbach2010) support the view that sustained therapeutic change may involve the reactivation of the normal developmental processes that proceed through a dialectical balance between attachment and autonomy domains in which the therapeutic relationship supports changes in the sense of self that lead to a more mature expression of interpersonal closeness that in turn contributes to further refinement in the sense of self.
Limitations and future directions
Several limitations of this study should be noted. First, whether CM influences change over time in personality or BPDs, or whether personality influences change over time in BPDs cannot be examined owing to the cross-sectional design. Cross-sectional data cannot identify the direction of effects or causal links. Second, the study used only self-report measures, which may be sensitive to social desirability and can inflate some of the associations among variables owing to shared method variance. Future research should use a multiple method approach, including interviews. Third, the distribution of our participants by gender was unbalanced both within and across groups; in the nonclinical sample gender was unbalanced at approximately a ratio of 3.4:1 for females to males, while in the clinical sample there was approximately a 2.7:1 ratio of males to females. Both nonclinical and clinical samples were composed of Italian adolescents who predominantly came from middle-class backgrounds. These are issues that could bias results and limit generalizability. Replication of our findings with more heterogenous samples in terms of gender, socioeconomic status, and culture would therefore foster generalization of findings to broader populations.
Despite these limitations, our data advance our understanding of the relationship between multiple forms of CM and BPDs by examining the role of personality profiles emerging from a combination of dependency and self-criticism traits. Future research may benefit from considering dependency and self-criticism in the development of BPDs by investigating the interaction with recognized heritable traits, such as emotional vulnerability and impulsivity (Crowell et al., Reference Crowell, Beauchaine and Linehan2009; Gratz et al., Reference Gratz, Moore and Tull2016; Kendler et al., Reference Kendler, Aggen, Czajkowski, Røysamb, Tambs, Torgersen and Reichborn-Kjennerud2008). Research suggests both Gene × Environment interactions and correlations in the development of BPD (Distel et al., Reference Distel, Middeldorp, Trull, Derom, Willemsen and Boomsma2011). An investigation of genetic factors was beyond the scope of this study and, therefore, we cannot exclude the role of predisposing factors that confer a biological vulnerability through which negative childhood experiences contribute to the development of personality vulnerabilities. Even though knowledge of developmental pathways to BPD has increase substantially in the last decade, we do not yet have a detailed understanding of the role of Gene × Environment interactions in the development of BPD in adult and adolescent populations (Kaess et al., Reference Kaess, Brunner and Chanen2014). Future research on emotional dysregulation, early negative experiences, and BPD may benefit from behavioral genetic research and from considering personality profiles as a vulnerability factor as a potential mechanism through which negative early experiences influence later BPD pathology.
Funding Statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.