Few areas of the study of relationships between race, ethnicity and health are more controversial than the association between serious criminal behaviour and severe mental illness. There are approximately 3000 secure beds in England and Wales for the treatment of mentally disordered offenders and patients who cannot be managed in ordinary psychiatric hospitals. These are in three special (maximum security) hospitals and a network of National Health Service (NHS) and private units which offer medium security. Most patients are compulsorily detained under Part III of the Mental Health Act 1983, following convictions for violent, sexual, or arson offences. A subgroup are detained under Part II of the Act, following noncriminalised but highly difficult or dangerous behaviour. It has become increasingly apparent that a disproportionate number of patients detained in secure psychiatric facilities is of African-Caribbean origin (Reference MurrayMurray, 1996).
Concerns over the differential representation of ethnic subgroups in the criminal justice process have been highlighted in the USA, where one in three African American men between the ages of 20 and 29 were under some form of criminal justice supervision (prison, probation, or parole) in 1994. Overall, African American men were estimated to be imprisoned at a rate six times that of White men (Reference DonzigerDonziger, 1996). However, Black adult males in the UK of African and Caribbean origin were imprisoned at 6.7 times the age-adjusted rate of White males in 1991, and show especially high rates of imprisonment for rape, robbery and drug offences (Home Office, 1992). A criminological review has concluded that “although some bias against Black people has been demonstrated at several stages of the process, and although some decision-making criteria clearly work to the disadvantage of Black people, in large part the difference in rates of arrest and imprisonment between Black and White people arises from a difference in the rate of offending”. Furthermore, persons of Indian, Pakistani and Bangladeshi origin are not over-represented among offenders (Reference Smith, Maguire, Morgan and ReinerSmith, 1997).
There is evidence that the overall demand for psychiatric service provision may be especially high in areas characterised by higher proportions of African-Caribbeans (Reference McGovern and CopeMcGovern & Cope, 1987; Reference Harrison, Holton and NeilsonHarrison et al, 1988; Reference Owens, Harrison and BootOwens et al, 1991; Reference Davies, Thornicroft and LeeseDavies et al, 1996; Reference Ineichen, Harrison and BootIneichen et al, 1996; Reference Bhugra, Leff and MallettBhugra et al, 1997; Reference Harrison, Glazebrook and BrewinHarrison et al, 1997; Reference McCreadie, Leese and Tilak-SinghMcCreadie et al, 1997). Independent of their diagnosis, Black African-Caribbean patients are more likely to have contact with the police and forensic services (Reference McGovern and CopeMcGovern & Cope, 1987), to be treated in intensive care facilities if detained under the Mental Health Act (Reference Moodley and ThornicroftMoodley & Thornicroft, 1988), and to have criminal convictions if they are young and male (Reference Wessely, Castle and DouglasWessely et al, 1994). The 1991 census provided detailed information about the population in the United Kingdom and for the first time included data on ethnic group (Reference Balarajan and RaleighBalarajan & Raleigh, 1992). We therefore studied the prevalence rates of treated mentally disordered offenders, and other patients requiring secure forensic services, from within a defined geographical area comprising half of England and Wales over a 7-year period. We compared standardised admission ratios between ethnic groups and examined factors that had led to their admission to these services.
METHOD
We recorded details of all admissions to secure forensic psychiatry services over a 7-year period (1988-1994) from seven of the 14 (pre-reorganisation) Regional Health Authorities: North East and North West Thames, South Western, West Midlands, East Anglian, Merseyside, and North Western regions. The intention was to cover a widely representative range of geographical areas: large urban, smalltown, semi-rural and rural areas, characterised by different levels of social deprivation. During the study, certain medium secure services did not have sufficient beds and a proportion of admissions were to the independent sector or other NHS units on an extracontractual referral basis. These admissions were included so as not to under-represent these areas. As there was no centralised database, each special hospital, independent sector hospital, or medium secure unit was visited and item sheets completed on each admission from the case notes.
Catchment area of origin was coded according to the patient's most recent address, from their 1991 postal code. Patients who had no fixed abode, or for whom no accurate details of address could be obtained, were omitted from the study. Data were recorded by a clinically trained research psychiatrist (N.K.) and included: demography; criminal behaviour and non-criminal behaviour disorder leading to admission; diagnosis (including personality disorder); and the source and nature of referral. The integrity of data in the case notes was generally high and an almost complete data-set was compiled from them. Ethnic group was assigned by the researcher using the Office of Population Censuses and Surveys' (now Office for National Statistics) classification (Reference SillitoeSillitoe, 1987). For the study analysis, this classification was simplified into four categories: White, Black (including Black Caribbean, Black African, Black Other), Asian (including Indian, Pakistani, Bangladeshi, but excluding Chinese and Asian Other), or Other (all other categories).
We used the Jarman Underprivileged Area Score (UPA) (Reference JarmanJarman, 1983) distributions to position admissions within UPA deciles, based upon the distribution of UPA, which was based on postal code of address within electoral wards in the relevant seven regions. As the subjects who were of prime interest in this study largely comprised the group that suffered most from under-enumeration in the census (i.e. young males), revised population statistics were used which allowed for both geographical and age/gender variations in the under-enumeration (Reference Simpson, Cossey and DiamondSimpson et al, 1997).
Statistical analysis
Analyses were carried out only on first admissions to the forensic services during the 7-year period. Some medium secure units readmitted larger proportions of their patients than did others, reflecting different patterns of service provision. Crude overall male and female admission rates were calculated for each UPA decile, by age and by gender. These were taken as the expected admission rates for the population as a whole. Expected admissions were then calculated for each ethnic group, based on the expected rates and the estimated populations split by ethnic group. The combination of expected and actual admissions was then used to calculate standardised admission rates for each of the ethnic, age and gender groups and for the ethnicity/gender groups overall.
Logistic regression was used to model the treated prevalence over the 7-year study period using gender, age, whether UK-born, marital status, UPA decile derived from address at ward level, and whether the primary diagnosis was personality disorder, as independent variables. Odds ratios (OR) with 95% confidence intervals (CI) were used to measure differences between the Black and Asian ethnic groups compared to White subjects, according to independent variables of criminal behaviour and behavioural disorder leading to admission, previous criminal history, previous institutional history, the source of referral for admission, and lifetime diagnoses.
RESULTS
Number of admissions and time series
Between 1 January 1988 and 31 December 1994, there were a total of 3155 first admissions to maximum and medium secure forensic psychiatry services in England from the seven regions. No data could be obtained on 18 additional patients, and 164 (5%) were of no fixed abode, or insufficient details were available about them to obtain a postal code. There were no differences between ethnic subgroupings in the subjects excluded. Three additional subjects could not be coded for ethnicity. The proportions of subjects included in the study, according to our defined ethnic groupings, were 2358 (74%) White, 656 (21%) Black, 81 (3%) Asian, and 57 (2%) Other.
Figure 1 demonstrates a proportional rise in the number of non-White, relative to White, patients from 1991 onwards. The proportion of admissions of non-Whites remained approximately constant at 23% from 1988 to 1990 (χ2 for trend, P=0.003).
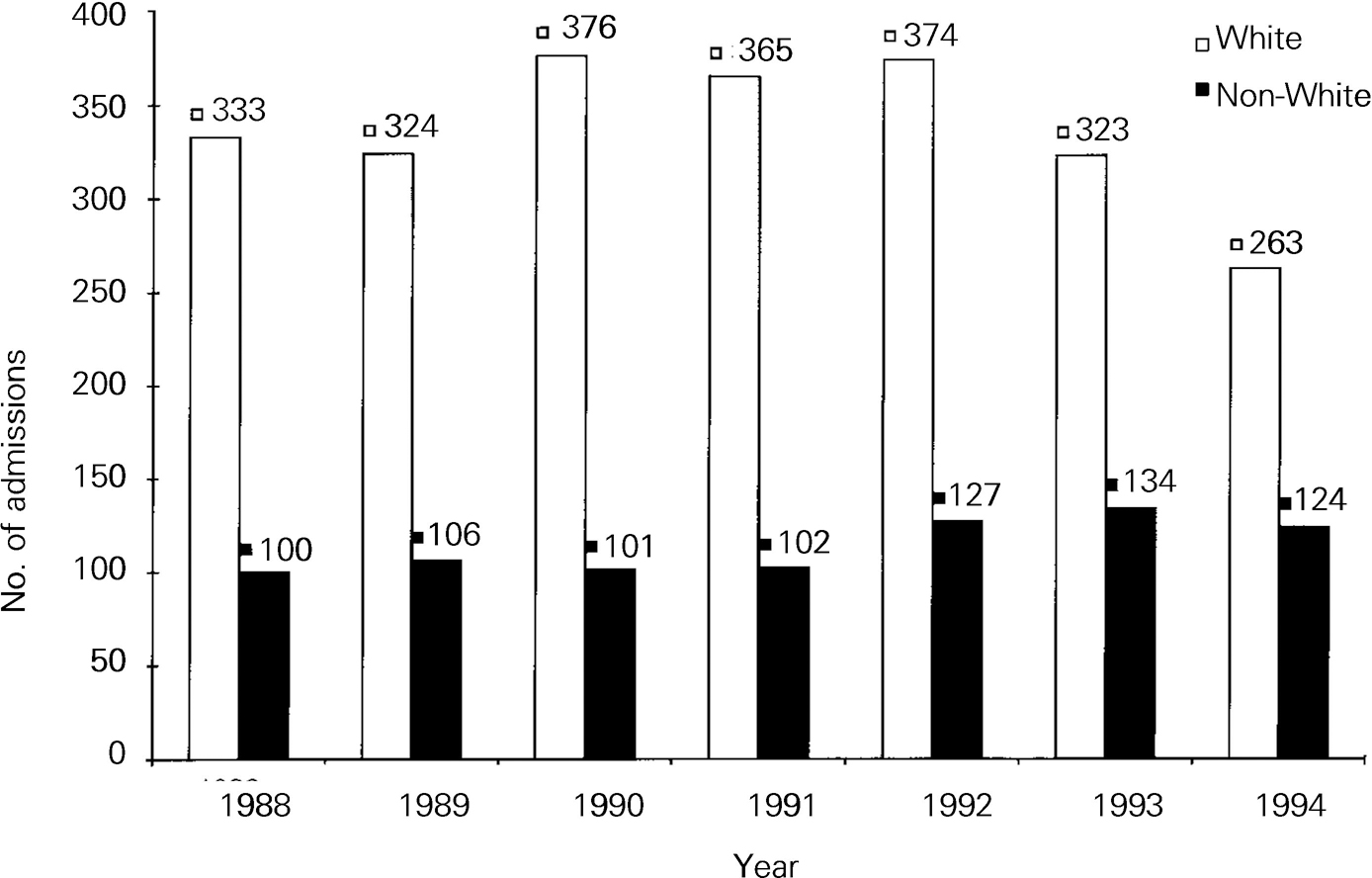
Fig. 1 Annual first admissions of White and non-White patients to maximum and medium security, 1988-1994.
Standardised admissions
Standardised admission ratios for males and females by ethnic group and age band are shown in Table 1. Admissions were higher for Black males, 473 (95% CI 435-513) than for White males, 85 (95% CI 81-89); and lower for Asian males: 39 (95% CI 30-49). Similarly, overall admissions were higher for Black females, 282 (95% CI 213-267) than for White females, 97 (95% CI 87-107), and lower for Asian females, 29 (95% CI 12-58). There were 5.6 times as many Black males admitted than White males, and nearly three times as many Black females than White females; 12 times as many Black males were admitted, and more than nine times as many Black females, than Asians of the same sex.
Table 1 Expected male and female admissions based on age-specific rates with standardised admission ratios (SARs)
| Age (years) | White | Black | Asian | Other | ||||
|---|---|---|---|---|---|---|---|---|
| No. expected | SAR (95% CI) | No. expected | SAR (95% CI) | No. expected | SAR (95% CI) | No. expected | SAR (95% CI) | |
| Males | ||||||||
| 15-24 | 559.7 | 85 (78-93) | 31.9 | 521 (445-607) | 61.2 | 26 (15-43) | 18.3 | 71 (78-122) |
| 25-34 | 921.2 | 80 (75-86) | 64.0 | 461 (410-517) | 77.3 | 41 (28-58) | 32.5 | 83 (55-121) |
| 35+ | 697.2 | 91 (84-98) | 25.2 | 441 (363-531) | 42.5 | 52 (32-78) | 12.1 | 107 (57-184) |
| Total | 2178.0 | 85 (81-89) | 121.0 | 473 (435-513) | 181.1 | 39 (30-49) | 62.9 | 84 (63-110) |
| Females | ||||||||
| 15-24 | 116.6 | 104 (86-124) | 7.0 | 215 (120-356) | 11.9 | 25 (5-75) | 3.5 | 50 (27-111) |
| 25-34 | 159.7 | 93 (79-110) | 10.2 | 284 (190-409) | 11.4 | 26 (5-78) | 4.7 | 105 (33-248) |
| 35+ | 112.6 | 94 (77-114) | 2.7 | 449 (231-787) | 4.3 | 47 (4-173) | 1.5 | 66 (0-378) |
| Total | 388.8 | 85 (87-107) | 19.8 | 282 (213-367) | 27.5 | 29 (12-58) | 9.8 | 61 (22-134) |
Logistic regression
Table 2 indicates that there were marked differences between Black and Asian patients admitted to secure services, and White patients, in terms of demography and several other characteristics that could have led to confounding within our subsequent analyses (numbers in ethnic groups are reduced because some data are missing). Compared to White patients, subjects in the Black ethnic group were more likely to be male, single, not born in the UK, living in the 20% of the most socio-economically deprived electoral wards of England and Wales according to the Jarman UPA, and less likely to have been admitted following non-criminal behaviour; and their primary psychopathology was less likely to be personality disorder. Compared to Whites, patients in the Asian subgroup were less likely to be unmarried prior to admission, more likely to be not born in the UK, more likely to originate from the 20% of most socio-economically deprived wards, and less likely to present with a primary diagnosis of personality disorder. As criminal statistics demonstrate a concentration of offences in inner-city areas in the UK, where non-White people are disproportionately concentrated, separate comparisons were carried out between Black and Asian ethnic subgroups and the White subgroup; first using crude OR, then by adjusting the OR having controlled for potential confounding factors of age, gender, single marital status, social deprivation according to UPA decile, and a primary diagnosis of personality disorder.
Table 2 Comparison of Black and Asian ethnic groups with White ethnic group for demography, socio-economic deprivation, non-crime admission and personality disorder diagnosis
| Variable | White (n=2224) | Black (n=628) | Asian (n=80) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | OR | (CI) | P | n | % | OR | (CI) | P | |
| Female | 367 | 17 | 56 | 9 | 0.48 | (0.36-0.65) | <0.001 | 10 | 13 | 0.70 | (0.36-1.38) | 0.300 |
| Single | 1567 | 71 | 507 | 81 | 1.80 | (1.45-2.25) | <0.001 | 31 | 39 | 0.26 | (0.17-0.42) | <0.001 |
| Non-UK-born | 125 | 6 | 217 | 35 | 0.11 | (0.09-0.14) | <0.001 | 61 | 76 | 0.02 | (0.01-0.03) | <0.001 |
| UPA Deciles 9+10 | 1207 | 54 | 554 | 88 | 6.31 | (4.88-8.15) | <0.001 | 67 | 84 | 4.34 | (2.28-7.91) | <0.001 |
| Non-crime admission | 467 | 21 | 102 | 16 | 0.73 | (0.58-0.92) | 0.008 | 13 | 16 | 0.74 | (0.41-1.36) | 0.330 |
| Personality disorder | 452 | 20 | 33 | 5 | 0.22 | (0.15-0.31) | <0.001 | 2 | 3 | 0.10 | (0.03-0.41) | <0.001 |
| Mean age (years) | 31.8 (s.d.=10.34) | 29.8 (s.d.=8.77) t=4.40, P<0.001 | 31.8 (s.d.=9.74) NS | |||||||||
Subjects were further stratified according to whether their admission followed criminal or non-criminalised behavioural disorder. For the subgroup of 569 (21%) patients whose admission had followed violent or difficult behaviour which had not led to criminal charges, comparisons were carried out between ethnic groups for behaviour specifically including violence to the person, fire-setting, sexual aggression, absconding from psychiatric facilities, deliberate self-harm, or other problem behaviour. No differences were found between the Black and Asian ethnic subgroups compared to the White ethnic subgroup for any of these variables.
Table 3 compares the index offences of Black and Asian ethnic subgroups (i.e. the offences which had led to admission) and those of the White subgroup, having stratified for admission due to criminal behaviour (80% of all patients) by excluding non-crime admissions. Black patients were more likely to be admitted following charges of, or convictions for, minor crimes of violence (assault occasioning actual bodily harm, threats to kill, possession of an offensive weapon), major sex offences (rape, buggery and indecent assault), robbery and drug-related offences. They were less likely to be admitted following arson and acquisitive offences (theft and burglary). There were no differences in types of criminal behaviour such as homicide, more serious violent offences (attempted murder, grievous bodily harm), and other offences not included in the table (including criminal damage, fraud and forgery, alcohol-related crimes and offences of public order). Asian patients were more likely than Whites to be admitted following homicide offences and less likely following acquisitive offences. (The index offences included in Table 3 are not mutually exclusive.)
Table 3 Odds ratios (95% CIs) for effects of index offence in Black and Asian ethnic groups
| Index offences | Black | Asian | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | P | Adjusted | P | Unadjusted | P | Adjusted | P | |
| Homicide | 0.99 (0.76-1.29) | 0.950 | 1.101 (0.18-1.44) | 0.490 | 2.05 (1.19-3.35) | 0.009 | 2.05 (1.17-3.60) | 0.012 |
| Attempted murder, grievous bodily harm | 1.29 (1.04-1.60) | 0.020 | 1.12 (0.89-1.43) | 0.330 | 1.35 (0.79-2.31) | 0.270 | 1.34 (0.78-2.29) | 0.280 |
| Actual bodily harm, threats | 1.41 (1.13-1.76) | 0.003 | 1.38 (1.10-1.73) | 0.005 | 0.59 (0.29-2.21) | 0.150 | 0.60 (0.29-1.21) | 0.150 |
| Rape, buggery | 2.10 (1.45-3.03) | <0.001 | 1.94 (1.34-2.81) | <0.001 | 2.04 (0.86-4.86) | 0.100 | 2.00 (0.83-4.80) | 0.120 |
| Indecent assault | 1.65 (1.12-2.41) | 0.010 | 1.53 (1.05-2.25) | 0.030 | 0.29 (0.04-2.13) | 0.200 | 0.28 (0.04-2.07) | 0.210 |
| Robbery | 1.57 (1.16-2.12) | 0.004 | 1.47 (1.08-2.00) | 0.010 | 0.50 (0.16-1.62) | 0.240 | 0.53 (0.16-1.71) | 0.280 |
| Arson | 0.33 (0.23-0.49) | <0.001 | 0.38 (0.25-0.56) | <0.001 | 0.65 (0.30-1.45) | 0.290 | 0.67 (0.29-1.51) | 0.330 |
| Theft/burglary | 0.70 (0.53-0.93) | 0.010 | 0.65 (0.49-0.87) | 0.003 | 0.22 (0.07-0.70) | 0.005 | 0.22 (0.07-0.72) | 0.012 |
| Drug-related | 1.74 (0.99-3.05) | 0.050 | 1.86 (1.05-3.27) | 0.030 | 1.45 (0.34-6.16) | 0.600 | 1.16 (0.27-4.98) | 0.860 |
Independent comparisons of the patterns of previous criminal behaviour and institutional history between Black and Asian ethnic groups and Whites are shown in Table 4. This demonstrates that Black patients were more likely to have previous convictions for violent, sexual, acquisitive, drug-related and robbery offences, and less likely to have previous convictions for arson and alcohol-related offences than Whites. Asian patients were less likely to have previous convictions for arson and acquisitive offences than Whites. There were no differences between Black and White ethnic groups in their previous experiences of having been in an approved school, borstal or young offenders' institution, or prison. Asian patients were less likely than Whites to have a previous history of approved school, borstal or young offenders' institution, or prison, and were also less likely to have a previous history of psychiatric hospitalisation than Whites. Black patients, although no more likely to have been in a psychiatric hospital on an informal basis, were more likely to have been compulsorily admitted on a civil order (Part II) and under Part III of the Mental Health Act following a previous criminal offence. Table 5 demonstrates the differences between the Black and Asian ethnic subgroups and the White subgroup according to their lifetime diagnostic categories. Black patients were more likely to receive diagnoses of schizophrenia, schizoaffective disorder, brief unspecified psychotic episodes, drug abuse or dependence, and less likely to receive diagnoses of depression, alcoholism, alcohol misuse, organic brain syndrome, and borderline personality disorder than White patients.
Table 4 Odds ratios (95% CI) for effects of previous criminal convictions, and institutional history, in Black and Asian ethnic subgroups
| Variable | Black | Asian | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | P | Adjusted | P | Unadjusted | P | Adjusted | P | |
| Previous convictions | ||||||||
| Violence | 1.81 (1.52-2.17) | <0.001 | 1.73 (1.44-2.08) | <0.001 | 0.73 (0.46-1.18) | 0.200 | 0.71 (0.44-1.14) | 0.160 |
| Sexual | 1.94 (1.42-2.66) | <0.001 | 1.74 (1.27-2.40) | 0.001 | 0.67 (0.21-2.16) | 0.500 | 0.63 (0.20-2.04) | 0.450 |
| Arson | 0.44 (0.29-0.08) | <0.001 | 0.49 (0.32-0.76) | 0.001 | 0.14 (0.02-0.99) | 0.020 | 0.14 (0.02-1.04) | 0.060 |
| Acquisitive | 1.54 (1.28-1.85) | <0.001 | 1.46 (1.21-1.75) | <0.001 | 0.33 (0.20-0.54) | <0.001 | 0.39 (0.19-0.52) | <0.001 |
| Alcohol-related | 0.29 (0.19-0.45) | <0.001 | 0.28 (0.18-0.43) | <0.001 | 0.60 (0.26-1.40) | 0.230 | 0.59 (0.25-1.36) | 0.210 |
| Drug-related | 2.96 (2.31-3.80) | <0.001 | 2.15 (2.15-3.56) | <0.001 | 0.46 (0.14-1.48) | 0.180 | 0.45 (0.14-1.44) | 0.180 |
| Robbery | 2.78 (2.16-3.57) | <0.001 | 2.19 (1.68-2.86) | <0.001 | 0.62 (0.23-1.72) | 0.360 | 0.50 (0.18-1.39) | 0.180 |
| Institutional history | ||||||||
| Approved school | 1.18 (0.89-1.41) | 0.350 | 1.01 (0.80-1.28) | 0.910 | 0.27 (0.10-1.74) | 0.006 | 0.25 (0.09-0.69) | 0.008 |
| Borstal/YOI | 1.30 (1.05-1.61) | 0.020 | 1.21 (0.98-1.51) | 0.080 | 0.34 (0.15-0.80) | 0.010 | 0.28 (0.12-0.65) | 0.003 |
| Prison | 1.37 (1.14-1.65) | 0.001 | 1.08 (0.89-1.31) | 0.420 | 0.38 (0.21-0.71) | 0.002 | 0.30 (0.16-0.56) | <0.001 |
| Psychiatric admission | 0.91 (0.75-1.11) | 0.370 | 0.96 (0.79-1.18) | 0.710 | 0.52 (0.33-0.82) | 0.004 | 0.52 (0.33-0.82) | 0.005 |
| Part II admission | 1.26 (1.06-1.51) | <0.010 | 1.32 (1.12-1.61) | 0.002 | 0.78 (0.49-1.25) | 0.310 | 0.80 (0.50-1.29) | 0.360 |
| Part III admission | 1.61 (1.34-1.94) | <0.001 | 1.78 (1.47-2.14) | <0.001 | 0.72 (0.42-1.21) | 0.210 | 0.71 (0.42-1.21) | 0.210 |
Table 5 Odds ratios (95% CIs) for effects of lifetime diagnosis in Black and Asian ethnic subgroups
| Variable | Black | Asian | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | P | Adjusted | P | Unadjusted | P | Adjusted | P | |
| Schizophrenia | 2.50 (2.05-3.04) | <0.001 | 1.83 (1.48-2.26) | <0.001 | 1.21 (0.77-1.90) | 0.410 | 0.76 (0.48-1.20) | 0.240 |
| Schizoaffective disorder | 2.01 (1.38-2.94) | <0.001 | 1.72 (1.18-2.54) | 0.005 | 3.01 (1.40-6.46) | 0.003 | 2.58 (1.20-5.56) | 0.020 |
| Unspecified psychosis | 1.79 (1.04-3.09) | 0.030 | 2.41 (1.34-4.34) | 0.003 | 1.41 (0.34-5.95) | 0.640 | 1.87 (0.12-2.30) | 0.400 |
| Depression | 0.28 (0.20-0.38) | <0.001 | 0.31 (0.22-0.42) | <0.001 | 0.94 (0.55-1.63) | 0.830 | 0.63 (0.36-1.11) | 0.100 |
| Alcoholism | 0.27 (0.22-0.34) | <0.001 | 0.29 (0.23-0.36) | <0.001 | 0.60 (0.37-0.97) | 0.040 | 0.65 (0.40-1.04) | 0.070 |
| Drug dependence/misuse | 2.07 (1.72-2.48) | <0.001 | 1.90 (1.57-2.31) | <0.001 | 0.49 (0.30-0.79) | 0.003 | 0.45 (0.27-0.75) | 0.002 |
| Organic brain syndrome | 0.47 (0.34-0.65) | <0.001 | 0.45 (0.32-0.63) | <0.001 | 0.81 (0.40-1.63) | 0.550 | 0.80 (0.39-1.61) | 0.530 |
| Antisocial personality disorder | 0.97 (0.79-1.19) | 0.080 | 1.03 (0.81-1.30) | 0.820 | 0.35 (0.17-0.73) | 0.003 | 0.44 (0.21-0.93) | 0.030 |
| Borderline personality disorder | 0.20 (0.11-0.35) | <0.001 | 0.23 (0.13-0.43) | <0.001 | 0.90 (0.89-0.92) | 0.004 | 0.001 | 0.340 |
Asian patients were more likely to receive a diagnosis of schizoaffective disorder and less likely to receive a diagnosis of drug dependence/misuse and antisocial personality disorder than patients in the White subgroup.
No differences were observed between several additional lifetime diagnoses which are not included in the table, such as delusional disorder, phobic disorder, obsessive-compulsive disorder, epilepsy, and dependent, paranoid and schizoid personality disorders (none of the diagnostic categories were mutually exclusive).
Comparisons were also made according to the source of referral and the location of the patient prior to admission. No differences were observed between ethnic groups according to whether they were admitted from prison, other psychiatric hospitals, the community, or a range of other locations. However, patients in the Black ethnic group were less likely to have been referred by a lawyer than Whites (adjusted odds ratio 0.69, 95% CI 0.52-0.91, P=0.008).
DISCUSSION
Methodological considerations
These analyses underestimate the prevalence of treated mentally disordered offenders and patients admitted to hospital following dangerous or difficult behaviour from the areas we studied. Most offender patients are admitted to ordinary psychiatric in-patient facilities, and the sample is representative of only the most serious offences against the person, sexual offences and arson, and cases for whom a forensic psychiatrist had determined that they required a bed in secure conditions. In some regions there were larger numbers of locked-ward (low security) beds available than in others. This factor may have reduced the pressure on the forensic psychiatry services to accept patients who presented with less serious offending and those who could otherwise have been managed at a lower level of security.
Changing demographics of forensic psychiatry
Department of Health statistics have indicated that there has been a progressive rise in admissions to psychiatric units in England and Wales over the past 15 years, accounted for by readmissions, compulsory admissions under Part II of the Mental Health Act, and compulsory admissions under Part III of the Act. Data from this study indicate that between 1988 and 1994, admissions of White patients to secure services rose and then fell, while the number of patients from non-White ethnic groups continued to rise. Admissions in all ethnic groups demonstrated a fall in 1993, relative to the previous 5 years. An unpublished study carried out in 1993 by one of us (J.C.) found a lack of any further bed capacity. The National Forensic Psychiatry Services, including the private sector, were over 100% full by 1993. Admissions could only rise following a further increase in the overall number of secure beds.
These time trends demonstrated moderate changes but require monitoring in the future. If the proportion of non-White admissions continues to increase, it would indicate that forensic psychiatry services in the UK must increasingly adapt to the needs of people with different cultural backgrounds. Bhui (Reference Bhui, Johnson, Ramsay and Thornicroft1997) has drawn attention to the concern within these communities that they do not receive services which they see as either acceptable or relevant to their needs. Catchment area populations with a significant proportion of persons of African-Caribbean origin may require an adjustment to the current formula for resource allocation in order to cope with this demand.
Risk factors for compulsory admission
It is of interest that the ratio of the number of Black to other males serving prison sentences in the United Kingdom was similar to that of Black to other males within the secure facilities we have studied. But whether risk factors leading to increased rates of imprisonment of Black males are the same as those leading to their increased rates of detention in secure psychiatric hospitals will require further study.
Black patients were more likely to be diagnosed as suffering from major psychosis and comorbid drug misuse and to be admitted following minor violent offences, serious sexual offending and robbery (findings similar to those for prisoners in England and Wales). Although they had more previous convictions, they did not appear more likely to have been in approved schools, borstals or prisons than the White ethnic group. They were more likely than Whites, however, to have been previously admitted compulsorily to hospital following a criminal conviction. These findings suggest that Black patients may demonstrate different patterns of criminal behaviour in association with mental illness, and that more were already known to psychiatric services as a result of previous criminal behaviour while mentally ill. This could reflect an accelerated pattern of offending behaviour related to the onset of severe mental illness. It is possible that the fact that a higher proportion of them were single, at the same time as living in more socio-economically deprived circumstances, contributed to a more significant degree of social isolation. Whether this contributed to poor compliance with medication and psychiatric follow-up after previous admissions, and to the risk of relapse and a further episode of psychotic illness exacerbated by misuse of drugs, are important questions that require further study. It also remains unclear whether community-based psychiatric services were able to intervene effectively in the cycle of relapse and subsequent reoffending that had previously occurred after discharges. However, for certain subjects the finding could reflect a predisposition to serious offending behaviour that was independent of their illness, but they had been diverted to hospital instead of prison because of mental illness.
Patients of Asian ethnic origin demonstrated very different patterns of criminal behaviour, and were considerably less likely to have had previous convictions for a range of different categories of offending. They were also less likely to have previously spent time in secure institutions. As they were highly unlikely to have a previous history of drug misuse, and few had previous convictions, the Asian subgroup demonstrated fewer risk factors that were potentially predictive of serious offending (Reference Copas and WalkerCopas, 1995).
Pathways into secure care
We did not specifically study our subjects' pathways into secure care. However, White patients were more likely to be referred from the community, or transferred from other psychiatric hospitals into secure forensic services, than Black (but not Asian) patients. This raises the question whether Black patients were more likely to be criminalised and processed instead through the criminal justice system, either having been rejected for treatment, or their illnesses having been missed by those assessing them at an earlier stage. However, there was no evidence that either Black or Asian patients were more likely to be transferred following non-criminalised violent or sexual behaviour in another hospital, which would have suggested that conventional psychiatric services had perceived them as more dangerous. There was some evidence that Black patients were less likely to have been referred to a forensic psychiatrist by lawyers. But whether this reflected reduced access to lawyers or more active endeavours by psychiatrists to find secure beds for White patients following instructions from defence lawyers (who attract a larger fee than the Crown Prosecution Service), would require future study.
The most striking diagnostic difference between the subgroups is the higher proportion of White patients considered to have a primary diagnosis of personality disorder. This has previously been observed in studies in special hospitals (Reference CoidCoid, 1992; Reference Shubsachs, Huws and CloseShubsachs et al, 1995) and raises two important questions for future research. First, do these findings reflect true differences between the prevalence of personality disorders in different ethnic groups? And second, do these findings result from clinical selection by forensic psychiatrists? For example, do they actively select Whites with personality disorders as more suitable for treatments such as psychotherapy in secure hospital settings?
Cultural and behavioural factors
Our analysis has allowed us to conclude that socio-economic disadvantage (determined by address or origin) was unlikely to be the primary cause of the variations we have observed between ethnic groups. Patients from African-Caribbean and Asian subgroups both originated from more socio-economically deprived areas, but treated prevalence rates were higher in African-Caribbeans and lower in Asians than in Whites. Similarly, patterns of criminal behaviour demonstrated even greater differences when the two non-White subgroups were compared.
The observation that many patients admitted to secure forensic services have experienced multiple previous compulsory admissions, including admissions following previous offending, suggests that psychiatric services sometimes fail to intervene effectively in a progressive escalation of seriousness of behavioural disorder associated with mental illness. Research should concentrate on recognition of high-risk subgroups of the mentally ill, within all ethnic groups, and the development of new measures to improve compliance with after-care. The finding of strikingly lower rates of admission in persons originating from the Indian subcontinent undermines the hypothesis that overrepresentation of certain ethnic subgroups merely reflects a racial bias operating within the criminal justice and psychiatric services. This should prompt the search for factors that were protective in this subgroup, and may ultimately indicate new preventive interventions.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Many patients in secure forensic psychiatry services demonstrate ‘high risk’ patterns of escalating criminal and dangerous behaviour, associated with repeated admissions to increasing levels of security.
-
▪ These patterns are more prevalent in African-Caribbeans, suggesting that community-based services may be less successful in their interventions with this group.
-
▪ New preventive interventions to improve after-care for high-risk patients, within all ethnic groups, are now priorities.
LIMITATIONS
-
▪ The survey involved a descriptive study of admissions, limited to specialist forensic psychiatry services.
-
▪ Classification into four categories does not take into account the range of cultural and ethnic backgrounds of the subjects.
-
▪ Diagnostic categories were based on patients' records.
ACKNOWLEDGEMENTS
This study was funded by a grant from the Department of Health. It would not have been possible without the cooperation of clinical and administrative staff in the medium secure units of the North West Thames, North East Thames, West Midland, Merseyside, North Western, South Western and East Anglian Regions, of Kneesworth House, Stockton Hall and St Andrew's Hospital, Northampton, and of Broadmoor, Rampton and Ashworth Special Hospitals; their assistance and advice are gratefully acknowledged.









eLetters
No eLetters have been published for this article.