Globally, CVD are the main cause of morbidity and mortality. They present multiple factors and several common mechanisms, and are highly influenced by inflammatory activity. Among the common and modifiable risk factors associated with CVD are diabetes mellitus (DM), hypertension, dyslipdaemia, hypertriacylglycerolaemia and obesity. Addressing the risk factors decreases the incidence and development of these diseases(1, Reference Esmaillzadeh and Azadbakht2).
It is known that Japanese people who live in Japan present lower CVD morbidity and mortality rates than Japanese immigrants and their descendents who live in the Americas(Reference Fujimoto, Bergstrom and Boyko3). Brazil is home to the largest Japanese population outside Japan (around 1 280 000 people) and more than 70 % of this total lives in the south-east region, mainly in the State of São Paulo(4). The size of this community, along with the results of American studies about the prevalence of type 2 DM among Japanese descendents in the USA(Reference Fujimoto, Bergstrom and Boyko5), led to the creation of the Japanese-Brazilian Diabetes Study Group (JBDSG). The results of studies of this group of researchers, carried out according to WHO guidelines(Reference Alberti and Zimmet6), have shown that the prevalence of type 2 DM was 25·5 % for men and 19·9 % for women in 1993, increasing to 40·6 % and 32·4 %, respectively, in 2000(Reference Gimeno, Ferreira and Franco7). Significant increases in BMI and in all other risk factors of the metabolic syndrome have also been noticed(Reference Rosenbaum, Gimeno and Sanudo8). These findings indicate the existence of a strong genetic predisposition associated with unfavourable environmental conditions related to the occidental lifestyle, and the need to implement measures to prevent and control the problem among these immigrants.
Epidemiological studies reporting the efficiency of lifestyle changes in decreasing the incidence of type 2 DM can be found in the literature(Reference Pan, Li and Hu9, Reference Tuomilehto, Lindstrom and Eriksson10). The results of surveys conducted with individuals presenting impaired glucose tolerance and excess weight have shown that changes in lifestyle are more effective than drug-based interventions(Reference Knowler, Barrett-Conner and Fowler11). However, as pointed by Sarrafzadegan et al.(Reference Sarrafzadegan, Kelishadi and Esmaillzadeh12), these evidences are less clear for developing countries and intervention studies in such countries have been scarce.
In this context, the main objective of the present study was to describe the results of a nutritional intervention programme carried out with Japanese-Brazilians according to gender.
Experimental methods
This was a non-controlled experimental study that was developed according to principles embodied in the Declaration of Helsinki. It was approved by the Research Ethics Committee of São Paulo Federal University – UNIFESP (protocol number 0862/05).
Considering the unfavourable cardiovascular profile found among Japanese-Brazilians as previously described by JBDSG researchers(Reference Gimeno, Ferreira and Franco7, Reference Rosenbaum, Gimeno and Sanudo8), characterized by a high percentage of glucose intolerance (70 %), hypertension (58 %), dyslipidaemia (65 %) and central obesity (57 %), all participants of the JBDSG study conducted in 2000 (n 1330) were invited to participate in the current nutritional intervention programme regardless of their chronic diseases or nutritional status. They represented the total Japanese-Brazilian first (Japan born) and second (born in Brazil) generation living in Bauru (State of São Paulo, south-east region of Brazil) of both genders and ≥30 years of age. In total 736 Japanese-Brazilians joined the intervention programme. Reasons for non-attendance (44·7 %) were death (15·7 %), moving to other city or country and refusal (84·3 %). Unimportant differences were observed concerning gender, age, generation and glucose tolerance status between non-participants and participants of the intervention study. The data of 575 subjects (78·1 %) who had been evaluated at least twice, at baseline (2005) and final (2006 or 2007), were used in the present analysis (Fig. 1).
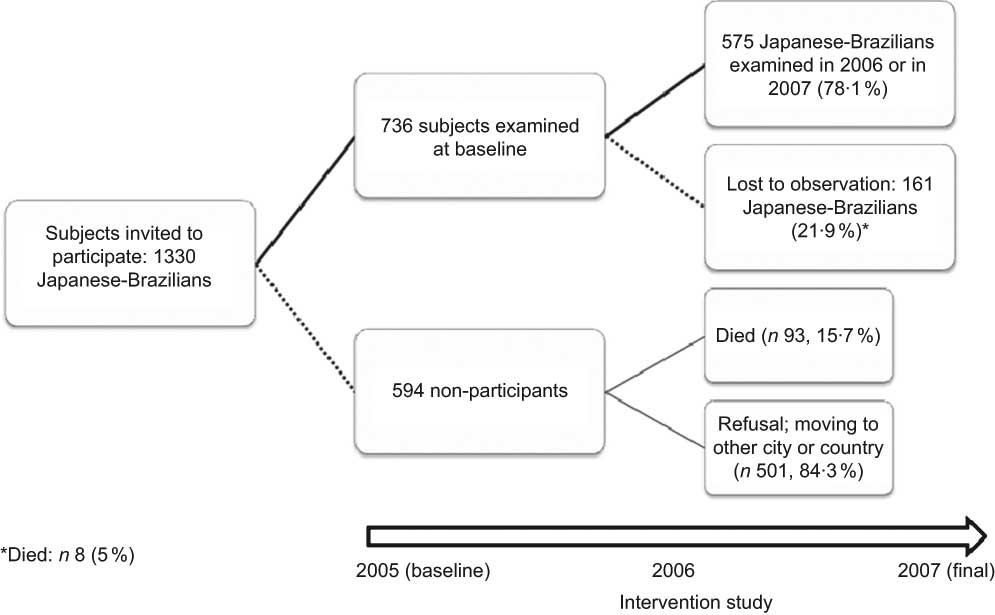
Fig. 1 Participants in the nutritional intervention study, Baura, São Paulo, Brazil, 2007
The nutritional intervention programme was communicated through letters and community events. All subjects were informed about the research objectives, of the minimum risks associated with blood collection with disposable materials and of the advantages of participating in the nutritional programme; information reliability and confidentiality were secured. Those who agreed to participate signed an informed consent agreement.
The survey included three clinical examinations: at baseline (2005), after the first intervention year (2006) and at the end of the second year (2007). On these occasions, subjects were physically examined, fasting blood samples were collected for several biochemical analyses and three 24 h dietary recalls were completed.
Nutritional intervention strategy
The nutritional intervention was based on a programme previously conducted at a health-care service of the State of São Paulo(Reference Sartorelli, Sciarra and Franco13, Reference Sartorelli, Sciarra and Franco14). Improvements in the anthropometric (primary outcome), clinical and biochemical profiles of the Japanese-Brazilian subjects were the goals of the intervention programme. Individual energy requirements and nutritional status of each subject were taken into consideration for diet prescription. For those presenting overweight or central obesity, a diet with reduced energy (2092 to 4184 kJ/d) was prescribed, aiming at a 5 % weight loss. Diet consisted of five meals per day with the following distribution of total energy: 50–60 % from carbohydrates (mainly complex carbohydrates); less than 10 % from SFA (red meat intake reduced to two medium servings daily, two or three daily servings of low-fat dairy products, and reduced intake of fried food, fat, mayonnaise, industrialized food dressing, fatty meat, poultry skin and too many eggs); minimum of 20 % from MUFA and PUFA (olive oil, nuts and fish); and 400 g of fruits and vegetables daily (equivalent to five servings).
The intervention plan was divided into two phases: (i) an individual nutritional assessment and (ii) two group orientation meetings (at the first and second year of the intervention programme) coordinated by nutritionists. In the first phase subjects received an individual assessment: their food records were checked, a detailed nutritional evaluation was made (food intake, energy needs, nutritional status, clinical and biochemical examinations), a diet was prescribed with a list of food replacements, and orientation was given on the importance of a healthy diet and physical activity. The two group meetings focused on food intake goals, physical activity, healthy lifestyle and discussion about difficulties faced by the subjects. Physical therapists and nutritionists supported these sessions.
Evaluation measures
In the three clinical examinations, all subjects were invited to come fasting (10 h minimum) to the clinical laboratory of Sagrado Coração University (Bauru), where a physical examination and a biochemical evaluation were done by the medical staff of UNIFESP. The physical examination included anthropometric measurements and evaluation of blood pressure and physical activity. For those who were not fluent in the Portuguese language, family members or bilingual staff members helped perform the examinations.
After collection of baseline data, results were informed to the participants and those who had health problems were sent for medical care; at that time, appointments with nutritionists were scheduled (subjects and their family members) for orientation on healthy lifestyle.
At the three clinical examinations (baseline in 2005; intermediate in 2006; final in 2007) three 24 h recalls were obtained by nutritionists during the group meetings, laboratory examinations or clinical examinations. Detailed information on food and beverages consumed in the last 24 h was requested. All questionnaires were revised in order to check data quality. Data of food intake in household measures were transformed into grams. To avoid discrepancies when typing data, all recipes and preparations were standardized according to a previously elaborated codification manual. NutWin software (Programa de Apoio à Nutrição, Versão 1.5; Escola Paulista de Medicina, São Paulo, Brazil) was used to quantity nutrient intake. National and international food composition tables were used for those foods not included in the above software(15–17). In all clinical examinations, the average values of the nutrients gathered in the three 24 h dietary recalls were analysed to evaluate possible changes in dietary habits.
During the clinical assessment, weight (kg) and height (m) were measured using a digital scale (150 kg capacity, 100 g precision) and a portable stadiometer, respectively. Waist circumference (cm) was measured with a measuring tape at navel level, with subjects standing upright, with relaxed abdomen, arms along the body and feet together. Blood pressure measurements were taken three times with an automatic monitor (model HEM-712C; Omron Healthcare, Inc., Bannockburn, IL, USA) approved by the American Heart Association for epidemiological studies. After a rest for 5 min, the cuff was applied to the right upper arm of the subject who was seated, and automatically inflated. Deflation occurred at a speed pre-determined by the equipment. Final values of systolic and diastolic blood pressure were the arithmetic average of the last two measurements (mmHg). Also, the physical activity of the Japanese-Brazilians was evaluated using the short version of the International Physical Activity Questionnaire (IPAQ), which has been validated in twelve countries including Brazil(Reference Matsudo, Timoteo and Matsudo18, Reference Craig, Marshall and Sjostrom19). A fasting blood sample was collected to determine glucose level and lipid profile (total cholesterol and its fractions, TAG), among others. The glucose oxidation method was used to determine glycaemia and enzymatic kits were used to measure lipoproteins.
Statistical analyses
Data from the laboratory and anthropometric examinations were analysed with the STATA statistical software package version 10·0 (Stata Corp., College Station, TX, USA). Relative and absolute frequencies, measures of central tendency and dispersion of clinical, biochemical, dietary and anthropometric variables, collected at different time points, were calculated. In crude analyses the paired Student t test was used to verify the presence of statistically significant alterations in nutritional, clinical and biochemical indices at the end of the intervention programme. Absolute changes in all variables of interest (final minus baseline value) observed during the intervention programme were compared between men and women who achieved the study goal (improvement in anthropometric profile) or not, using the Student t test. Multiple linear regression analysis was employed to adjust the absolute change in all variables according to their baseline values and number of examinations (two or three). For analysis purposes, all nutrients were adjusted by energy according to Willett and Stampfer(Reference Willett and Stampfer20).
Results
The 161 (21·9 %) Japanese-Brazilians excluded from the present analysis (those who had been examined just once) presented similar frequency distributions to those who were evaluated two or three times for gender, age, BMI and waist circumference (P > 0·05).
Of the 575 subjects who participated in the nutritional intervention programme, 197 were evaluated twice (baseline and final: at 12 or 24 months), while 378 were examined three times (baseline, intermediate and final). Analysis of frequency distributions according to sociodemographic characteristics, anthropometric measures, health status and examinations performed showed a statistically higher rate of individuals with central obesity or normal glucose tolerance among those with two evaluations, compared with those who were evaluated three times.
Female and second-generation subjects represented 56·9 % and 84·7 % of the participants in the intervention programme, respectively. Table 1 shows mean values of anthropometric, clinical, biochemical, dietary and physical activity variables for Japanese-Brazilian men. Comparison of baseline and final values (crude and adjusted changes) showed significant reductions of body weight, waist circumference, blood pressure, fasting glucose, TAG, total cholesterol and its fractions, and energy, SFA and fibre intakes. During this period a statistically significant increase of carbohydrate intake was also observed.
Table 1 Baseline and final mean values with standard deviations, and absolute change and adjusted change with 95% confidence intervals, of anthropometric, clinical, biochemical, dietary and physical activity variables of Japanese-Brazilian men during the intervention programme, Bauru, São Paulo, Brazil, 2007

WC, waist circumference; DBP, diastolic blood pressure; SBP, systolic blood pressure; TC, total cholesterol; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol.
*Paired Student t test.
†Absolute change=(final minus baseline value).
‡Adjusted to baseline value and number of examinations.
§Log-transformed value for statistical test.
∥Energy-adjusted value by the residual method for statistical test and confidence interval estimation.
The comparison of values of baseline and final variables among women showed statistically significant decreases in weight, waist circumference, blood pressure, fasting glucose, total cholesterol and its fractions, and protein, total fat (including PUFA, MUFA and SFA) and fibre intakes (Table 2). The mean daily intake of carbohydrate and alcohol increased during the study period.
Table 2 Baseline and final mean values with standard deviations, and absolute change and adjusted change with 95% confidence intervals, of anthropometric, clinical, biochemical, dietary and physical activity variables of Japanese-Brazilian women during the intervention programme, Bauru, São Paulo, Brazil, 2007

WC, waist circumference; DBP, diastolic blood pressure; SBP, systolic blood pressure; TC, total cholesterol; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol.
*Paired Student t test.
†Absolute change = (final minus baseline value).
‡Adjusted to baseline value and number of examinations.
§Log-transformed value for statistical test.
∥Energy-adjusted value by the residual method for statistical test and confidence interval estimation.
Both genders showed a significant mean weight loss (0·9 kg) and a reduction in waist circumference (2·9 cm). Among all subjects, 32·5 % (n 172) achieved the primary goal of the study. Table 3 shows the main features of these Japanese-Brazilians according to gender. Statistically significant improvements in nutritional and metabolic profile were observed among those who achieved the study goals, especially in men (weight, BMI and TAG levels). Even among those who did not achieve the study goal, some benefits to cardiovascular health were apparently reported, particularly in men.
Table 3 Mean absolute change with standard deviationsFootnote *,Footnote † for anthropometric, clinical, biochemical, dietary and physical activity variables of Japanese-Brazilians during the intervention programme according to gender and achievement of the study goal, Bauru, São Paulo, Brazil, 2007

WC, waist circumference; DBP, diastolic blood pressure; SBP, systolic blood pressure; TC, total cholesterol; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol.
* Absolute change = (final minus baseline value).
† Adjusted to baseline value and number of examinations.
‡ Student’s t test.
§ Log-transformed value for statistical test.
∥ Energy-adjusted value by the residual method for statistical test.
Discussion
The present intervention was based on a programme previously applied among overweight Brazilian subjects at a primary health-care centre that was effective in a short follow-up time(Reference Sartorelli, Sciarra and Franco13, Reference Sartorelli, Sciarra and Franco14). In the present study, we verified that this programme is also suitable for free-living Japanese-Brazilian subjects after 24 months of follow-up. Nutritional intervention studies among Japanese migrants are sparse in the literature.
In both genders, a substantial improvement in nutritional and metabolic profile was detected during the study. Comparison of the results of both genders suggests that men have achieved better results, with important changes in their anthropometric and metabolic profiles (except HDL cholesterol levels), even with no significant changes in physical activity and food intake. It is important to note that a decrease in energy intake due to reduced SFA intake can contribute to decrease LDL cholesterol levels, as observed in the present study. Although diet compliance has not been evaluated, the results presented suggest (indirectly) that it was, at least, moderate.
Several studies have shown the efficacy of lifestyle intervention programmes in reducing the incidence of type 2 DM, reporting body weight reduction, better glucose tolerance, decreased blood pressure and improved plasma lipid profile of the subjects. In their study with 1232 normotense and hypercholesterolaemic subjects aged between 40 and 49 years, Forti and Diament observed that after a 5-year oriented diet the intervention group presented a 45 % reduction of myocardial infarction risk because of decreased hypercholesterolaemia (13 %) and TAG levels (20 %) and increased HDL cholesterol levels (20 %)(Reference Forti and Diament21). Researchers of the Multiple Risk Factor Intervention Trial (MRFIT) followed up 12 866 high-risk subjects from twenty-two US clinical centres. The subjects were divided into two groups: (i) the intervention group (participants received group and individual counselling on smoking cessation, drug treatment programme and hypocholesterolaemic diet) and (ii) the usual care group (subjects were informed about risk factor reduction and drug treatment programme). After 6 years of follow-up, subjects from the intervention group presented a decline in hypercholesterolaemia (5 %) and smoking habit (50 %). Over a longer period of time (10·5 years) subjects in the intervention group showed a 36 % reduction of CHD mortality risk compared with those in the usual care group(Reference Eberly, Neaton and Thomas22).
In weight-loss studies a lack of accuracy in self-reporting of food consumption and physical activities is frequently reported(Reference Siedel, Powell and Zgibor23). In this regard, in our study dietary intake was assessed every meeting using standardized procedures by highly trained nutritionists; however, the limitations of the 24 h dietary recall, such as under-reporting mainly by women and by those with higher body weight, are well described(Reference Tucker24).
In our study 21·9 % of the subjects evaluated at baseline were lost to observation; this is a problem frequently found in epidemiological studies with moderate- to long-term follow-up(Reference Bo, Ciccone and Baldi25–Reference Pagoto, Kantor and Bodenlos28). Considering that the subjects lost presented similar frequency distribution to those who were evaluated two or three times according to some characteristics of interest (gender, age, BMI, waist circumference), we can conclude that the study population was representative of all Japanese-Brazilians who agreed to participate in this nutritional intervention programme.
The absence of a control group did not allow us to show that the results of the study were actually due to the intervention programme. Randomized controlled intervention studies are more efficient to evaluate causal relationships. However, there are ethical or logistical situations in which this type of study is not advisable. One of the most frequent, which applies to the current study, is the ethical consideration. When the effectiveness of an intervention is well known and established, proven by previous studies, then the ethical question arises and does not allow the denial of treatment to a group of individuals(Reference Harris, McGregor and Perencevich29). As previously described(Reference Gimeno, Ferreira and Franco7, Reference Rosenbaum, Gimeno and Sanudo8), this Japanese-Brazilian community demonstrated a high prevalence of metabolic syndrome components and initiatives to minimize this problem were needed urgently. In this context, the JBDSG researchers conducted the present nutritional intervention study. It is important to note that the results found in the present study are in agreement with those previously published(Reference Pan, Li and Hu9–Reference Sartorelli, Sciarra and Franco14, Reference Forti and Diament21–Reference Siedel, Powell and Zgibor23). Also, the absolute change adjustment to baseline values and number of examinations may have contributed to reduce the possibility of bias in the present results.
Some limitations of the study must be taken into consideration. First, although it is known that the motivation to change dietary and health habits of the subjects who entered the intervention study may be different from that of non-participants (people who were invited but, for different reasons, did not want or could not join the programme), this fact does not jeopardize the results. Second, the supposition that all intervention programme subjects adhered to the treatment has not been evaluated; but it is presumed that if 100 % of the subjects had adhered, the positive results would have been higher. Third, it is known that measurement mistakes in food intake and physical activity cannot be eliminated entirely, but the choice of a standardized methodology to collect information has probably minimized the risks. Fourth, the combined analysis of the data of subjects who were evaluated two or three times may have reduced the observed effects, as intervention benefits may be higher in shorter periods of time. Finally, the results refer to a 2-year follow-up of Japanese-Brazilian subjects but the long-term impact is unknown.
It can be concluded that the intervention programme was of benefit to those Japanese-Brazilian subjects who incorporated healthier lifestyle habits, as reflected in their nutritional and metabolic profile. Other studies are necessary to evaluate the effects of the benefits over longer periods of time.
Acknowledgements
Sources of funding: Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP, 2005/59178-7) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, 505845/2004-0). Conflict of interest: None declared. Contribution of each author: R.D. participated in planning and execution of the nutritional intervention study, in data collection and in manuscript writing. D.S.S., A.H., F.M., J.P., M.R.B., R.C. and V.L.M.A.d.S. participated in planning and execution of the nutritional intervention study, in data collection and in manuscript review. L.A. participated in the planning and writing of the manuscript. S.R.G.F. participated in planning and execution of the nutritional intervention study, in data collection, in manuscript review and in funding obtaining to support the research (CNPq, 505845/2004-0). S.A. participated in the planning, statistical analysis and writing of the manuscript. S.G.A.G. participated in planning and execution of the nutritional intervention study, in data collection, in manuscript writing and in obtaining funding to support the research (FAPESP, 2005/59178-7). Acknowledgements: The authors thank the Japanese-Brazilian community living in Bauru for their kind cooperation.
Appendix Members of Japanese-Brazilian Diabetes Study Group
A. Hirai, A.T. Hirai, H. Harima, M. Kikuchi, K. Osiro, S.G.A. Gimeno (Department of Preventive Medicine, Federal University of São Paulo, Brazil); R. Damião (Nutrition Graduation Course of Triângulo Mineiro Federal University, Brazil); L.J. Franco, D. Sartorelli (Department of Social Medicine, Faculty of Medicine of Ribeirão Preto, University of São Paulo, Brazil); L. Matsumura (Department of Internal Medicine, Federal University of São Paulo, Brazil); K. Wakisaka (Japanese-Brazilians Study Center, Brazil); R. Chaim (Department of Nutrition, University of Sagrado Coração de Jesus, Bauru, Brazil); M.A. Cardoso, S.R.G. Ferreira (Department of Nutrition, School of Public Health, University of São Paulo, Brazil).






