Introduction
The medical system is an extensive network of teams that work together to deliver care. This system is complex; interprofessional team members hold unique qualifications and education, and the membership of teams frequently fluctuates. Such complexity can cause issues with teamwork; collaboration can be hindered by the use of unfamiliar jargon, as well as differing knowledge, procedures, and work norms [Reference Rosen, DiazGranados and Dietz1]. While selecting providers based on their individual competence (e.g., education, test scores) is common, team science researchers caution that a team of experts does not necessarily make an expert team [Reference Salas, Reyes and McDaniel2]. Though technical skills and knowledge are important, healthcare providers that work as part of a team must also have nontechnical skills (e.g., communication, coordination) to develop and execute patient care plans effectively. Without the ability to work together, even a team consisting of leading experts in their field can fail [Reference Salas, Reyes and McDaniel2]. Research has shown that teamwork impacts patient (e.g., morbidity, mortality), staff (e.g., well-being), and healthcare organizational outcomes [Reference Rosen, DiazGranados and Dietz1]. Clinician perceptions and attitudes towards teamwork are related to staff well-being, which can impact clinicians’ ability to provide safe care [Reference Manser3].
In addition to considering teamwork skills in provider/trainee selection, teamwork training is recommended to improve performance. Healthcare team training is effective and has a significant impact on attitudes, learning, transfer, and results [Reference Hughes, Gregory and Joseph4,Reference Weaver, Dy and Rosen5]. Both classroom and simulation-based team training interventions improve teamwork processes and patient safety outcomes [Reference Weaver, Dy and Rosen5]. These interventions are even more effective when accompanied by tools and organizational change that support the sustained transfer of teamwork competencies to practice [Reference Weaver, Dy and Rosen5]. The dynamic nature of healthcare teams underscores the need for as many team members as possible to possess sound teamwork competencies.
Although there is evidence that team knowledge, skills, and attitudes are important and training is beneficial, consensus on the optimal training content, methods, and evaluation is lacking [Reference Rosen, DiazGranados and Dietz1,Reference Hughes, Gregory and Joseph4,Reference Buljac-Samardzic, Doekhie and van Wijngaarden6]. The TeamSTEPPS™ training program provides a strong foundation for team training efforts. In the area of training content, the proposed framework adds instructional value to this foundation by integrating newer teamwork concepts, which have been identified in recent literature (e.g., creating a psychologically safe environment, team orientation) [Reference King, Battles, Baker, Henriksen, Battles and Keyes7,Reference Newman, Donohue and Eva8,Reference Rahman, Rehman, Imran and Aslam9]. Existing evidence indicates that there is a need to: 1) develop teamwork interventions that are rooted in the science of teamwork, 2) implement educational interventions meaningfully, such that evidence-based best practices for training implementation are followed to the greatest extent possible given practical restrictions (i.e., resources available), and 3) rigorously evaluate education initiatives to establish training efficacy, identify areas for improvement in implementation efforts, and guide continual training refinement. This paper will primarily address the first need, establishing the content for an interprofessional, preclinical teamwork training program. This program is derived from team science, building beyond the TeamSTEPPS™ program with complimentary elements. Considerations for training implementation and rigorous evaluation will also be briefly overviewed. While an in-depth discussion of implementation strategies and best practices (e.g., implementation methods, evaluation) is crucial, it is beyond the scope of the current paper and will be the focus of future work.
Teamwork Competencies
To optimize team performance in a complicated multidisciplinary healthcare environment, team training must address learners of all levels, teams working in various settings, and teams of teams, from cognitive- to procedural-based teams. We worked with team scientists to identify critical teamwork competencies for healthcare professionals and design a curriculum around these competencies. These experts drew from their experiences studying teams not only in healthcare, but also in aviation, aeronautics, engineering, and the military. This complimented the contextual knowledge of clinical educators to establish the most important competencies for healthcare-specific team challenges. Through this combined effort, the Team FIRST (Feedback, Interprofessional, Reliable, Safe for Synthesis, and Team Training) framework was developed. This framework asserts that there are 10 requisite teamwork competencies that are essential for healthcare providers. Research suggests that to create an effective team training program, critical teamwork competencies must be used as a foundation for focusing training content [Reference Salas, DiazGranados, Weaver and King10]. These competencies are clustered under three overarching themes: handling teamwork challenges, communication skills, and coordination skills. Each of the 10 competencies and their rationale for selection are discussed below, as well as the risks to their effective execution and practical implications for healthcare education. The competencies are defined in Fig. 1.
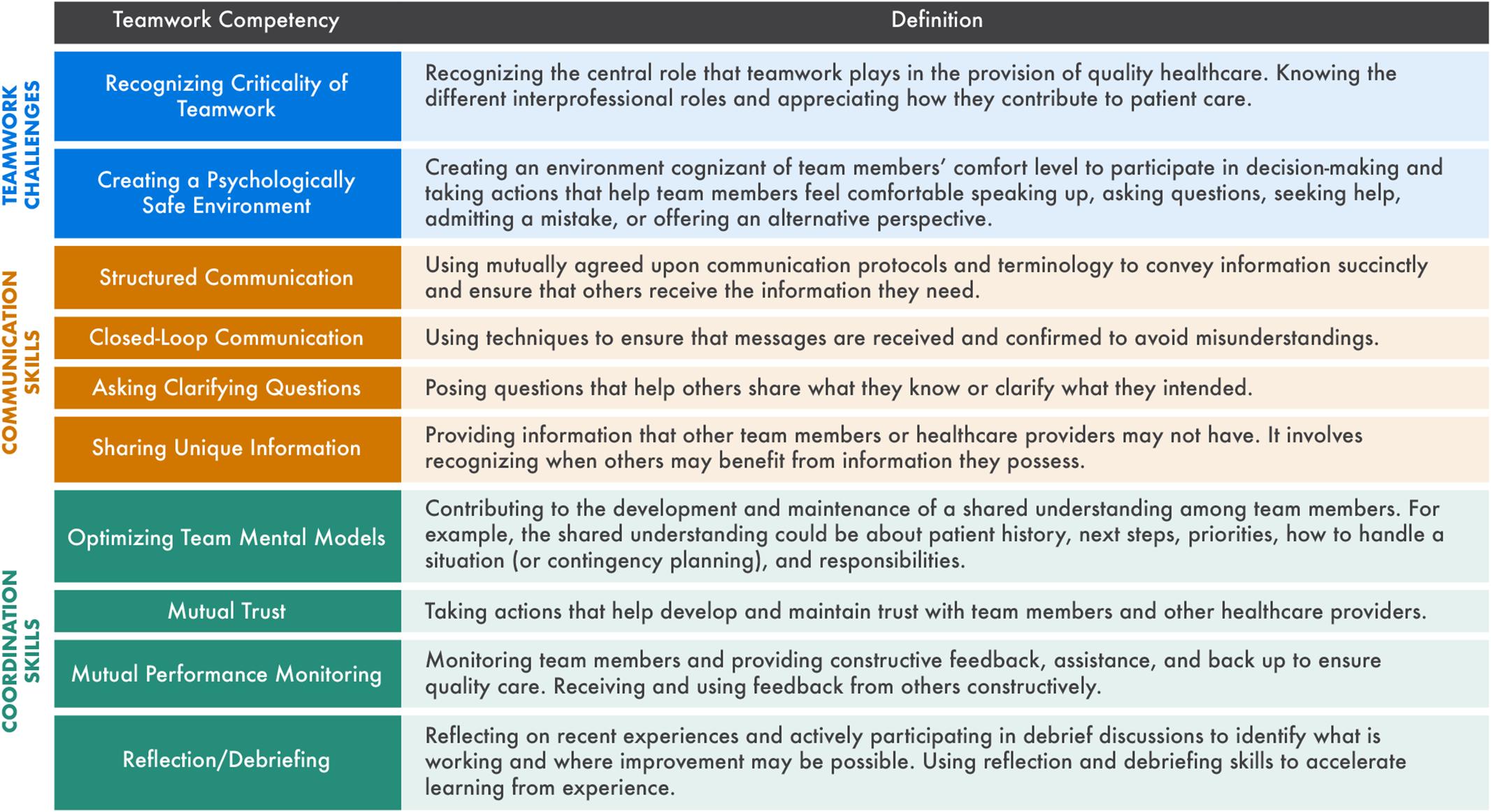
Fig. 1. Defining the 10 Team FIRST teamwork competencies.
Fig. 2 depicts our conceptual model of all 10 Team FIRST competencies, their interaction, and the process by which they impact performance. The framework begins with the competencies that teams must have to effectively work together and handle challenges to teamwork.

Fig. 2. The Team FIRST framework.
When individuals recognize the criticality of teamwork and the team is psychologically safe, an environment exists in which teams can engage in functional competencies including mutual performance monitoring, reflection/debriefing, and effective communication (i.e., structured communication, closed-loop communication, asking clarifying questions, and sharing unique information). Mutual performance monitoring, reflection/debriefing, and communication skills help develop effective team mental models (TMMs) and mutual trust, which ultimately impact team performance (e.g., patient safety, efficiency, provider wellness) [Reference Rosen, DiazGranados and Dietz1]. We believe that providing learners with an understanding of how these competencies enable or enhance each other is key to developing a deeper comprehension of the inherent challenges of teamwork, while also providing guidance on how to approach addressing them. For example, teams are unlikely to learn and apply new communication skills if they do not have an appreciation for the criticality of teamwork or a psychologically safe environment in which to practice these skills.
Handling Teamwork Challenges
Handling teamwork challenges enables the effective development of teamwork competencies and involves anticipating, recognizing, and overcoming common challenges to teamwork. This requires team members to acknowledge the criticality of teamwork, instill a psychologically safe climate, and proactively identify potential obstacles to teamwork. This may include actions such as actively managing distractions (e.g., noise), acknowledging the competing responsibilities of team members (caused by environmental factors like scheduling conflicts), inviting readback/feedback, addressing anticipated obstacles while forming treatment plans, and utilizing huddles and debriefs to discuss concerns.
Recognizing criticality of teamwork. For healthcare providers to engage in effective teamwork, each team member must recognize its importance and place team goals ahead of their own (e.g., Team FIRST), otherwise known as team orientation [Reference Rahman, Rehman, Imran and Aslam9]. Teams need to understand how different interprofessional roles contribute to patient care and affect one’s ability to complete their own tasks. Without recognizing the criticality of teamwork, team members may not engage in effective back-up behaviors or care coordination, such as recognizing and addressing a medication error before it causes patient harm. Past research indicates that higher levels of team orientation are associated with higher performance [Reference Rahman, Rehman, Imran and Aslam9]. Team orientation has traditionally been viewed as a relatively stable, intrinsic construct [Reference Eby and Dobbins11]. However, there is evidence to suggest that team orientation is related to cooperative team behaviors and can change over time through experience [Reference Eby and Dobbins11]. By providing healthcare professionals with team training, education on the importance of teamwork, and positive team experiences, it is possible to increase team orientation [Reference Rahman, Rehman, Imran and Aslam9,Reference Eby and Dobbins11,Reference Chakraborti, Boonyasai, Wright and Kern12]. Providers should learn to recognize that their effectiveness as a clinician is dependent on more than their clinical knowledge and skills; teamwork skills are critical to high performance and must also be developed [Reference Rosen, DiazGranados and Dietz1].
Creating a psychologically safe environment. Psychological safety is the collective perception shared among team members that the team is safe for interpersonal risk-taking [Reference Edmondson13], including actions such as speaking up, asking questions, admitting mistakes, seeking help, and offering alternative perspectives during group discussions. Creating a psychologically safe environment is critical to ensure healthcare team members feel empowered to voice concerns to prevent patient safety incidents. Supporting this, psychological safety is present in several recent healthcare teamwork frameworks [Reference Salas, DiazGranados, Weaver and King10,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14]. Research indicates that teams with higher psychological safety tend to outperform other teams [Reference Newman, Donohue and Eva8]. Maintaining the balance between psychological safety and accountability can be difficult in environments with a hierarchical structure, as is present in healthcare. Providers may feel reluctant to speak up or admit concern in the presence of people with authority or greater expertise [Reference Newman, Donohue and Eva8]. Perceived status within a team has been shown to affect psychological safety [Reference Newman, Donohue and Eva8]. If leaders are unnecessarily harsh, team members can become embarrassed, adversely impacting psychological safety throughout the team [Reference Edmondson13]. Research suggests that psychological safety is most effectively propagated through the example of team leaders; team members will reciprocate the support they receive. Therefore, it is critical for team leaders to create a psychologically safe environment by consistently encouraging team members to voice concerns and ensuring members do not suffer repercussions for speaking up. This will in turn lead team members to emulate this example towards their leaders and coworkers [Reference Newman, Donohue and Eva8].
Communication Skills
Communication can be defined as an exchange of information between two or more team members [Reference Marlow, Lacerenza, Paoletti, Burke and Salas15]. Communication is a fundamental competency present in numerous existing healthcare teamwork frameworks and training initiatives [Reference Rosen, DiazGranados and Dietz1,Reference Manser3,Reference Salas, DiazGranados, Weaver and King10,Reference Chakraborti, Boonyasai, Wright and Kern12,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14,Reference Clay-Williams and Braithwaite16]. Communication is considered a transportable teamwork competency; it is important regardless of the context in which the team works [Reference Salas, Reyes and McDaniel2]. Ineffective communication has been identified as a causal factor in medical errors and patient harm [Reference Morath and Turnbull17]. Therefore, it is critical to advance providers’ understanding of communication competencies and provide them with opportunities to practice and receive feedback in the context of ubiquitous communication events, such as handovers. Four subcomponents of communication that healthcare organizations should focus on developing include: structured communication, closed-loop communication, asking clarifying questions, and sharing unique information. Mastering these communication skills is also critical to developing coordination competencies like optimizing TMMs and mutual trust.
Structured communication. To communicate efficiently and effectively, it is critical that teams establish structured communication patterns. When the communicator and the recipient in a communication event share a common understanding of mutually established communication protocols and use consistent terminology, communication content and clarity improve [Reference Marshall, Harrison and Flanagan18], and cognitive load (the work required to process information) decreases [Reference Young, Ten Cate, O’Sullivan and Irby19]. Structured communication is prevalent during patient handoffs, where communication protocols are commonly used. However, it is also useful in other interactions, such as care planning and problem-solving sessions. Results from the implementation of a commonly used structured communication strategy, SBAR (Situation, Background, Assessment, and Recommendations), have shown improved communication competence in interprofessional collaboration [Reference Randmaa, Mårtensson, Swenne and Engström20]. Organizations should be mindful that utilizing several different communication protocols (e.g., different mnemonics) may increase the risk of misunderstandings. Healthcare professionals should keep in mind that when speaking with individuals outside of their team (e.g., patient, physician in a different discipline), that they should avoid using jargon and speak in a way that is both clear and understandable to the recipient [Reference Ervin, Kahn, Cohen and Weingart21].
Closed-loop communication. Closed-loop communication uses a three-step process: 1) a provider communicates a message to the receiver, 2) the receiver acknowledges that they received the information by paraphrasing and seeks clarification if required, and 3) the original provider verifies that the information was received and accurately interpreted [Reference Salik and Ashurst22,Reference Weller, Boyd and Cumin23]. This teamwork competency is important for team performance as it provides the sender with opportunities to correct potential misunderstandings before they escalate and result in incorrect actions [Reference McIntyre, Salas, Guzzo and Salas24]. Providers should be skilled in closed-loop communication as both an information provider and receiver and understand its importance when interacting with individuals from different disciplines/professions who may have different communication behaviors. Instilling this in providers will help prevent breakdowns in communication and avoid unnecessary medical errors [Reference Salik and Ashurst22].
Asking clarifying questions. This competency involves posing questions that help others share what they know and clarify what they intended. A clarifying question can operationally be defined as a question or request that is designed to seek clarification of another’s preceding utterance [Reference Apker, Mallak and Applegate25]. It is essential that providers are able and willing to ask clarifying questions of coworkers and patients to avoid errors that may result in patient safety incidents [Reference Clay-Williams and Braithwaite16]. Providers should be encouraged to ask follow-up questions when the original question did not yield all the information that they needed and ask “why” questions to clarify what another person is thinking. Existing work on teamwork training in trauma contexts includes asking clarifying questions as a targeted communication behavior [Reference Roberts, Williams and Schwind26]. As previously described, it is critical to establish psychological safety to enable team members to ask clarifying questions with confidence.
Sharing unique information. Finally, providing information that other team members or healthcare providers do not already possess is critical to effective teamwork communication. Past research indicates that communication quality is more important than communication quantity [Reference Marlow, Lacerenza, Paoletti, Burke and Salas15]. Failure to share unique information has been shown to result in medical errors and negative patient outcomes [Reference Page, Lederman, Kelly, Barry and James27]. However, sharing too much information, particularly information that is not important for providing care, may create increased cognitive demands on the receiver due to information overload. This information overload can impede provider performance, as it causes the information receiver to spend a prohibitively long time seeking the appropriate information and managing knowledge contributions [Reference Bock, Mahmood, Sharma and Kang28]. Previous work has found that psychological safety enables information sharing in teams [Reference Frazier, Fainshmidt, Klinger, Pezeshkan and Vracheva29], reinforcing the need to have psychological safety as a foundational competency for healthcare teamwork.
Coordination Skills
Coordination skills involve demonstrating effective team behaviors and understanding team dynamics. Coordination is a prominent teamwork theme that is present in several existing teamwork frameworks in healthcare [Reference Manser3,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14]. For providers to effectively coordinate within a clinical team, they must understand and appreciate the concepts of optimizing TMMs, mutual trust, mutual performance monitoring, and reflection/debriefing is essential.
Optimizing team mental models (TMM). When healthcare teams possess a TMM, all team members have a shared understanding about the patient, urgency, treatment, and next steps. Establishing a shared mental model, or having all team members on the same page, has been identified as a transportable skill integral to forming a TMM [Reference Salas, Reyes and McDaniel2]. This shared cognition has been deemed a critical driver of team performance and is present in various established teamwork frameworks and training interventions for healthcare contexts [Reference Manser3,Reference Salas, DiazGranados, Weaver and King10,Reference Chakraborti, Boonyasai, Wright and Kern12,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14,Reference Salas and Fiore30]. For healthcare teams to be effective, members must consciously optimize the TMM regarding team roles and responsibilities, care plans and contingencies, as well as system protocols and procedures. These areas should be discussed amongst the team during key coordination events such as interdisciplinary rounds, handoffs, and huddles. A strong TMM also affords teams the ability to anticipate and mitigate complications in a timely manner. When team members possess a shared awareness and common expectations, they are better able to coordinate their actions, engage in team back-up behaviors, monitor each other’s needs, and form a sense of trust.
Mutual trust. Mutual trust is the shared belief that team members will perform their roles and protect the team’s interests [Reference Salas, DiazGranados, Weaver and King10]. It is commonly listed in teamwork models and interventions, particularly in healthcare [Reference Salas, DiazGranados, Weaver and King10,Reference Chakraborti, Boonyasai, Wright and Kern12,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14]. Existing evidence indicates that teams with higher levels of intrateam trust and trust in their leader perform more effectively [Reference De Jong, Dirks and Gillespie31]. Additionally, previous research provides evidence that mutual trust is positively associated with provider and patient satisfaction [Reference Hovlin, Gillsjö, Dahl Aslan and Hallgren32,Reference Shan, Li, Ding and Wu33]. When members of the team feel valued and acknowledged for their work, mutual trust within the team can form [Reference Weller, Boyd and Cumin23]. When members of the team are unsure if they can rely on the character or ability of other members, trust erodes as well as team success [Reference Varpio, Bader, Meyer, Durning, Artino and Hamwey34]. Providers should be taught to demonstrate reliability while avoiding unrealistic commitments and acknowledge others’ contributions. For example, providers should honestly communicate their limitations (related to time, expertise, etc.) and offer alternatives while acknowledging the effect this may have on other team members’ ability to complete their own tasks. This establishes trust they can draw upon when they need a team member’s help, improving long-term functionality.
Mutual performance monitoring. Mutual performance monitoring is the ability to observe the actions of fellow team members, monitor team progress towards shared goals, and skillfully intervene by providing constructive feedback or offering assistance when needed [Reference Albon and Jewels35]. For example, if a team member notices that another member is overwhelmed or struggling with a particular task, they can engage in back-up behaviors and offer assistance. If team members are not engaging in mutual performance monitoring, they may not be situationally aware enough to recognize that a team member needs help. A strong TMM, mutual trust, and mutual performance monitoring compliment and strengthen one another. Teams that effectively engage in mutual performance monitoring demonstrate consistently higher levels of performance [Reference Fransen, Kirschner and Erkens36]. Performance monitoring is a prevalent element in healthcare teamwork frameworks and is present in existing healthcare teamwork interventions [Reference Salas, DiazGranados, Weaver and King10,Reference Chakraborti, Boonyasai, Wright and Kern12,Reference Zajac, Woods, Tannenbaum, Salas and Holladay14,Reference Clay-Williams and Braithwaite16]. Mutual performance monitoring is less effective in healthcare teams when team members' individual workloads are too cognitively demanding to monitor and provide support to other team members. Stressful work episodes tend to increase team members narrowing their focus to their own work, resulting in declines in vigilance towards monitoring others’ activities [Reference Shaw, Matthews, Warm, Finomore, Silverman and Costa37]. Additionally, mutual performance monitoring may decline if team members are considered ineffective because others had to help them. Education on this competency will help reinforce that team members must rely on one another to deliver care and normalize the essential skills of both giving and receiving feedback or assistance.
Reflection/debriefing. Debriefs are interactive, bidirectional, and reflective conversations that healthcare teams engage in, typically after an event (e.g., post-surgery) [Reference Sawyer, Eppich, Brett-Fleegler, Grant and Cheng38]. Debriefs help team members to better understand their situation, reflect on past events, and adapt their strategies as necessary [Reference Allen, Reiter-Palmon, Crowe and Scott39]. Evidence suggests that individuals and teams that participate in periodic, structured debriefs outperform (by over 20%) counterparts who do not [Reference Reyes, Tannenbaum and Salas40]. A significant portion of provider learning takes place during on-the-job experience, and reflection during debriefs helps to accelerate learning from experience [Reference Couper, Salman, Soar, Finn and Perkins41]. For example, conducting a debrief immediately after a code can help the team to recognize that they did not use closed-loop communication when discussing medication administration and make a plan to ensure they do so in the future. Teams can maximize the effectiveness of debriefs by applying the general guidelines outlined by current literature [Reference Tannenbaum and Greilich42]. Teams should minimize the time between performance and feedback, structure the debrief (i.e., structured communication), ensure a psychologically safe environment, and focus on key events and learning objectives [Reference Salas, Reyes and McDaniel2,Reference Allen, Reiter-Palmon, Crowe and Scott39]. When conducting a debrief, teams should consider several elements, including conversation facilitation (i.e., facilitator-guided vs. self-guided), conversation structure (i.e., event/performance-focused, cognitive aid driven), and process elements (i.e., conversational techniques, strategies) [Reference Sawyer, Eppich, Brett-Fleegler, Grant and Cheng38].
Discussion
The Team FIRST framework advocates for the incorporation of 10 teamwork competencies in healthcare organizations. These evidence-based competencies provide a foundation from which providers can utilize teamwork skills in any team. Team FIRST draws from the strengths identified in the TeamSTEPPS™ program, particularly its base in team science and demonstrated impact on teamwork attitudes, knowledge, and outcomes [Reference King, Battles, Baker, Henriksen, Battles and Keyes7,Reference Parker, Forsythe and Kohlmorgen43]. Team FIRST adds instructional value by integrating crucial teamwork concepts, such as creating a psychologically safe environment and team orientation, which are not included in the TeamSTEPPS™ training program [Reference King, Battles, Baker, Henriksen, Battles and Keyes7]. This expansion of the TeamSTEPPS™ framework is based on recent literature. Team FIRST integrates previous work with recent evidence to present the requisite teamwork competencies that should be emphasized in an effective teamwork training program.
Another significant obstacle impacting team training within healthcare systems is gender and racial biases. The effects of these biases in healthcare continue to be unveiled and must be considered when creating training content. Such biases affect training climate and the way healthcare team members interact with one another [Reference Salles, Awad and Goldin44,Reference Serafini, Coyer and Brown Speights45]. Providing interprofessional teamwork training has been proposed as a means of combating these biases in the literature [Reference Stephany Sanchez, Tran-Reina, Ackerman-Barger, Phung, Molla and Ton46]. Concepts present in the Team FIRST framework (i.e., team orientation) have been found to neutralize the negative effects of surface-level diversity (i.e., gender, race) on team conflict [Reference Mohammed and Angell47]. Overall, while the Team FIRST program content is theorized to reduce racial and gender biases, these biases should be rigorously evaluated throughout program implementation.
Considerations for Implementing a Team FIRST Curriculum
There are opportunities for improvement in current teamwork training interventions, such as TeamSTEPPS™, relating to training design, training climate, and training evaluation in addition to training content. Though an in-depth discussion of the Team FIRST educational strategy is beyond the scope of this paper, it important to briefly acknowledge considerations for future efforts. Teamwork training should be provided early, during the most formative stages of clinical training. Teaching new skills later requires providers to engage in unlearning, in which they must acknowledge and release prior learning to accommodate new information and behaviors, which can be difficult and mentally demanding [Reference Becker48]. The mentally demanding task of unlearning may cause providers to feel overwhelmed with their job demands, which has been shown to increase burnout [Reference Abraham, Zheng and Poghosyan49]. Therefore, we recommend that it is optimal to incorporate teamwork competency training during preclinical education to instill a foundation in team skills.
Efforts to train individuals on the Team FIRST framework should consider the benefits of different training types (e.g., information, demonstration, practice, feedback) while taking into account practical constraints, such as resource availability (e.g., time, space, funding). Additionally, existing evidence suggests that training programs should be longitudinal (i.e., spaced sessions), interprofessional, multimodal, and, facilitated [Reference Weaver, Lyons and DiazGranados50,Reference Lacerenza, Reyes, Marlow, Joseph and Salas51,Reference Fox, Onders and Hermansen-Kobulnicky52]. For training initiatives to be successful, organizational conditions must create a system and training climate for sustaining learned teamwork behaviors on-the-job [Reference Bisbey, Reyes, Traylor and Salas53]. To foster transfer of learned skills and behaviors from training and promote sustainment over time, teamwork should be incorporated into performance evaluations of more senior team members, integrating teamwork into the organizational culture [Reference Salas, DiazGranados, Weaver and King10]. Finally, the impact of team training on team performance and relevant outcomes must be rigorously evaluated [Reference Bisbey, Reyes, Traylor and Salas53]. Kirkpatrick’s (1956) framework for assessing preclinical and clinical teamwork training initiatives is recommended, which asserts there are four levels of assessing impact: reactions, learning, transfer, and results [Reference Vuurberg, Vos, Christoph and De Vos54]. The most meaningful impact is found in assessing results, which translates to team performance (e.g. patient safety, efficiency, and provider wellness) in the case of a team training program [Reference Rosen, DiazGranados and Dietz1]. If learned skills transfer to the clinical environment, this should result in improved team performance. To date, transfer of teamwork competencies into the clinical environment remains elusive. The Team FIRST curricula will aim to build on previous work to address this critical gap in healthcare.
Conclusion
There is a growing call to instill teamwork competencies in healthcare professionals. The Team FIRST framework was conceptualized as a foundation for such a training program, targeting 10 evidence-based teamwork competencies for improving interprofessional collaboration in healthcare using ubiquitous teaming contexts, such as handoffs and care transitions. The educational strategy needed to effectively deliver the Team FIRST framework will be described in future works. This will include a detailed discussion of the training design, training climate, and rigorous evaluation methods. Implementation of a team training program based on the Team FIRST framework bodes the exciting possibility of improving healthcare teams to make the medical system safer for both patients and providers.
Acknowledgments
We would like to acknowledge the contributions of the Quality Enhancement Plan (QEP) Development Steering Committee including the special contributions of Gary Reed, MD, MS, and David Klocko, MPAS, DMSc, for interprofessional integration of the curriculum, Aditee Ambardekar, MD, MSEd, Logan Gisick, PhD, and Andrew Griggs, PhD, for their mapping of teamwork competencies to learning outcomes, and William Daniel, MD, MBA, Vice President and Chief Quality Officer for UT Southwestern Medical Center, for the identification of competencies critical to health system quality and operational excellence.
The QEP is an internally funded 5-year program at UT Southwestern Medical Center for the fulfillment of an accreditation requirement of the Southern Association of Colleges and Schools.
Disclosures
There are no conflicts of interest to disclose.
The following authors served as paid consultants for the QEP: Dr Scott Tannenbaum, President of the Group for Organizational Effectiveness, Inc., Dr Elizabeth H. Lazzara, Associate Professor of Human Factors, Embry-Riddle Aeronautical University, and Dr Eduardo Salas, Chair of Psychological Sciences, Rice University.






