To the Editor—The worldwide emergence of carbapenemases has challenged antimicrobial therapy against the Enterobacteriaceae family, which are dangerous pathogens in most nosocomial infections.Reference Tamma, Goodman and Harris 1 A recent survey demonstrated that the production of this type of enzyme could be strongly related to an increased prevalence of an agent carrying it, with unfavorable clinical outcomes.Reference Rodrigues Perez 2 , Reference Giacobbe, Del Bono and Trecarichi 3
Bacterial bloodstream infections (BSIs) are serious infections associated with significant mortality and healthcare costs. Although a cause-and-effect association has not yet been properly elucidated, as previously reported by Tumbarello et al,Reference Tumbarello, Trecarichi and De Rosa 4 the emergence of Klebsiella pneumoniae carbapenemase (KPC)–producing Enterobacteriaceae as a BSI agent has been associated with a higher mortality rate than infections not due to a KPC-producing pathogen. Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae is the most prevalent carbapenemase in Brazil, and the prevalence of KPC has been increasing in most Brazilian hospitals, severely limiting the therapeutic options for the treatment of patients because β-lactams, including carbapenem, become ineffective, with only a few agents remaining active, particularly polymyxins.Reference Perez 5 The current study was performed (1) to determine the cumulative prevalence of BSIs caused by KPC-producing Enterobacteriaceae, by no carbapenemase-producing multidrug-resistant (nCP-MDR) organisms, and by K. pneumoniae species with no resistance mechanism detected, (2) to measure the impact of the presence of the bla KPC gene, and (3) to assess the polymyxin resistance rate among these pathogens in comparison to the prevalence rate of those organisms naturally resistant to this drug.
Patients followed in a surveillance cohort performed at a general-care hospital in Porto Alegre, southern Brazil, who presented positive blood cultures with enterobacterial isolates, were included in the study. Microbiological data such as bacterial identification, antimicrobial susceptibility testing, and characterization of any resistance mechanism are described in detail elsewhere.Reference Perez 6 The study period was from January 1 to December 26, 2016.
A total of 535 enterobacterial isolates were recovered from BSIs; of these, 152 (28.4%) had the bla KPC gene (notably the sole carbapenemase detected during this survey). Klebsiella pneumoniae was the only specie characterized as KPC (ie, KPC-Kp). According to the phenotypic testing, 14 isolates were ESBL producers, including 11 K. pneumoniae, 2 Escherichia coli, and 1 Enterobacter aerogenes. Another 7 isolates (6 Enterobacter cloacae and 1 E. aerogenes) were categorized as CRE isolates because they could hydrolyze at least 1 carbapenem agent (basically ertapenem). Together, both groups comprised 21 of the isolates characterized (3.9%) in this survey as an nCP-MDR group. The cumulative prevalence of these enterobacterial isolates over the study period is shown in Figure 1.
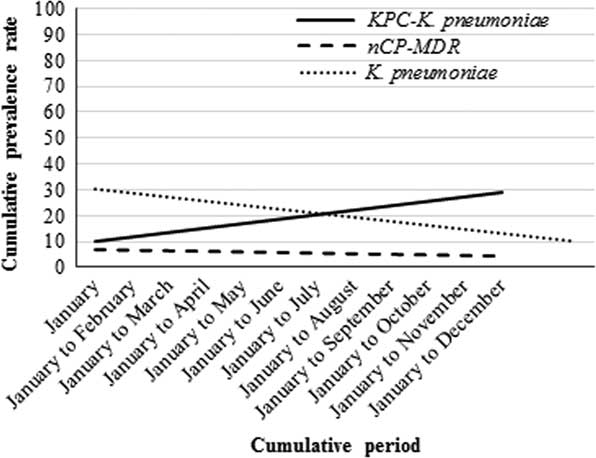
FIGURE 1 Cumulative prevalence rates of KPC, nCP-MDR, and K. pneumoniae isolates during the study period.
An increased prevalence (media±standard deviation; 19.6%±6.8) was observed for KPC-Kp in BSIs, and notably, a high rate of polymyxin B (PMB) resistance (35.3%±11.3) was also observed, although a slight decreased in the trend over the assessed period was identified (Figure 2).
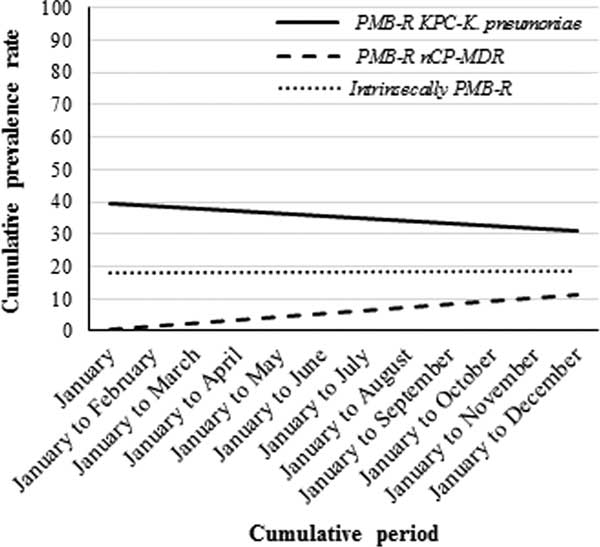
FIGURE 2 Cumulative prevalence of polymyxin-resistance rates of KPC, nCP-MDR, and intrinsically polymyxin-resistant Enterobacteriaceae isolates during the study period.
Although a stable cumulative prevalence (18.5%±1.4) had been observed among those organisms intrinsically resistant to PMB (an important issue in a setting with a high usage of this agent), we identified a trend toward increasing prevalence of polymyxin-resistant nCP-MDR isolates (6.1%±4.0), which made the selective pressure evident, even with a reduction in the overall prevalence (5.6%±1.3) of these nCP-MDR organisms during the same study period (Figure 2).
Carbapenem-resistant K. pneumoniae BSIs have been associated with higher morbidity and mortality rates than BSIs due to carbapenem-susceptible isolates.Reference Tumbarello, Viale and Viscoli 7 This finding may be due to the presence of any carbapenemase gene, especially bla KPC, which is highly endemic in Brazilian hospitals, and to the virulence and competitive fitness of K. pneumoniae regardless of its susceptibility profile.Reference Rodrigues Perez 2
In this survey, KPC production by K. pneumoniae seems to be responsible for increasing the prevalence rate of this pathogen over the study period, compared with the prevalence rates of “wild-type” K. pneumoniae and multidrug-resistant organisms with any other mechanism (eg, ESBL, ampC, or efflux pumps). Importantly, this superior prevalence seems to be driven by the acquisition of adaptive PMB resistance, which is found mainly in KPC-Kp but also in the nCP-MDR group.
Although the impact of the PMB-resistant KPC-Kp recovery on patient outcome was not evaluated in this study, the results reported here are important, particularly concerning multidrug-resistant pathogens, because KPC producers are important in the effort to reduce rates of infection, especially in a clinical site as notable as the bloodstream.
In conclusion, an increase in the prevalence of KPC-Kp recovered from the bloodstream was observed during the study period. Apart from that, KPC production probably contributes to this increased rate. A notorious emergence of polymyxin resistance among nCP-MDR isolates is worrying and may be attributed to strong selective pressure. The optimization of polymyxin use in treating BSIs must be further investigated to minimize the overall resistance development.
ACKNOWLEDGMENTS
Financial support: No financial support was provided relevant to this article.
Potential conflicts of interest: The author reports no conflicts of interest relevant to this article.






