Introduction
It is estimated that about 300,000 women die annually of pregnancy related causes in low- and middle-income countries (LMICs); 99% of global estimates (Filippi et al. Reference Filippi, Chou, Ronsmans, Graham, Say, Black, Laxminarayan, Temmerman and Walker2016). In Nigeria, about 512 maternal deaths occur in every 100,000 live births and about 556 pregnancy-related deaths occur in every 100,000 live births(National Population Commission- NPC/Nigeria and ICF 2019). Birth preparedness and complication readiness (BPACR) is a strategy that aims to support pregnant women, their families, and communities to plan adequately for births and potential complications(JHPIEGO 2004). The strategy seeks to address the common delays in pregnancy that are associated with maternal mortality. These delays occur with respect to identifying the complication, deciding to seek care, identifying, and reaching a health facility, and receiving adequate and appropriate treatment at the health facility(Thaddeus and Maine Reference Thaddeus and Maine1994; MacDonald et al. Reference MacDonald, Jackson, Charles, Periel, Jean-Baptiste, Salomon and Premilus2018). Some elements of BPACR include registration at an antenatal clinic, knowledge of danger signs, plan for where to give birth, plan for a skilled birth attendant, plan for transportation, a birth companion, and identification of compatible blood donors in case an emergency occurs(Acharya et al. Reference Acharya, Kaur, Prasuna and Rasheed2015).
Across several African countries, BPACR knowledge and practice among pregnant women has been shown to be poor(Florence et al. Reference Florence, Atuhaire, Nkfusai, Shirinde and Cumber2019; Hailu et al. Reference Hailu, Gebremariam, Alemseged and Deribe2011; Aikpitanyi et al. Reference Aikpitanyi, Ohenhen, Ugbodaga, Ojemhen, Omo-Omorodion, Ntoimo, Imongan, Balogun and Okonofua2019; Okonofua, Ntoimo, Ekezue, Ohenhen, Agholor, Gana, et al. Reference Okonofua, Ntoimo, Ekezue, Ohenhen, Agholor, Gana, Igboin, Ekwo, Imongan, Galadanci and Ogu2020; Okonofua, Ntoimo, Ekezue, Ohenhen, Agholor, Igboin, et al. Reference Okonofua, Ntoimo, Ekezue, Ohenhen, Agholor, Igboin, Maduako, Imongan, Gidago, Galadanci and Ogu2020). One study in Ethiopia revealed that 24.1% of pregnant women practice elements of the BPACR; while knowledge of at least three key danger signs during pregnancy, delivery, and postnatal period were 23.2%, 22.6%, and 9.6%, respectively(Bitew et al. Reference Bitew, Awoke and Chekol2016). Another study in Uganda revealed that the median practice score was 57.5%(Florence et al. Reference Florence, Atuhaire, Nkfusai, Shirinde and Cumber2019). A study in Ghana, found that less than 15% were able to name at least three of the five basic components of birth preparedness/complication readiness that were fulfilled(Saaka and Alhassan Reference Saaka and Alhassan2021).
A study in Edo State, Nigeria showed that less than half (134, 48.4%) of the pregnant women had good birth preparedness practice while 143 (51.6%) had poor birth preparedness. More than half of the women were saving money for delivery (158 (57.0%)); 147 (49.5%) had identified a health facility and skilled birth attendants for delivery, 135 (48.7%) had arranged for accompaniment in case of emergencies and 95 (34.3%) had made arrangements for transportation. Identification of blood donors or blood banks and facilities for emergency obstetric care was poor, with less than 15% of respondents having carried out these actions(Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016). A study conducted among women attending antenatal care in south eastern Nigeria found that knowledge of key danger signs in pregnancy was low(Ekabua et al. Reference Ekabua, Ekabua, Odusolu, Agan, Iklaki and Etokidem2011). A community-based survey in northern Nigeria among 5083 rural women recruited from three states found that birth preparedness and complication readiness practices were generally poor, with 33.2% having made no preparation for delivery; fewer than 2.5% had made provisions for a trip to the health facility at delivery and only 32.0% knew any critical danger sign relating to pregnancy and delivery(Doctor et al. Reference Doctor, Findley, Cometto and Afenyadu2013). A negligence of birth preparedness practice among pregnant women endangers these women to pregnancy complications and maternal death. In fact, a Nigerian woman has a one in 22 lifetime risk of dying during pregnancy, childbirth or postpartum/post-abortion, whereas in high income countries, the lifetime risk is one in 4900(World Health Organization 2015).
With the dearth of knowledge of maternal birth preparedness in secondary health facilities and the enduring gap between this poor knowledge and maternal birth preparedness in practice reported in previous studies, there is need for further study to understand the determinants of maternal birth preparedness among women and how this relates to knowledge of the women. Evidence from such knowledge would have policy and programme implications towards closing the gap.
The “know-do gap” refers to the gap between what is known and what is practiced(Pakenham-Walsh Reference Pakenham-Walsh2004). Whereas most efforts aimed at improving health outcomes have focused on improving knowledge through training, health education and other “knowledge infusion” strategies, it is increasingly being recognized that more knowledge may not necessarily translate to better practice(Pakenham-Walsh Reference Pakenham-Walsh2004; Eboreime, Olawepo, et al. Reference Eboreime, Olawepo, Banke-Thomas, Abejirinde and Abimbola2021; Eboreime and Banke-Thomas Reference Eboreime and Banke-Thomas2020; Eboreime et al. Reference Eboreime, Idika, Omitiran, Eboreime and Ibisomi2019). The implications of the know-do gap may be particularly demonstrated with respect to maternal health in LMICs, where much has been invested to improve knowledge of women about their reproductive health(Jolivet et al. Reference Jolivet, Moran, O’Connor, Chou, Bhardwaj, Newby, Requejo, Schaaf, Say and Langer2018). Practice, while improving, is still significantly not commensurate with the knowledge available; and maternal health indices remain sub-optimal(Banke-Thomas et al. Reference Banke-Thomas, Ayomoh, Abejirinde, Banke-Thomas, Eboreime and Ameh2021; Banke-Thomas et al. Reference Banke-Thomas, Abejirinde, Ayomoh, Banke-Thomas, Eboreime and CA2020; Eboreime Reference Eboreime2019).This study aims to bridge this gap by evaluating determinants of the know-do gap with respect to the BPACR among pregnant women attending antenatal care clinics at the Central hospital, Benin City, Nigeria. The study hypothesis is that knowledge of BPACR components and the danger signs of pregnancy by pregnant women is associated with birth preparedness practice.
Methods
Study settings
This study was conducted among pregnant women attending antenatal care clinic in a secondary health facility (Central Hospital Benin) in Benin City, Edo State, Nigeria. The hospital has 60 Obstetric beds, and an annual delivery rate of 4200 births. There are 34 doctors comprising of consultants (n=8), senior registrars (n=4), registrars (n=4), medical officer (n=8), medical house officers (interns) (n=12) in the Department of Obstetrics and Gynaecology.
Study design and sampling
This study was a cross-sectional study. The minimum sample size at 95% confidence level was determined to be 422, using the Cochran’s formula for single proportion(Kotrlik and Higgins Reference Kotrlik and Higgins2001):
n = (Z2pq)/d2, where, n = minimum sample size, “Z” is the standard normal deviate usually set at 1.96 which corresponds to 95% confidence interval, “p” is the estimated proportion of an attribute that is present in the population (i.e. proportion of pregnant women from a previous study who were well prepared for birth and its complications – 51.6%) (Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016), “q” is 1 – p, and “d” is the desired level of precision which is 5% (0.05).
Pregnant women who presented for their antenatal care visit and gave consent were included in the study, while those who were too ill to participate, or who failed to give consent were excluded from the study. Given that at the study setting, first trimester antenatal visits are uncommon, and often present as emergencies, no first trimester presentation met the criteria to be included in the study.”. 427 participants were subsequently selected using simple random sampling technique by balloting.
Data collection tools and procedure
The data collection instruments were adapted from standardized BPACR tools and indicators(JHPIEGO 2004). The data was collected between October and December 2020 using a structured interviewer-administered questionnaire which assessed the socio-demographic characteristics of participants (age, educational level, marital status, religion, occupation, monthly income), and practices concerning BPACR. Research assistants/volunteers (intern doctors, midwives, and nurses) were recruited to administer the questionnaires to participants based on the BPACR guidelines. These categories of health professionals were recruited given that the complexity of assessment involved in the study which may require some level of subject matter knowledge. The data collectors were trained to identify and score participant responses as well as assess birth preparation practices based on the BPACR guidelines. 440 eligible women were approached out of which 13 declined to participate in the study, giving a response rate of 97%. Reasons for decline were not collated.
Variables
The predictor variables of interest include knowledge of the components of BPACR (n=12) and knowledge of danger signs of pregnancy and labour (n=12). Responses were categorized such that poor knowledge indicates the ability to recognize less than eight components of BPACR or danger signs of pregnancy. Moderate and good knowledge were assessed by the ability to identify eight to 10, and greater than 10 components /danger signs, respectively.
The socio-demographic characteristics of respondents (age, marital status, level of education, occupation, religion, ethnicity, annual income, family type, and place of residence), obstetric history (gravidity, parity, utilization of antenatal clinics, past obstetric complications) served as correlates in this evaluation.
The practice of BPACR was the outcome of interest. This outcome was assessed by responses to eight criteria categorized into poor practice (less than three), moderate practice (three to five), and good practice (greater than five).
These categorizations were agreed on by subject matter experts in maternal and child health (these include gynaecologists, obstetricians, maternal and child health workers, researchers, and policymakers).
Data analysis
This was conducted using IBM SPSS (version 22.0) and STATA 14. All variables were initially summarized using frequency tables, while outcome variables were represented using pie and bar charts. Thereafter multivariable ordinal logistic regression was conducted to demonstrate associations between socio-demographic variables and the outcome variable. Further, post-estimation predictive margins were evaluated, indicating the probabilities of the various levels of practice (poor, moderate, good) with respect to the levels of knowledge of BPACR components and danger signs of pregnancy.
Results
Socio-demographic characteristics of participants
This is represented in Table 1. A total of 427 pregnant women participated in this study, 408 (95.6%) of whom were married. The mean age was 30.1 ± 5.3 years, 358 (83.8%) were urban dwellers and 208 (48.7%) of the respondents had tertiary level of education. Respondents were predominantly Christians 406 (95.1%) with monogamous families 406 (95.1%), and 214 (50.1%) of the respondents were Bini by tribe. Also, 72 (16.9%) of the respondents had an average annual income of < N 220,000 ($466). 250 (58.5%) of the respondents had their spouses employed in the informal sector, and 208 (48.7%) of the respondents had spouses with tertiary level of education.
Table 1. Socio-demographic characteristics of participants

N to $ conversion rate of 471.62 as at December 2020 according to Central Bank of Nigeria (CBN) monthly average exchange rates of the Naira. Available at https://www.cbn.gov.ng/rates/exrate.asp?year=2020&month=5
Participants’ obstetric history, utilization of antenatal clinics, and previous obstetric complications
This is provided in Table 2. 69 (16.2%) of the respondents were primigravida, while 98 (23.0%) were nullipara. Of the 329 women with previous deliveries, 54 (16.4%) of them had their last delivery at home. The average number of antenatal visits in previous pregnancy among participants was 6 ± 2 visits. 162 (37.9%) of the participants reported to have had previous pregnancy complications.
Table 2. Participants’ obstetric history, utilization of antenatal clinics, and previous obstetric complications

* Gravidity is defined as the number of times that a woman has been pregnant. A primigravida is a woman who is pregnant for the first time, while a multigravida s a woman who has been pregnant more than once.
** Parity is defined as the number of times that she has given birth to a foetus with a gestational age of 28 weeks or more, regardless of whether the child was born alive or was stillborn. A nullipara has never given birth previously, a primipara is a woman who has given birth once, a multipara has given birth more than once while a grand multipara has had ≥5 births.
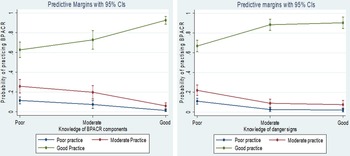
Descriptive analysis of knowledge and practice variables
This study found that out of 427 respondents, most (230, 53.9%) could identify greater than 10 components of BPACR, thus qualifying as good knowledge; while 53 (12.4%) and 144 (33.7%) had moderate (eight to 10 components) and poor (less than ten components) knowledge, respectively (Tables 3-5). One hundred and eighty-one (42%) respondents had poor knowledge of pregnancy/labour danger signs, while 157 (36.8%) and 89 (20.8%) had good and moderate knowledge, respectively. Birth preparedness practice was good among most respondents as 328 (76.8%) given that they had met more than five out of eight criteria. While 35 (8.2%) and 64 (15%) were classified as poor and moderate, having met less than three and three to five criteria, respectively (Figure 1).
Table 3. Knowledge of the Components of BPACR
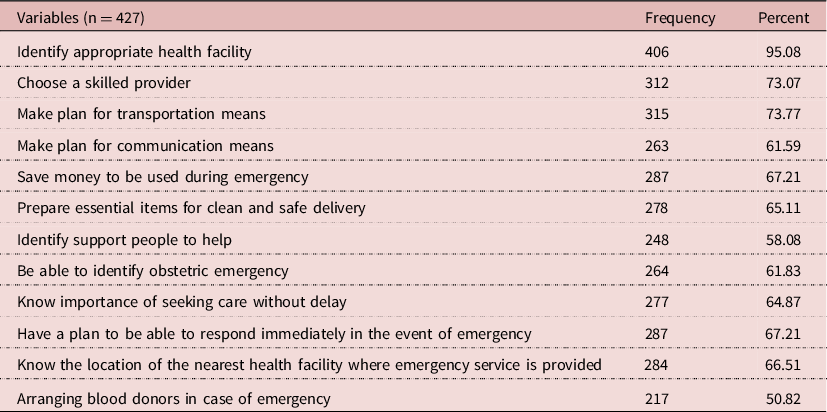
Table 4. Knowledge of the danger signs in pregnancy, labour, and delivery
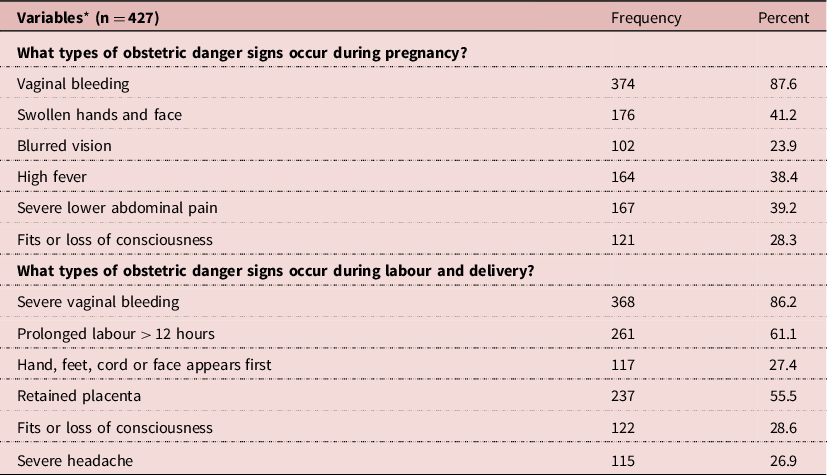
* Multiple responses.
Table 5. Practice of Birth Preparedness and Complication Readiness
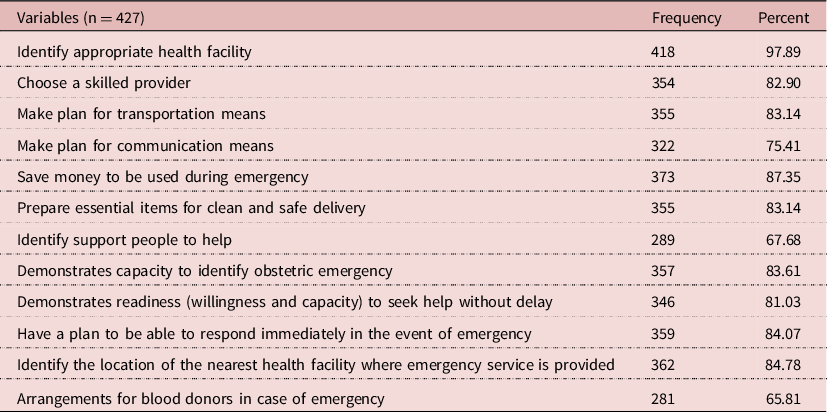

Figure 1. Descriptive analysis of knowledge and practice.
Multivariable ordinal regression analysis of association between knowledge and practice of BPACR
The results of the multivariable ordinal regression model (n=427) are presented on Table 6. The analysis revealed that respondents with poor knowledge and moderate knowledge of components of BPACR had statistically significant lower odds (OR:0.05 (95% CI: 0.02-0.13) and 0.10 (95% CI: 0.03-0.30) times, respectively) for greater practice of BPACR when compared to those with good knowledge. Likewise, respondents with poor knowledge of danger signs had statistically significant lower odds (OR: 0.08 (95% CI: 0.03-0.26) times, respectively for greater practice of BPACR when compared to those with good knowledge. Covariates are also presented on Table 6.
Table 6. Multivariable ordinal logistic regression analysis evaluating predictors of the practice of BPACR
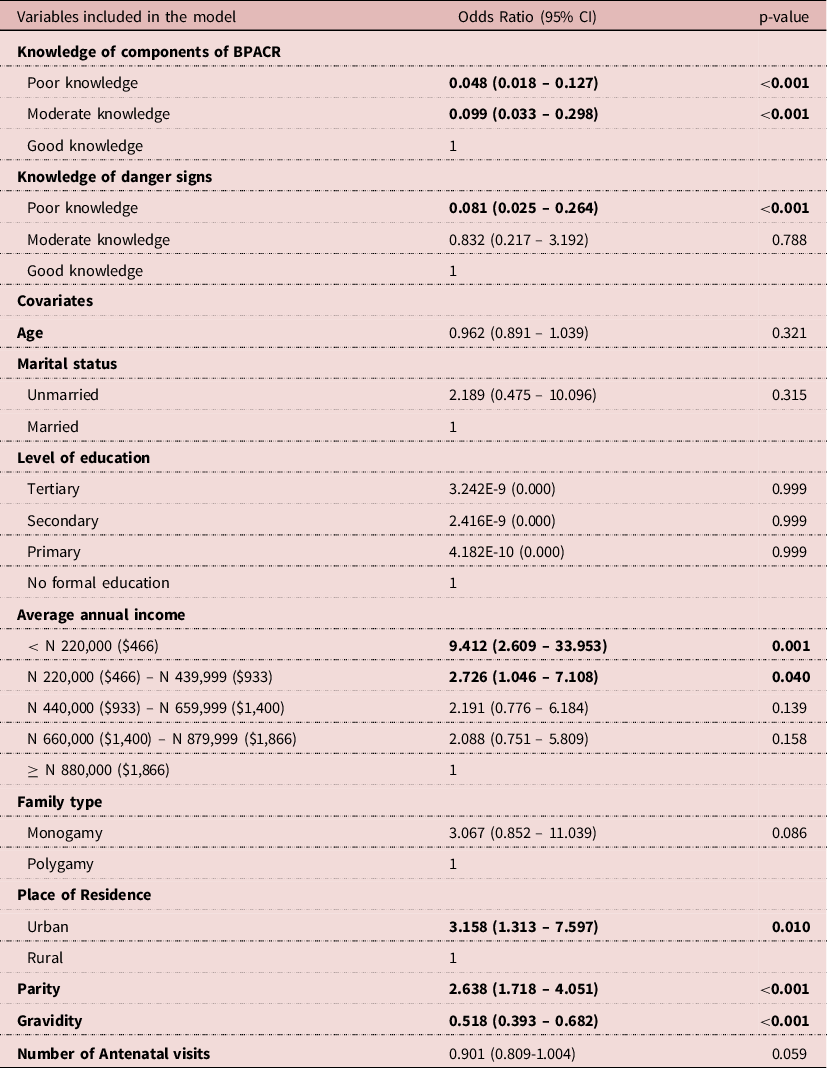
CI = Confidence Interval.
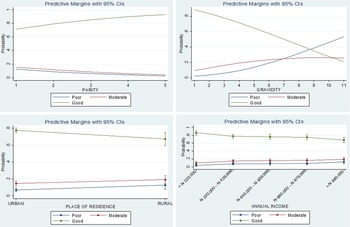
Post-estimation predictive margins
Figures 2-3 shows the results of the post-estimation predictive margins analysis.

Figure 2. Predictive margins of practicing BPACR with respect to knowledge of the BPACR components and danger signs.
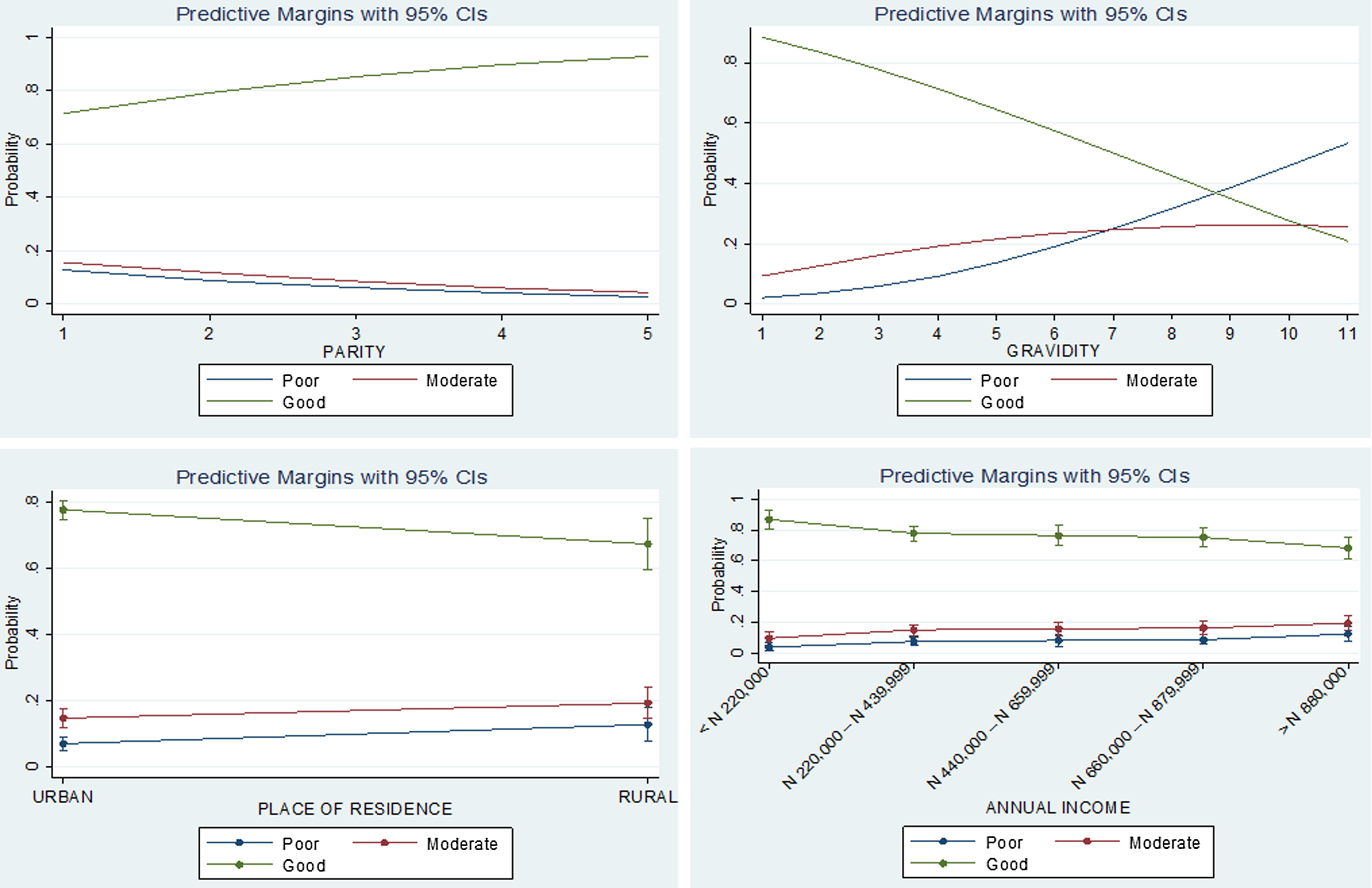
Figure 3. Predictive margins of practicing BPACR with respect to statistically significant covariates.
The probability of respondents having good practice of BPACR increased with knowledge levels from 63% (95% CI: 55-71%) among those with poor knowledge, to 73% (95% CI: 63-82%) and 93% (95% CI: 83-97%) among those with moderate and good knowledge, respectively. Conversely, the probability of poor and moderate practice decreased with increasing levels of knowledge. The probability of respondents’ practice of BPACR positively correlated with the level of knowledge such that practice increased from 67% (95% CI: 61-73%) among those with poor knowledge, to 88% (95% CI: 83-94%) and 90% (95% CI: 85-96%) among those with moderate and good knowledge, respectively. The probability of having poor to moderate practice of BPACR decreased with increasing levels of knowledge of pregnancy danger signs (Figure 2).
Post-estimation predictive margins of statistically significant covariates are demonstrated in Figure 3. The probability of good birth preparedness practice increased with parity from 71% among women who had given birth once to 93% among women who had experienced five child births. Conversely, the probability of poor birth preparedness decreased with increasing number of pregnancies from 89% among women experiencing their first pregnancy to 21% among women experiencing their 11th pregnancy. Women residing in urban settings had a 78% (95%CI: 75-81%) probability of having good birth preparedness practice, as compared to rural dwelling women had a 68% (95%CI: 60-75%). Women with an annual income of less than N220,000 ($466) had the highest probability of good birth preparedness (87%, 95%CI: 80-93%). This probability reduced with increasing income to 68% (95%CI: 61-76%) among women with annual income above N880,000 ($1,866).
Discussion
This study found that about 77% of respondents had good birth preparedness practice. Also, the findings suggest that knowledge, though critical to ensuring practice, is insufficient on its own to optimize practice, as the multivariate regression analysis demonstrates.
Pareto analysis indicates that about 80% of BPACR practice was in relation to identifying an appropriate health facility for delivery, saving money for possible emergency, identifying the location of the nearest health facility where emergency services can be provided, having a plan to be able to respond immediately in the event of an emergency, having the capacity to identify an obstetric emergency, making plans for transportation, preparing essential items for clean and safe delivery, and choose a skilled provider. Ibadin and colleagues found a similar prioritization (though in a slightly different order) in their study in another community in Edo state, Nigeria(Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016). As with findings form this current study, identification of blood donors or blood banks also had the least preparation.
Approximately 54% of respondents in this study had good knowledge of the components of BPACR, while only 36.8% good knowledge of the danger signs of pregnancy and labour. Majority of respondents had knowledge on how to identify an appropriate health facility (95.1%), choose a skilled provider (73.1%), make plan for transportation (73.8%), save money for communication (61.6%), prepare essential items for clean and safe delivery (65.1%), identify obstetric emergency (61.8%) and make arrangements for blood donors in case of emergency 50.8%. However, another also study conducted in Edo state, Nigeria had a seemingly contrasting finding. The authors reported less than half (48.4%) of the respondents with good birth preparedness(Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016). But considering that the study was conducted in a rural health facility, this finding aligns with the outcome of the multivariable regression which demonstrated that rural dwellers have greater tendency towards poor BPACR practice than urban dwellers. An explanation could be that rural dwellers are more likely to rely on traditional birth attendants (TBAs) for information on birth preparedness(Iwu et al. Reference Iwu, Uwakwe, Oluoha, Duru and Nwaigbo2021; Ohaja et al. Reference Ohaja, Murphy-Lawless and Dunlea2020). Thus underscores the importance of prioritizing interventions aimed at training TBAs in BPACR. Further, rural communities may lack infrastructure and services needed for birth preparedness. For example, many rural communities in Nigeria have limited access to blood banks and transfusion services(Oreh et al. Reference Oreh, Irechukwu, Biyama, Nnabuihe, Ihimekpen, Oshiame, Bozegha, Leo-Nnadi, Izedonmwen, Oga, Suberu, Odiabara and Amedu2022).
The weakest link in the knowledge to practice continuum was with the knowledge of danger signs in pregnancy, labour and delivery where about 42% of respondents had poor knowledge, even though the majority of respondents fell into the moderate and good knowledge categories. These findings are proximal to another Nigerian study which found knowledge of danger signs in pregnancy to be 62.5%(Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016), as well as a study in Ethiopia which found knowledge of danger signs to be high(56.9%). Whereas these studies considered knowledge above 50% to be high, the authors opine that much work needs to be done to educate women on the danger signs of pregnancy/labour and delivery, given that such knowledge could potentially reduce delays attributed to the high maternal and foetal morbidity and mortality in sub-Saharan Africa.
This study found that bleeding, prolonged labour, retained placenta and abdominal pain (39.2%) were the most identified danger signs by participants. This finding resonates with another in a similar Nigerian context (Ibadin et al. Reference Ibadin, Adam, Adeleye and Okojie2016), as well as in Ethiopia (Mulugeta et al. Reference Mulugeta, Giru, Berhanu and Demelew2020). But in a study conducted in Tanzania only about 10% of respondents identified vaginal bleeding as danger sign, despite about 98% of the women having attended antenatal care at least once (Pembe et al. Reference Pembe, Urassa, Carlstedt, Lindmark, Nystrom and Darj2009). The implication is that antenatal clinic attendance is insufficient to improve knowledge. Efforts must be made to enhance the content and delivery strategy of health education during antenatal care. Applying contextually appropriate strategies to improve knowledge of mothers about danger signs can improve care-seeking behaviour during obstetric emergencies.
This study indicates, somewhat intuitively, that increase in the knowledge of BPACR components and pregnancy danger signs correlates with an increase in practice. This finding resonates with existing knowledge from the literature regarding closing the know-do gap as applies specifically to BPACR in comparable sub-Saharan African contexts(Florence et al. Reference Florence, Atuhaire, Nkfusai, Shirinde and Cumber2019; Bitew et al. Reference Bitew, Awoke and Chekol2016);and more generally to other interventions or contexts(Samuel et al. Reference Samuel, Martinez, Chen, Markatou and Talal2018; Eboreime Reference Eboreime2019; Eboreime, Olawepo, et al. Reference Eboreime, Olawepo, Banke-Thomas, Abejirinde and Abimbola2021; Eboreime and Banke-Thomas Reference Eboreime and Banke-Thomas2020; Pham et al. Reference Pham, Byrkit, Pham, Pham and Nguyen2013; Eboreime, Itanyi, et al. Reference Eboreime, Itanyi, Ogidi, Iheanacho, Olayiwola, Onoka and Ezeanolue2021).
An interesting observation was made in this study context, however. As with other studies, the probability of increase in good practice rose significantly better when knowledge of the components of BPACR transitioned from moderate to good, compared to a transition from poor to moderate knowledge. But the picture became slightly different with respect to the knowledge of danger signs of pregnancy where an increase in knowledge from moderate to good did not result in significantly better practice. The implication is that, for this context, the optimum number of danger signs women need to know to improve practice may be between eight to ten. Beyond this number, practice may not change significantly. Thus, birth preparedness practice by pregnant women may be more effectively improved by continuously increasing the women’s knowledge about the components of BPACR than by increasing their knowledge about the danger signs in pregnancy/labour/delivery beyond the optimum point. This finding may have practical implications for designing effective health education and training programmes as relates to BPACR.
This study is not without limitations. Being a hospital-based study, the findings may have limited generalizability as the study sample may not be representative of the general population of pregnant women in Benin City. However, given that study participants were randomly selected, the findings may be considered reflective of women attending antenatal clinics at the Central Hospital, Benin City, and lessons learned may have reasonable applicability beyond the study context.
The use of health workers for data collection may raise concerns about balance of power and its influence on responder bias. However, this approach was necessitated and approved by the ethics committee given the COVID-19 restrictions at the time of data collection. Healthcare workers adhered strictly to the COVID-19/Infection Prevention protocol already established in the hospital. Further, subject matter knowledge was necessary for data collection. Potential responder bias resulting from this was mitigated by ensuring that the managing physicians and nurses were not involved in collecting data from their own patients.
Self-reporting could also pose potential recall bias on the part of the responder. Further, the data collection approach could result in potential interviewer bias, particularly with respect to scoring some of the practice indicators given the potential subjectivity in assessment. However, this bias is hopefully mitigated by the training of the data collectors.
The findings of this study may be interpreted with caution with respect to temporal direction of association between knowledge and practice considering that the study design is cross-sectional, thus does not intend to infer causality.
The grading and categorization of variables were done by subject matter experts. While this may introduce potential bias, given that there is no standardized scale for knowledge and practice of BPACR, this approach was the most feasible. Further, the three-level categorization of the outcome variable, and the application of an ordinal logistic regression can be considered a strength over most previously published research on the topic which applied binary logistic regression. This is because the approach used in this study reduces potential bias introduced by an arbitrary dichotomization of outcomes into poor and good practice by introducing a moderate practice class.
Conclusion
The proportion of women with knowledge and practice of BPACR is relatively high among the study respondents. But the high maternal morbidity and mortality in Nigeria makes the impact or poor knowledge and practice significant if extrapolated to the population level. Whereas knowledge facilitation such as educating mothers and communities, as well as training health workers on effective knowledge translation can significantly improve practice, the effect of these interventions may not be optimal, as this study demonstrates. Interventions to facilitate practice at the community level may further improve outcomes and bridge the know-do gap. For example, training of TBAs to prepare mothers for pregnancy, labour, and delivery. Reactivation of home visits by community health extension workers to complement facility-based support and care is recommended, considering that this study suggests that antenatal clinic visits may not be significantly associated with BPACR practice. Future research involving multiple centers and communities will be helpful to further explore the population wide determinants of closing the know-do gap with respect to BPACR.
Acknowledgements
The authors acknowledge the support of the staff (particularly the midwives) of the Department of Obstetrics And Gynaecology, Central Hospital, Benin City for their support.
Ethical considerations
Ethical approval for this study was obtained from the ethics and research committee of Hospital Management Board, Edo State (Ref: A732/T/1; September 11, 2020) and permission was sought from the management of Central Hospital Benin. Verbal informed consent was obtained from the participants, and privacy, confidentiality of information was guaranteed. Participation was voluntary, and as such those who consented were allowed to opt out of the study at any point in time if they felt uncomfortable.
Conflicts of interest
The authors declare no competing interests
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.