To the Editor—The nosocomial influenza rate among cancer and severely immunosuppressed patients (ie, transplant recipients) has been reported to be between 9% and 28%. Reference Chemaly, Ghosh and Bodey1,Reference Renaud and Campbell2 Healthcare workers (HCWs) with influenza can transmit the virus to patients, and this transmission can be particularly problematic when HCW vaccination rates are low. Reference Blanco, Eisenberg, Stillwell and Foxman3 High rates of influenza vaccination in HCWs have been associated with lower morbidity and mortality among patients in long-term care facilities. Reference Horcajada, Pumarola and Martínez4
During the coronavirus disease 2019 (COVID-19) pandemic, most hospitals established measures to limit the spread of severe acute respiratory coronavirus virus 2 (SARS-CoV-2); therefore, the transmission of other respiratory viruses was also limited. In this study, we examined the demographics, clinical presentation, and outcomes of patients with nosocomial influenza in a Mexican cancer-referral center over 13 years, including the first year of the COVID-19 pandemic.
Methods
This cross-sectional study was conducted from 2008 to 2021 at the Instituto Nacional de Cancerologia, an oncological referral center in Mexico City. We included adult patients with solid and hematological malignancies and confirmed nosocomial influenza. Informed consent was waived, and patient confidentiality was protected. Nosocomial influenza was suspected in patients who developed influenza-like symptoms >48 hours after admission. Influenza was confirmed by polymerase chain reaction from nasal swabs, endotracheal tube aspirates, or bronchoalveolar lavage samples.
Demographic and clinical data were obtained from influenza surveillance databases and electronic medical records. Categorical variables are described using proportions, and continuous variables are described using mean and standard deviation (SD) or median and interquartile range (IQR). The Pearson χ Reference Renaud and Campbell2 test was used to compare categorical variables, the Student t test was used for means, and the Mann-Whitney U test was used for medians. In addition, we compared HCW influenza vaccination rates from 2015 to 2021.
Before COVID-19, any patient with an influenza-like illness was isolated in an individual room, with droplet and contact precautions. Relatives of patients with influenza-like illnesses had to wear surgical masks, and hand hygiene was also reinforced. In March 2020, tighter infection control practices were introduced, with mandatory face mask use, increased hand hygiene, restrictions for accompanying persons, and cohort isolation in a specific in-hospital ward for patients under evaluation for respiratory symptoms.
Results
In total, 1,808 influenza-like illness cases were evaluated between 2008 and March 2021. Among them, 289 (15.3%) had confirmed influenza. Of these, 30 (10.38%) were diagnosed with nosocomial influenza. The median number of nosocomial influenza cases per year was 2 (IQR, 0–3).
Overall, the median age of these patients was 43 years (IQR, 22–55), and most (70%) had hematologic malignancies. Oseltamivir was prescribed for 29 patients (96.6%). In addition, 10 patients (33.3%) with nosocomial influenza died. Clinical and sociodemographic characteristics are summarized in Table 1.
Table 1. Clinical and Sociodemographic Characteristics, and Comparison Between Alive and Dead Cases
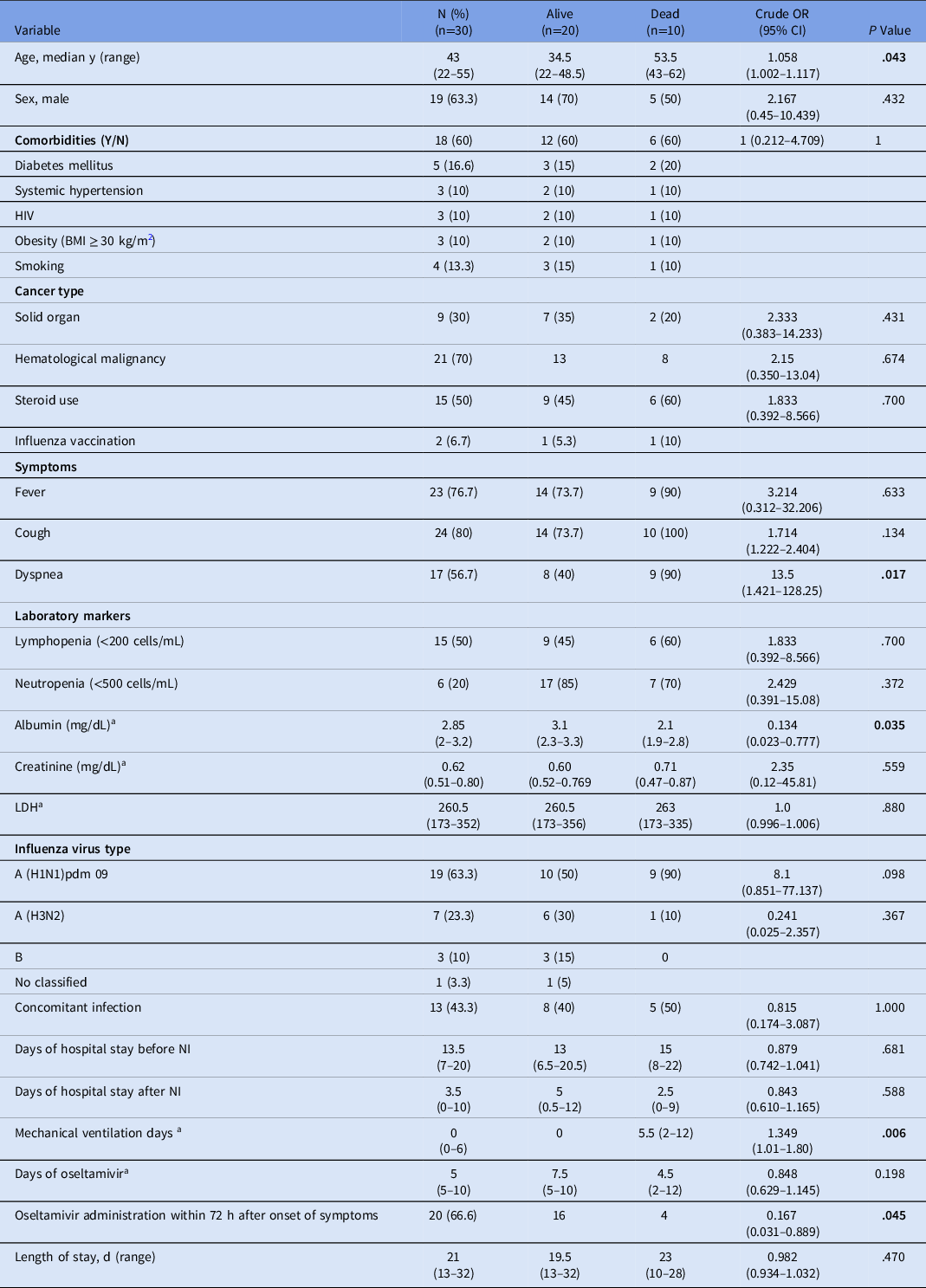
Note. IQR, interquartile range; OR, odds ratio; HIV, human immunodeficiency virus; LDH, lactate dehydrogenase; NI, nosocomial influenza.
a We used median and IQR for continuous variables.
Influenza vaccination among HCWs increased from 2015 to 2019, with a sharp increase in 2020. From 2015 to 2019, the mean rate of influenza vaccination among HCWs was 54.64%. In 2020, this rate increased to 95.3%, and there were no cases of community-acquired influenza nor nosocomial influenza. The difference between 2015 to 2019 versus 2020 was statistically significant (P < .001).
Discussion
In this observational study, we reviewed 30 cases of nosocomial influenza in 13 years. Notably, one-third of the patients died, and we observed that early administration of oseltamivir (within 72 hours after onset of symptoms) was related to survival. In February 2014, during the 2013–2014 season, we had an influenza outbreak among unvaccinated HCWs that correlated with a remarkable increment of nosocomial influenza cases in patients (Supplementary Fig. 1 online).
A few studies have described nosocomial influenza among cancer patients. A study from MD Anderson Cancer Center in Texas reported a nosocomial influenza rate between 0% and 6.6% in a 7-year period, Reference Frenzel, Chemaly and Ariza-Heredia5 which is lower than ours. In contrast, a German study reported a nosocomial influenza rate of 20%. Reference Huzly, Kurz, Ebner, Dettenkofer and Panning6 Regarding mortality, Chemaly et al Reference Chemaly, Ghosh and Bodey1 in 2006 reported a rate of 15%, which is lower than ours. This difference may be related to more advanced underlying malignancies in and poorer functional status of our patients. Also, 50% of our patients had lymphopenia (<200 cells/mm Reference Blanco, Eisenberg, Stillwell and Foxman3 ), which has been reported as an independent factor for a poor prognosis and death. Reference Chemaly, Ghosh and Bodey1 Similar to our report, early initiation of oseltamivir was associated with better outcomes. Reference Chow, Doyle and Uyeki7 In our study, coinfections were not associated with increased mortality.
At the beginning of 2020, the COVID-19 pandemic caused the reformulation of infection control practices worldwide. Mandatory face mask use and social distancing have probably contributed to lower transmission of respiratory infections. Reference Leung and Plotkin8 These measures have positively affected the dynamics of respiratory virus transmission, and we need to consider those for regular medical care, even when the pandemic comes to an end. It is also remarkable that vaccination against influenza in HCWs in our hospital almost doubled last year, demonstrating that wide vaccine availability, political will, and most importantly, HCW responses are critical factors in prevention.
This study has several limitations. It included a small number of cases over an extended study period. In addition, this is a single-center report, so the results may not be generalizable. During the first years after the 2009 pandemic influenza, testing was limited. Finally, influenza vaccination rates among HCWs were available from 2015 onward.
The rate of nosocomial influenza in cancer patients at our institution is similar to that of other reports. The high mortality rate highlights the relevance of strict infection control and prevention practices in cancer patients and the importance of HCW vaccination as a preventive measure to reduce influenza in hospitals. The increased uptake of the influenza vaccine in 2020, universal face mask use, social distancing, and more strict visitor policies correlated to the absence of cases of influenza in 2020, and should make us reconsider infection prevention policies overall.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2021.337
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.






