LEARNING OBJECTIVES
-
Gain a basic understanding of religious principles governing dietary laws and their influence on concordance with psychotropic medication
-
Be able to discuss confidently with patients the presence of religiously or ethically forbidden ingredients in medication
-
Be able to offer alternative strategies to address medication non-adherence secondary to religious, ethical or personal beliefs
Medication is probably the most frequently prescribed treatment in mental healthcare and non-adherence has a significant impact on patients’ lives and well-being (Reference Weiden and OlfsonWeiden 1995; Reference Patel and DavidPatel 2005). Although religious beliefs may not markedly influence medication adherence in patients who present to psychiatric services (Reference DeinDein 2004), non-adherence should prompt a comprehensive assessment of the patient’s demographics, social circumstances, and cultural and religious beliefs (Reference Subach and Abdul-EzzSubach 1999; Reference Sattar, Ahmed and MajeedSattar 2004a).
In psychiatric practice, it is not uncommon to come across patients who refuse any psychiatric intervention, placing their faith in a spiritual recovery enabled by their religious beliefs (Reference Campion and BhugraCampion 1997; Reference Koenig, McCullough and LarsonKoenig 2001). Although religious laws do not usually restrict the taking of psychotropic medication, many do forbid consumption of the animal derivatives, particularly gelatin and stearic acid, that many psychotropics contain. This has major implications, for example, for patients who follow Judaism, Islam, Hinduism, Buddhism and Seventh Day Adventism (Reference Singsit and NaikSingsit 2001; Reference Leung, Davies and WongLeung 2005). There are also over 4 million vegetarians in the UK and the number is ever growing (Food Standards Agency 2005).
The experience of illness can be akin to a spiritual event for many psychiatric patients. Patients, carers and their families may be more likely to consult religious teachings during times of illness (Reference Borras, Mohr and HugueletBorras 2007; Reference Chatters, Taylor and LincolnChatters 2008). A discussion about the presence of animal products in medications not only opens the door to a dialogue with people for whom the psychiatrist pledges to care but also shows a willingness to acknowledge that their beliefs are important to the psychiatrist (Reference Huguelet, Mohr and BrandtHuguelet 2006). Lack of consideration for these matters can impair the doctor–patient relationship (Reference Khokhar, Hameed and AliKhokhar 2008). Although there has been little research in this area (e.g. Reference Mohr and HugueletMohr 2004; Reference Sattar, Ahmed and MadisonSattar 2004b; Reference Dogra and KarimDogra 2005), the fostering of patients’ trust through a shared understanding of their illness can improve treatment adherence, reduce relapse rates and thus help to reduce their mental distress (Reference Borras, Mohr and HugueletBorras 2007). There is also evidence to suggest that the patients of clinicians who respect their perspectives have improved healthcare outcomes and feel better understood, respected and valued as partners in their own care (Reference Secker and HardingSecker 2002). Reference WilliamsWilliams (1997) argued that, when culture is overlooked, incorrect and even harmful decisions may be made. Good patient care is not only culturally aware, but also religiously sensitive. Such care requires commitment, willingness to honour differences and openness to exploring diversity. It also requires mental health professionals to be more aware of issues of religion and spirituality and educated about the major teachings of diverse religious groups (Reference MeyerMeyer 1988).
Dietary requirements and food laws from a religious perspective
The concept of clean and unclean animals
Followers of many religions forbid the consumption of certain animals, which are commonly referred to as ‘unclean’. Some religions also have specific requirements with regard to the slaughtering of animals and the preparation of meat and meat products. These issues are prominent in Judaism and Islam, where pork is not consumed, and they are largely used as the basis for identifying ‘taboo’ meat proscribed by religious dietary laws. For certain faiths, medicines derived from sources that are forbidden can present huge problems for patients, carers as well as healthcare professionals. Methods for determining what is and is not acceptable among people of particular religious creeds remain a source of discussion by religious leaders and scholars (Reference Eriksson, Burcharth and RosenbergEriksson 2013).
The Abrahamic faiths
A brief word on the concept of Abrahamic faiths and their common ground will aid the understanding of references to non-Abrahamic faiths later in this article. Judaism, Christianity and Islam are the three religions collectively referred to as the Abrahamic faiths. All are monotheistic religions and are unified in their belief that God revealed himself to the Prophet Abraham. Thus, the Prophet Abraham is the common forefather of these faiths, which currently embrace more than half of the world’s population. According to this trio of religions, God is the Divine Creator and source of all moral law. All other faiths, including the dharmic religions and the Chinese religions of East Asia, are therefore termed non-Abrahamic faiths. The non-Abrahamic faiths that we discuss in this article are Hinduism, Buddhism and Sikhism.
Judaism
Views on animals
God created animals and His covenant with the animals was to promise that they would be properly looked after. God created humans and gave them dominion over the animals. Humans are given detailed rules and regulations on how to take care of animals. Several passages in Jewish scriptures exhibit concern for the psychological and physical well-being of animals. For example, Exodus 23:5 and Deuteronomy 22:4 both talk about relieving animals of their burden, regardless of whether their owner is a friend or an enemy.
Jewish dietary laws
Kashrut comes from the Hebrew root Kaf-Shin-Reish, meaning fit, proper or correct. According to Jewish dietary laws (Kashrut), only animals that chew the cud (ruminate) and have cloven hooves, for example cows, can be consumed. Pigs are forbidden, as they do not chew the cud despite having cloven hooves. Horses and camels do chew the cud, but do not have cloven hooves. Thus, Jews are forbidden to eat pork, as swine are considered to be unclean (Reference Dresner and SiegelDresner 1980).
Meat must be kosher, which is achieved by the ritual slaughter of the animal (schechita) with respect and compassion by a religious Jew who is trained and licensed. Kosher dietary laws are observed all year round, not just during Pesach (Passover). Any products of a non-kosher animal are also non-kosher (Reference HeberHeber 1995). Gelatin is one such product, and within the past 20 years, kosher gelatin has become available: some of this is derived from cows or fish and some is derived from a plant or seaweed base using agar or pectin.
What does this mean for the Jewish patient?
According to Jewish teachings, people who are ill fall into one of three categories:
-
choleh sheyesh bo sakanah: someone who is ill and whose life may be in danger as a result of the illness;
-
choleh she’ain bo sakanah: someone who is ill but whose life is not likely to be in danger; this includes those who are bedridden and those who are not functioning at normal levels owing to pain or illness;
-
one who has a michush: someone who is uncomfortable but is able to maintain routine activities despite discomfort, for example those with a headache or indigestion.
Jewish medical ethics derived from Jewish law (halacha) provide guidance on the use of medicinal substances. All food and dietary additives or medicines that are swallowed must contain only kosher ingredients. However, porcine or other non-kosher material administered in a non-edible manner is permitted in the case of choleh sheyesh bo sakanah and choleh she’ain bo sakanah. Therefore, there are no restrictions or prohibitions on the injection or administration by other parenteral methods of non-kosher products such as porcine insulin. However, a rabbi must be consulted in matters pertaining to consumption of non-kosher medication by someone who has a michush (Reference AdlerAdler 2007).
Islam
Views on animals
Islam, like the other Abrahamic faiths, sees animals in a very positive light. It considers them as signs and worshippers of God, hence worthy of great respect. The Qur’an refers to animals as communities in their own right, stating: ‘And there is no creature on the earth or bird that flies with wings except [that they are] communities like you’ (Qur’an 6:38). Rules of interaction with animals are addressed in the Hadith (the collective body of traditions relating to Muhammad and his companions), in which Muhammad compares acts of cruelty to animals with cruel acts to humans.
Islamic dietary laws
According to Islamic dietary laws, several animals are considered unclean and not to be eaten (haraam), while others are permitted (halaal) as long as they have been killed or slaughtered in the correct manner (dabiaah). The Qu’ran states this clearly: ‘Forbidden to you are: dead meat, blood, the flesh of swine, and that on which hath been invoked the name of other than Allah; that which hath been killed by strangling, or by a violent blow, or by a headlong fall, or by being gored to death; that which hath been eaten by a wild animal; unless ye are able to slaughter it; that which is sacrificed on stone [Altar?]; [forbidden] also is the division by raffling with arrows: that is impiety’ (Qur’an 5:3).
According to Islamic law (sharee’ah), the most important condition of dabiaah is that basmala or tasmiyah (reciting the name of Allah) be performed at the time of slaughter. Several verses of the Qu’ran explain that meat of those animals whose slaughter was not performed in this manner is forbidden. The meat of animals slaughtered by a kafir (non-believer) or mushrik (polytheist) is also forbidden. This means that, although Muslims are permitted to eat bovine meat, if it has not been slaughtered according to the Islamic laws, then it cannot be consumed (Reference UsmaniUsmani 2006).
The products of a non-halaal animal are also considered non-halaal. However, in the case of gelatin, there is a considerable variation in views. One less accepted belief is that, owing to change in its chemical nature (istihalah) during the process of its derivation from animal hides and bones, gelatin derived from non-halaal animals becomes halaal (Reference Hashim, Ismail and SaziliHashim 2009).
What does this mean for the Muslim patient?
If the prescription is ‘life saving’ then all treatments are permissible. If ‘preventive’ or ‘life enhancing’, then there is some room for doubt and a number of Muslims either use their own discretion or consult an Imam (a religious leader). As a broad guide: if a medication contains alcohol or pig products, then it must not be taken orally – but parenteral or external application is probably permitted. The use of porcine-derived material for life-threatening illness may become temporarily exempt from the dietary laws, but the decision requires discussion with religious leaders or Imams (Reference Gatrad and SheikhGatrad 2001).
Comparison of Judaism and Islam
Table 1 outlines the main differences between Jewish and Islamic dietary laws. In reviewing these, healthcare professionals should recognise that within each faith there are many schools of thought. In addition, different cultures will have different customs that will be intertwined with religious law. The extent to which people adhere to each religious teaching is a matter for the individual. The intensity of religious practice may vary according to an individual’s situation: for example, as mentioned earlier, patients, carers and families may place greater importance on religious needs at times of ill health. Adherence to religious dietary laws in relation to medication is a wide-ranging issue and heterogeneous religious communities can vary in individual practices.
TABLE 1 Dietary laws in Judaism and Islam: principle differences and similarities
Christianity
Views on animals
The Christian view on animals has varied over the course of time. Christian thinkers in the past believed that humans were far superior to animals and that there were few, if any, moral obligations towards animals. However, modern Christians take a much more pro-animal line and believe that human dominion over nature should be seen as stewardship and partnership rather than domination and exploitation (Reference KemmererKemmerer 2011).
Christian dietary laws
In the very early days of Christianity it was debated whether converts ought to follow Jewish customs (including the dietary laws) or not. The commonly held theological position is that with the death and resurrection of Jesus, the ‘old Covenant’ and its restrictions no longer apply. The Epistle of Paul to the Colossians states: ‘He forgave us all our sins, having cancelled the written code, with its regulations […] Therefore do not let anyone judge you by what you eat or drink, or with regard to a religious festival, a New Moon celebration or a Sabbath day’ (Colossians 2:13–14, 16). Accordingly, Christians permitted themselves to eat pork, despite the fact that the Torah prohibits it. The main modern day exception to this is the denomination of Seventh Day Adventists, whose cofounder Ellen G. White was a proponent of vegetarianism. Adventists do not eat pork or other unclean meat as identified in the Book of Leviticus. Many Seventh Day Adventists avoid meat for health reasons, although vegetarianism is not a requirement.
What does this mean for the Christian patient?
The question of taking medication is most straight forward in Christianity. Christians, with the exception of Seventh Day Adventists, are generally permitted to consume all animals, including pork, as well as any drug excipients derived from animals.
Ahimsa, non-Abrahamic faiths and vegetarianism
Ahimsa
Ahimsa is a religious doctrine that advocates nonviolence and a respect for all life. It is interpreted most often as meaning peace and reverence towards all sentient beings. Ahimsa is the core of Hinduism, Jainism and Buddhism. Hinduism’s vast scriptures widely prescribe vegetarianism based on profound links between ahimsa, karma (ill effects on oneself as a result of mistreatment of others) and reincarnation (the beginning of a new life for one’s soul after biological death) to achieve a balance in one’s ‘spiritual ecology’. Most of the secular motivations for vegetarianism, such as ethical considerations and nutrition, apply to Hindu, Buddhist and Jain motivation as well (Reference Walters and PortmessWalters 2001).
Hinduism
Hindu teachers and scriptures often expressly encourage a vegetarian diet in which meat, fish, poultry and eggs are forbidden, although dairy products are allowed. However, not all Hindus are vegetarians. Regardless of whether vegetarian or meat eaters, Hindus almost universally avoid beef since they consider the cow sacred.
Buddhism
Siddhartha Gautama, the Buddha, is widely believed to be a Hindu by birth and he accepted many of the Hindu core doctrines, such as karma. He explicitly taught vegetarianism as a component of his general instruction to be mindful and compassionate. It is not surprising that the term ‘sentient being’ is used repeatedly in Buddhist writings and refers to both humans and animals. Buddhists aim to relieve the sufferings of all sentient beings. Rebirth is a basic tenet of Buddhism and it includes rebirth of humans as other animals and vice versa. As a result, many Buddhists do not kill animals and many also do not eat meat (Reference PhelpsPhelps 2004). Many vegetarian Buddhists are not vegan, but for those who are, their choice often rests on objections to the conditions in which the animals producing products such as milk and eggs are raised. There are, however, no universally agreed rules for permitted and not-permitted foods in Buddhism (Reference KemmererKemmerer 2011).
Sikhism
Sikhism arose as a separate religion from Hinduism about 500 years ago, but it is still markedly influenced by Hinduism: it shares a culture and a world view involving ideas of karma, rebirth and an emphasis on individuals and families to maintain a lifestyle conducive to physical and mental health (Reference GrahamGraham 2004). Sikhism, like many other world faiths, has a number of different sects. In the Akhand Kirtani Jatha sect, eating any meat is believed to be forbidden, yet this is not a universally held belief among Sikhs (Reference Eriksson, Burcharth and RosenbergEriksson 2013). Sikhs can only eat the meat of an animal slaughtered by the jhatka method, whereby the animal is killed quickly, with one stroke of the weapon causing instantaneous death. Vegetarian sikhs are prohibited from consuming animal-derived ingredients such as gelatin, certain thickeners (e.g. chitin) and animal-based lecithin emulsifiers.
Vegetarians and vegans
Vegetarianism is not a religion, but rather the practice of not eating meat, including beef, poultry, fish and their by-products (such as lard, tallow, gelatin, rennet and cochineal). The exclusion may also extend to dairy products and eggs. Vegans may be considered the strictest vegetarians, but vegetarianism encompasses a host of other subtypes (Table 2). Motivations behind various practices of vegetarianism are listed in Box 1.
TABLE 2 Various practices of vegetarianism
BOX 1 Motivations behind various practices of vegetarianism
| Religious | Individuals may choose to live a vegetarian life on the basis of their religious values, for example in Hinduism and Jainism. |
| Nutritional | Vegetarians argue that being vegetarian has numerous health benefits and prevents incidence of diseases such as ischaemic heart disease, hypertension and type 2 diabetes. |
| Ethical | Issues include the inhumane treatment of animals before slaughter, animal rights and that animals have the right to life particularly as there are alternative sources of nourishment and sustenance. |
| Environmental | Environmental vegetarianism revolves around the concern that eating meat is environmentally damaging and that production of meat and animal products on a mass scale are environmentally unsustainable. Animal agriculture is a cause of land degradation, loss of biodiversity, air and water pollution as well as being a major contributor to greenhouse gases and, thus, climate change. |
| Economic | The basis for economic vegetarianism is that the consumption of meat is expensive and there are issues of public health and curbing world starvation. |
| Spiritual | Spirituality does not necessarily coincide with being religious. A person can be deeply spiritual without following a religious faith. Spiritual vegetarians feel that eating meat harms them spiritually and damages their soul. |
Use of animal-derived products in medication
The inert substances derived from meat products that are frequently used in medications include gelatin, stearic acid, lactose, shellac, lanolin and beeswax. Of these, gelatin is the most commonly and widely used in pharmaceuticals, although stearic acid comes a close second. Concerns about the use of animal products in medications are not limited to those with particular religious beliefs (Reference Singsit and NaikSingsit 2001; Reference Leung, Davies and WongLeung 2005). Individuals with a stated preference to adhere to vegetarian or vegan diets might also prefer to avoid all such medications.
Gelatin is derived from collagen, a protein found in animal skin and bones. The most common sources of the collagen used in gelatin are pigs and cows. Gelatin is predominantly used in the manufacture of capsules. Hard-shell capsules are produced from gelatin solutions, whereas soft-shell capsules are made from gelatin films. A review of the Physicians’ Desk Reference (www.pdr.net) reveals that 336 listed medications contain gelatin as an inert substrate. Table 3 lists some of the most commonly prescribed psychotropics that contain gelatin.
TABLE 3 Commonly prescribed brand name psychotropic medications that contain gelatin
Clinical implications
Prescribing medication containing animal-derived gelatin and/or stearic acid is sometimes unavoidable. However, people who follow certain belief systems may well be committing a ‘sin’ if they take it. Thus, they face the dilemma of compromising their deeply held religious values or their health (Reference Sattar, Ahmed and MadisonSattar 2004b). As practice shows, some choose the latter course. This has obvious implications not only for patients but also for physicians, who may find themselves facing ethical and even legal challenges. It is therefore imperative that clinicians discuss this matter with patients fully and frankly before any agreement is reached on the use of psychotropic medication. The patient information sheet shown in Fig. 1 might help in initiating such discussion.
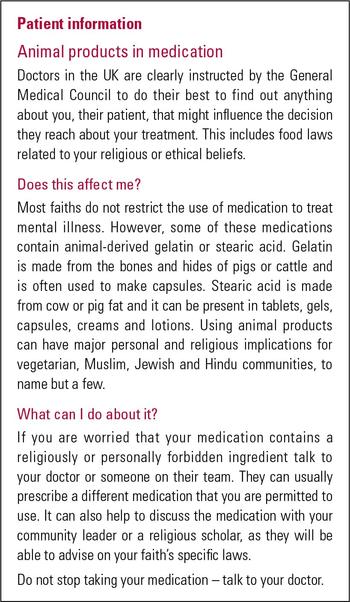
FIG 1 An information sheet for patients concerning animal products in medications.
Psychiatrists should be familiar with religious dietary restrictions (Reference MeyerMeyer 1988) and should make every effort to identify patients with dietary restrictions arising from religious, cultural or personal beliefs (Royal College of Psychiatrists 2004). They should educate patients on the ingredients in their medication and be aware of alternative treatments consistent with patients’ beliefs (Box 2). In many cases an offending medication can be safely avoided.
BOX 2 Approaches to avoid medication containing gelatin or stearic acid
Consider:
-
using liquid or elixir preparations
-
removing the drug from gelatin-containing capsules
-
using non-sustained-release and non-orodispersible forms of the medication
-
exploring both generic and branded forms of the drug, as the gelatin and stearic acid composition may vary
Information on the gelatin or stearic acid content of medications may not be readily available to prescribers and patients. However, it can be obtained directly from the manufacturers or from sources such as the Physicians’ Desk Reference (www.pdr.net) and RxList (www.rxlist.com).
Some medications (modified-release, controlled-release and gastroresistant preparations) already note the presence of gelatin in capsules, but the information is usually confined inconspicuously to the product information leaflet. A logical solution would be to clearly label medications with a single identifiable logo or mark (e.g. a crossed-out ‘V’, reflecting the ‘V’ sign used on vegetarian-approved food products). Such product label guides have now become the accepted and expected norm for many foods.
It can sometimes be helpful to involve community leaders or religious scholars in the decision-making process, not only to aid understanding of these sensitive issues but also to instil a spirit of trust in patients. Theological positions on this matter can be complex, but many faiths follow the overriding principle of medical necessity and exercise leniency to preserve life (Reference Gatrad and SheikhGatrad 2001; Reference SpitzerSpitzer 2003; Reference Gatrad, Mynors and HuntGatrad 2005; Reference UsmaniUsmani 2006).
Conclusions
This article has emphasised the importance for psychiatrists of taking into consideration the patient’s personal and religious beliefs when prescribing psychotropic medication. Some patients choose not to take certain medications, for example those containing gelatin (predominantly found in capsules), as it would be in direct contradiction of their religious practices. Having a basic understanding of a patient’s religious beliefs can improve the doctor–patient relationship and, consequently, adherence to medication.
The interpretation of dietary laws in relation to the consumption of medication containing substances such as gelatin can vary between faiths and depending on a number of factors, including necessity to take the medication, the consequences of not taking it, the availability of alternative preparations and the route of administration (i.e. oral or parenteral). Religious leaders and scholars can be a useful point of contact for patients who have further questions on the subject and discussion can be facilitated through local mental health chaplains.
All psychiatrists should be aware of dietary requirements and food laws relating to psychotropic medication. However, comprehensive policy planning on such an important issue should ideally involve prescribing and non-prescribing healthcare professionals, pharmaceutical industry representatives, religious clerics, community leaders, the Vegetarian Society, the General Medical Council, carers and patients.
MCQs
Select the single best option for each question stem
-
1 A shared understanding of illness between clinicians and patients:
-
a increases relapse rates:
-
b increases mental distress
-
c improves treatment adherence
-
d has a negative impact on healthcare outcomes
-
e has a negative impact on the trust between them.
-
-
2 There are clearly described rules for slaughtering animals in:
-
a Christianity
-
b Hinduism
-
c Buddhism
-
d Judaism
-
e Jainism.
-
-
3 The most common source of animal-derived gelatin used in medication:
-
a cows and goats
-
b cows and pigs
-
c cows and camels
-
d cows and fish
-
e pigs and poultry.
-
-
4 Dietary vegans can consume:
-
a meat
-
b eggs
-
c dairy products
-
d fruits
-
e gelatin.
-
-
5 All of the following approaches can be used to avoid taking medication that contains religiously forbidden ingredients except:
-
a using an elixir preparation of the same medication
-
b using a non-sustained-release form of the same medication
-
c using a generic form of the same medication
-
d involving a community leader or religious scholar
-
e using a non-orodispersible form of the drug.
-
MCQ answers
| 1 | c | 2 | d | 3 | b | 4 | d | 5 | d |










eLetters
No eLetters have been published for this article.