Background
Family carers’ presence and contribution have been widely recognized as a predictor for enabling patients’ end–of–life care at home (Gomes and Higginson, Reference Gomes and Higginson2006). Moreover, family carers’ ability to cope with the role, specifically their ability to manage symptoms, influences the likelihood of death at home (Ullgren et al., Reference Ullgren, Tsitsi, Papastavrou and Charalambous2018), whilst physical and emotional exhaustion from the burden of caregiving acts as a barrier (Wahid et al., Reference Wahid, Sayma, Jamshaid, Kerwat, Oyewole, Saleh, Ahmed, Cox, Perry and Payne2018). It is, therefore, important that healthcare professionals try to meet family carers’ needs by providing timely, tailored support.
Evidence suggests an important component of this support is the provision of information and skills training necessary to undertake physical nursing tasks (Bee et al., Reference Bee, Barnes and Luker2009). This information could increase carers’ mastery and confidence, and carers may find it easier to accept support that enables them to provide care than to accept help for themselves (Grande et al., Reference Grande, Stajduhar, Aoun, Toye, Funk, Addington-Hall, Payne and Todd2009).
The ‘Caring for Someone with Cancer’ booklet is an evidence-based intervention, which was developed to be used by District Nurses to support family carers to care for someone at home towards the end of life by identifying some of the skills required to complete basic nursing tasks. Guided by the Medical Research Council (MRC) framework for developing and evaluating complex interventions, the resource was developed based on existing evidence (Medical Research Council, 2008; Bee et al., Reference Bee, Barnes and Luker2009, Caress et al., Reference Caress, Chalmers and Luker2009) and interviews with current and recently bereaved family carers. Findings from the feasibility study suggest the booklet has the potential to have a positive impact on family carers and may facilitate more people to die at home, by reducing uncertainty and providing reassurance. District Nurses stated they received fewer phone calls from family carers as a result, potentially reducing their workload (Luker et al., Reference Luker, Cooke, Dunn, Lloyd-Williams, Pilling and Todd2015). In addition, further work revealed the booklet has wider utility: using it for other conditions, to support relatives to be involved in the care of residents in nursing homes, and in Healthcare Assistants’ (HCAs) end-of-life care training (Mathieson, Reference Mathieson2018). Important questions remained, however, regarding when and how to deliver the booklet, suggesting more work was required to answer how best to implement the intervention and maximise its usefulness. This was in line with the MRC Framework (2008), and contributed to the current need to translate models of support for family carers into realistic applications for practice (Ferrell and Wittenberg, Reference Ferrell and Wittenberg2017).
The evidence base for effective implementationFootnote 1 of complex interventions remains limited (Medical Research Council, 2008), particularly within home careFootnote 2 nursing (Brooke and Mallion, Reference Brooke and Mallion2016). Implementation studies in this area are challenged by inconsistent terminology, and limited use of theory (Mathieson et al., Reference Mathieson, Grande and Luker2019). Thus, there is a need to assess the extent to which implementation is effective in home care nursing. We, therefore, aimed to implement the booklet intervention in four home care provider sites.
Normalization Process Theory
To address the gap of a limited use of theory in implementation studies in home care, Normalization Process Theory (NPT) guided this study. NPT focuses on the process through which new ways of thinking, interacting, and organising work are embedded, sustained, and ‘normalized’ in practice (May and Finch, Reference May and Finch2009). This theory was considered the most appropriate approach to guide implementation of the intervention after conducting a review of implementation science literature, which evaluated the potential application of 48 different models, theories, and frameworks (Mathieson, Reference Mathieson2018). The reason for using NPT was threefold. First, NPT is compatible with qualitative research and offers specific applications for researchers when designing research, collecting, and analysing data. Second, NPT is useful to explore the barriers and facilitators to embedding the intervention in practice. Third, by using NPT, it is possible to explain the extent to which the new practice has become normalised, thus evaluating the implementation efforts. Furthermore, few studies have tested its use to guide the implementation process (McEvoy et al., Reference Mcevoy, Ballini, Maltoni, O’donnell, Mair and Macfarlane2014). This study, therefore, aimed to test the prospective use of NPT.
NPT has four constructs, each with four corresponding components (Table 1) (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015). This paper reports on data pertaining to the construct ‘Collective Action’, defined as the ‘operational work’ people do to enact new practices (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015). The construct ‘Collective Action’ is therefore useful to understand successful implementation within the study’s context.
Table 1. Summary of Normalization Process Theory’s (NPT) constructs and components

Aims
The study’s aims were to: (1) actively implement the booklet intervention with home care providers using NPT and (2) identify barriers and facilitators for a successful implementation of the booklet intervention, including contextual factors that influence adoption to inform future implementation of evidence-based interventions in this setting.
Methods
Study design
Due to the issues raised in the feasibility study (Luker et al., Reference Luker, Cooke, Dunn, Lloyd-Williams, Pilling and Todd2015), a qualitative approach was adopted to identify ‘task’, ‘social’, and ‘physical’ context levers, which may affect implementation and adoption within the study setting (Johns, Reference Johns2006). Specifically, a qualitative case study was considered a useful technique, as little was known about the phenomenon; multiple perspectives needed to be recognised; and the research needed to be congruent with clinical practice (Walshe et al., Reference Walshe, Caress, Chew-Graham and Todd2004).
We designed a qualitative case study based on Stake’s methodology (Stake, Reference Stake1995). Data for this paper are drawn from semi-structured interviews with key staff, identified as gatekeepers to information, within the case study sites.
Setting
The case was defined as ‘home care settings in one city in the North West of England actively implementing the “Caring for Someone with Cancer’ booklet”. Palliative care is provided by District Nurses in patients’ homes, by Registered General Nurses and HCAs in nursing/residential homes, and by the hospice in-patient and out-patient services (Hospice@Home and Community Specialist Palliative Care Team). Four cases (two nursing homes, a District Nurse team, and a Hospice@Home team) within the case study area were purposefully selected to actively implement, and evaluate the implementation of the intervention (Table 2).
Table 2. Description of case study sites
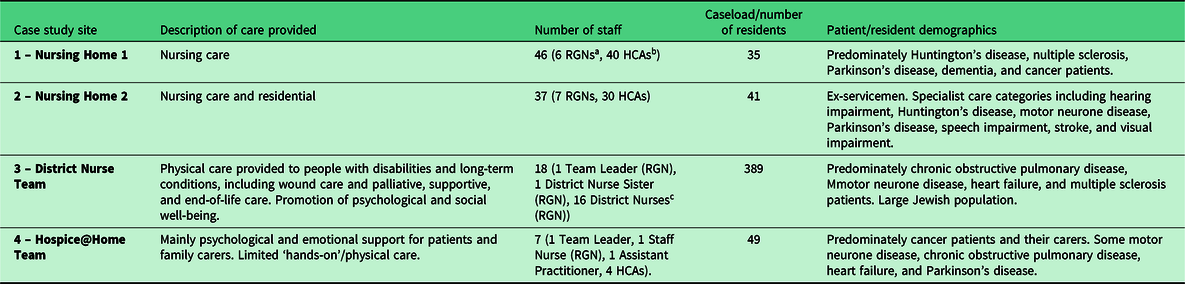
a RGNs or Registered General Nurses are nurses who have completed a 3-year training course in all aspects of nursing care to enable him/her to be registered with the UK Central Council for Nursing, Midwifery, and Health Visiting.
b HCAs or Healthcare Assistants provide care to patients in hospitals or nursing/residential homes (residents’ ‘usual place of residence’) under the direction of a qualified professional. HCAs are sometimes known as nursing assistants, auxiliary nurses, or support workers.
c District Nurses are RGNs with specialist practitioner qualification.
Information sessions, led by the researcher (AM), were used to ‘kick start’ implementation (Wilcox, 2010, Kapp, Reference Kapp2013). Information sessions lasted 30 min and provided details about the booklet’s development, study’s purpose, and expectations of the sites involved. At the sessions, the researcher explained the Internal Facilitator role, which involved becoming a voluntary member of the research team, acting as the intervention’s champion for the site, and attending regular meetings. Internal Facilitators were recruited from all sites.
Data collection
Interviews were conducted by one researcher (AM). Topic guides were tailored to individual case study sites and were informed by NPT (Box 1) (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015). Data, before and after implementation, were collected between May 2016 and June 2017. Most people (n = 35) took part in one interview (pre- or post-implementation). Reasons for this included work commitment, staff rostering, participants leaving the organisation, or site withdrawal from the study.
Box 1. Topic guide questions and example of questions for specific case study sites
General topics covered:
Participants’ background and work experience
The provision of information/support for relatives and participants’ end-of-life care training (Coherence)
Initial impressions of the intervention (Coherence and Cognitive Participation)
Implementation strategies, delivery processes, and implementation work (Collective Action)
Evaluation of the intervention and its implementation (Reflexive Monitoring)
Hospice@Home and District Nurses
Pre-implementation interviews:
Is supporting family carers an important part of your role? Why/why not?
How would you identify which family carers to give the booklet to?
How does the booklet relate to the support you are already giving family carers?
Post-implementation interviews:
How did you work with others to implement the booklet?
Did you have any opportunities to evaluate the usefulness of the booklet?
When might it be difficult to use the booklet? Why?
How do you feel about carrying around copies of the booklets when you visit patients and their carers?
Nursing homes
Pre-implementation interviews:
What end-of-life care training have you received?
What challenges have you faced when putting this training into practice?
How important is it to give relatives help with practical care needs?
How could the booklet help with explaining care and what to expect with relatives?
Post-implementation:
Have recent changes had an impact upon implementation of the booklet? Why/why not??
What is your understanding of the benefits of using the booklet (for staff and relatives)?
Has your understanding of your role in supporting relatives changed? Why/why not?
Sampling and recruitment
All staff members who had access to the booklet, or could provide information about its implementation, were eligible. Internal Facilitators initially contacted potential participants who, with their permission, were introduced to the researcher. All participants had time to consider their involvement, and interviews were arranged at a time convenient to them. Snowball sampling techniques, whereby participants were asked to suggest potential informants, were used once data collection was underway (Coyne, Reference Coyne1997).
Interviews were held in private rooms at the case study sites. Interviews averaged 46 min in length. All interviews were digitally recorded, transcribed verbatim, and anonymised. Written informed consent was obtained from participants prior to each interview. All participants received a ‘Certificate of Participation’ in exchange for their time, which were thought to be an incentive for skilled staff to include in their professional development portfolio and/or contribute to revalidation.
Forty-three females and two males participated, spread across the four case study sites (see Table 3 for a breakdown of roles).
Table 3. Participants interviewed

Data analysis
Framework analysis was used to facilitate within and cross-case analysis (Ritchie and Spencer, Reference Ritchie, Spencer, Bryman and Burgess1994). The researcher (AM) familiarised herself with the data by reading and re-reading transcripts. Recurring ideas were collated into groups of similar concepts and organised into an index (Furber, Reference Furber2010), which was used to inform open coding in NVivo 10, generating a number of thematic ‘sets’ (Spencer et al., Reference Spencer, Ritchie, O’connor, Morrell, Ormston, Ritchie, Lewis, Mcnaughton Nicholls and Ormston2014). The research group (AM, GG, and KL) then met to refine and collapse coding categories, and discuss any discrepancies of interpretation. Summaries of indexed extracts were developed for each thematic set to facilitate within-case analysis. Cross-case analysis was facilitated by examining similarities and differences between the underlying elements identified in the data. Table 4 summaries the analysis process.
Table 4. Summary of analysis process

Findings
Five themes, and corresponding sub-themes, were identified regarding the contextual factors, organisational culture, and implementation capability, which made changing practice within the sites difficult, or conversely more straightforward.
Theme 1: Workforce and predictability of processes
Organisational changes within the NHS in general and specifically within the organisations, in conjunction with demands on staff, possibly due to competitive tender, appeared to result in a number of staff leaving across case study sites. All participants, with the exception of Hospice@Home, discussed the high turnover of staff and current ‘unsettled’ state of the organisation: ‘There’s a lot of disharmony at the moment, because of poor staffing levels and large turnover of staff’ (CHS9 Site 1). This was widely stated as the reason for failed implementation attempts, and was recognised as a potential barrier to other areas of practice development: ‘you don’t want to start a research project with somebody that’s going to leave’ (HaH01 Site 4).
For staff in Nursing Home 1, there was a sense of uncertainty regarding its future, as the current contract for the unit that provided end-of-life care was out for tender. This had an impact on morale, and resulted in some staff seeking other employment, which inhibited implementation and adoption of the booklet. Participants expressed feelings of hopelessness and the futility of developing current practice; changes may not be sustained and the future of the unit was uncertain: ‘I don’t really know how things are going to pan out in the future. It’s like the million dollar question’ (CHS1 Site 1). This suggests there was an absence of ‘change efficacy’; the shared belief in the staff’s collective capability to execute actions involved in implementation (Weiner, Reference Weiner2009). Consequently, some staff did not engage in the work required to embed the new practice.
Within the nursing home settings, staff turnover and use of agency staff – temporary or long-term workers hired from an employment agency – was widely perceived as inevitable, as it was frequently witnessed by participants. This was reflected in one participant’s understanding of her attempts to implement end-of-life care training within nursing homes:
“I: I wonder if you’ve come across any challenges getting this [End-of-Life Care Training] into care homes and actually embedding it?
Absolutely, care home staff move, care home managers move, the commitment from one manager might be less than another manager, staff not being able to be released because they’re short-staffed; and what you need to remember is this is voluntary, they don’t have to take part […] so if that means that they’re leaving the residents vulnerable because there’s not enough staff on the floor then they’re not going to attend your training” – TS01
Similarly, the District Nurse site was undergoing a turbulent period due to staff shortages. The District Nurse team was understaffed for the study’s duration and relied upon agency staff. District Nurse participants discussed the challenges associated with everyday practice, and it was considered an inappropriate time to introduce and integrate something new: ‘I just don’t think at the moment the timing’s right to be introducing new stuff when we’ve got new staff coming through all the time’ (TS02 Site 3). Despite evidence to suggest the booklet intervention could save clinical time (Luker et al., Reference Luker, Cooke, Dunn, Lloyd-Williams, Pilling and Todd2015), and thus facilitate its adoption, participating nurses chose not to use it and rather focused on immediate challenges. The nursing homes and District Nurse team appeared to be ‘in limbo’, waiting for the service to ‘settle down’ before implementing the booklet. This is in contrast to Hospice@Home site, which had a stable workforce, and successfully implemented the booklet: ‘your HCAs, your unqualified staff, tend to stay the same. There tends to be a core of nurses’ (HaH08, site 4).
A stable workforce was thus considered an important facilitator when implementing new practice: ‘otherwise it’s like trying to ice a cake that’s not been baked’ (TS01); with a lack of continuity inhibiting adoption.
Theme 2: Guidance and shared vision
Support from colleagues
The availability of support from other staff members was a key factor in ensuring the successful implementation of the booklet, particularly within the nursing home settings. Specifically, the lack of continuity with nurses in this setting, who were perceived as leading the intervention, and the reliance on agency nurses, resulted in individual adoption, which was haphazard:
“ We’ve had different nurses…when [name of nurses] were here they’d say “I’ve just given such and such that book”…the [nurses] we’re getting now, they’re not here on a regular basis…the one we have on today might not be on for another couple of weeks… so it’s not the same communication” - CHS3, Site 1
When reflecting upon past practice development, many participants discussed the lack of direction from managers and few allocated resources to support staff adjusting to change, resulting in staff feeling ‘abandoned’ and ‘alienated’. Participants claimed they were ‘upset’ and ‘disheartened’ by the absence of manager support, suggesting there was a disconnect between the manager’s perception of the change process and staff’s morale, and that belonging to frontline staff. This often resulted in staff leaving the organisation, which had an impact on subsequent practice development:
“If I was the owner of a factory and suddenly all my senior staff or very experienced carers were upping and leaving, I would have been down on the shop floor saying “what’s going on?”, and that’s what we didn’t get. And it was soul destroying.” – CHS1, Site 1
Communication
Staff’s sense of ‘abandonment’ was exacerbated if the changes were perceived to be ‘sweeping’, or if there was a lack of communication from managers regarding developments. For example, HCAs in nursing home settings usually became aware of changes to practice through ‘word of mouth’: ‘One day when you’re off it just comes, this is a new thing, you have to go and do it’ (CHS204 Site 2). Thus, HCAs appeared to be ‘kept in the dark’ regarding current or future changes. Conversely, nurses were informed of practice developments, which was then cascaded down to HCAs:
“I: When something new is introduced, how are you told about it?
Email or you get told by the nurses. They get the information first and they pass it on to us.” – CHS209, Site 2
New practices were therefore largely adopted and normalised by nurses, whereas HCAs’ adoption was often delayed.
Theme 3: Management of time
Lack of time and large caseloads was a frequently reported barrier to the engagement with the booklet intervention. District Nurses claimed it was difficult to ‘do anything extra’ as they were ‘just getting through the day’; thus, prioritising other tasks over implementation work. However, the time required to deliver the booklet was minimal, suggesting the reported lack of time was instead a consequence of family carers having more information and thus asking nurses more questions. By claiming to ‘be busy’, nurses may restrict patients’ and family carers’ ability to ask for, or access, additional support (Nagington et al., Reference Nagington, Luker and Walshe2013). Furthermore, some nurses were convinced they ‘knew’ so-called ‘tricky’ relatives would ‘tick off’ symptoms in the booklet and apply them to the patient/resident, which could cause upset and generate more work for nurses.
Staff also claimed they required time to become familiar with the intervention, which was considered as an essential preparation work to build accountability and confidence in the new practice (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015). Many District Nurse participants claimed they did not have time to engage in this ‘preparation work’, inhibiting their adoption. Moreover, District Nurses did not have the time to critically reflect upon their practice and identify how the booklet could be integrated. Value, therefore, was not attributed to the booklet, nor was the intervention’s potential to save time realised.
Additionally, as District Nurses anticipated delivering the booklet would add extra time to an already busy visit, and not wanting to overburden staff, the Internal Facilitator did not champion the booklet nor reminded staff to use it. Regardless of initial buy-in from the Internal Facilitator and management endorsement, workload and a perceived lack of time were, therefore, too much of a barrier for many District Nurse participants:
“…I’ll be brutally honest with you, when you’re sitting here in a huddle and you’re saying “this is what I’m doing and I need you all to go out and do this [deliver the booklet]” they’re not thinking about that, they’re thinking about their next visit because they’re busy…” – TS02, Site 3
Similarly, in the nursing homes, participants discussed the chaotic nature of their work, claiming there was ‘never a dull moment’ (CHS1 Site 1) and there was ‘never a break’ (CHS9 Site 1). One participant compared her increasing workload to being on a ‘rollercoaster’, unable to fulfil all her duties within the time available during a shift. Consequently, nursing home staff had to prioritise their workload. Nursing home participants claimed residents care ‘comes first’. Therefore, work related to the resident’s care including new admissions, death of a resident, and communication with relatives was perceived as tasks that required immediate action and were thus prioritised, delaying implementation work.
In addition, scheduled tasks within the nursing home settings took priority. For example, medication rounds consumed the majority of nurses’ time and could be considered a ‘scheduled task’, as they occur at the same time every day. Documentation presents another demand on nurses’ time, which precluded their involvement in implementation and practice development. Documentation makes the invisible visible, which arguably improves communication and continuity of care (Gjevjon and Hellesø, Reference Gjevjon and Hellesø2010), but also places staff under surveillance, possibly accounting for why staff spent time on it. Completing documents could be perceived as ‘maintenance tasks’, which were continuous throughout the day and had an impact on other areas of their practice. Specifically, due to the ‘demands of modern auditing’ (CHS1 Site 1), which was compounded by staff shortages and the use of agency staff, nurses were unable to interact with relatives, which may involve delivering the booklet.
Theme 4: Organisational ethos, leadership, and culture
Successful implementation required the organisation to be conducive to change, whereby sufficient resources to support the change process were allocated. Across the sites, a variety of perspectives were expressed regarding research and changing practice. Some participants emphasised the need to ‘go with the times’, whereas others claimed they preferred ‘old school nursing’ (CHS202), limiting their engagement in practice development. Overall, the hospice, in which the Hospice@Home team was based, was perceived as ‘an open culture for change’, which aimed to ‘develop and share’. Consequently, Hospice@Home staff were given time to participate in the research and were encouraged by the manager. It is likely that Hospice@Home participants had ‘more time’ to engage in implementation work compared to other sites, most notably District Nurses.
Leadership was considered a crucial factor in potential adopters gaining the confidence to use the intervention. For example, in Nursing Home 1, there were persistent claims that implementation ‘fell by the wayside’ because the two Internal Facilitators left, who were perceived as influential local champions. Leadership, including the influence from senior nurses as role models, therefore facilitated the implementation of the booklet intervention.
In contrast, HCAs in the Hospice@Home team had clear leadership and role models in the service co-ordinator and staff nurse. Participants perceived the Hospice@Home Internal Facilitator as the ‘hub’, who engaged in work to keep the intervention visible. In turn, the Clinical Service Manager supported the Hospice@Home Coordinator in her role as Internal Facilitator, describing herself as a ‘leader’ rather than a manager who is ‘more hands on than most people’ (HaH08 Site 4). Participants suggested that the characteristics of a ‘good leader’ includes being knowledgeable of patients, residents, and their families; and taking a ‘hands on’ approach yet giving staff the freedom to organise and develop their practice. Furthermore, constantly communicating with staff, being a ‘port of call’ and approachable were perceived as characteristics of a ‘good leader’. The abovementioned ‘good leader’ was a facilitator in this study.
Theme 5: Staff’s understanding of the innovation and its workability
Applicability
As end-of-life care was the main remit for the Hospice@Home team, the intervention was considered relevant to staff within this site, and thus potential adopters perceived engagement in implementation work to be a legitimate use of their time. The team was, therefore, open to the change process and the booklet was successfully integrated into their routine practice. In contrast, some participants at other sites – where end-of-life care was only a partial remit – considered the innovation to be incompatible with their norms, values, and perceived needs of family carers. These participants resisted adoption and did not deliver the booklet.
Adaptability
The Hospice@Home participants also demonstrated that they worked as a team, and staff felt supported by their colleagues. In contrast to the nursing home sites, there was a sense amongst the Hospice@Home participants that each member positively contributed to the team’s work, and the booklet’s implementation. Specifically, participants discussed the knowledge and expertise within the team, which was accessed when supporting family carers. Consequently, not only was the booklet intervention applicable for staff within this site, but also staff were able to adapt the innovation by providing additional support – with help from colleagues – to meet the needs of their service users; facilitating implementation and encouraging adoption.
HCAs within the nursing home settings claimed they did not feel confident delivering the booklet, as they may disclose prognosis or may be unable to answer relatives’ questions, indicating a ‘Closed Awareness’ (Glaser and Strauss, Reference Glaser and Strauss1965). Conversely, Hospice@Home HCAs felt valued, supported, and were able to use the intervention. It is likely that this respect amongst staff, sharing of expertise, and acknowledgment of individual capabilities, gave Hospice@Home HCAs the confidence to trial and adopt the booklet.
Hospice@Home staff, compared to HCAs within the nursing home settings, were autonomous; not only in the management of their caseload but also within practice development, including the adoption of the booklet. According to one participant, nursing home HCAs required ‘discipline’ (CHS10); indeed, they needed to be ‘told what to do’. This suggests leadership is not only needed to support staff adjusting to change, but is also important in giving potential adopters the authority to change their practice. That is, not the autonomy to introduce changes without approval from the manager, rather directing staff on how to change their practice based on decisions they have made:
“I think… giving out these books, we can’t do that. We need our management to tell us, we can do it” – CHS207
Discussion
In this study, we aimed to better understand the implementation of evidence-based interventions in home care settings by exploring adopters’ experience of implementing the ‘Caring for Someone with Cancer’ booklet in four case study sites. We identified a number of contextual factors, which inhibited or enabled practice development in home care settings, including workforce composition and predictability of processes; management and peer support; time management; and organisational ethos, leadership, and culture.
‘Context’ is widely recognised as a contributing factor to implementation in the theoretical literature (Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009; Weiner, Reference Weiner2009; May et al., Reference May, Johnson and Finch2016), including the well-known distinction between ‘receptive’ and ‘non-receptive’ contexts for change (Pettigrew, Reference Pettigrew1985). Features of organisational context in this study, which dictated the support for the use of the intervention, included communication; leadership; learning culture; and the intervention’s compatibility with, and relevance to, individuals’ work. Implementation was also affected by broader economic and social contexts (‘outer’ context) (Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009), including a national shortage of nurses (NMC, 2017) and HCAs (Skills for Care, 2017), and low morale amongst District Nurses (Drennan, Reference Drennan2019). This may be because people are being discharged ‘quicker and sicker’ from the hospital, which is having a detrimental effect on the workload of District Nurses (Speed and Luker, Reference Speed and Luker2004). Whilst this pattern has existed for over 15 years, it is arguable this is increasing due to the current shortages of hospital beds. Moreover, it is a global fact that the world’s population is increasing and most countries have an ageing population (World Health Organisation, 2015), with many patients living with multiple long-term conditions (Costello, Reference Costello2017). Demographic changes are therefore putting pressure on community-based care providers. This ‘outer’ context may have made otherwise receptive contexts and/or innovating individuals/groups non-receptive. In this study, due to unstable work environments, there was often an absence of ‘change efficacy’ – confidence that collectively staff can implement the change effectively – and ‘change commitment’, which inhibited implementation and adoption (Weiner, Reference Weiner2009). Non-receptive contexts therefore dismiss development, and foster environments in which individuals resist change.
It is widely recognised that ‘context’ is a dynamic process (Bate, Reference Bate and Bamber2014). However, whilst theory has identified context as having an impact upon implementation, ‘timing’ is not explicitly addressed (Nilsen et al., Reference Nilsen, Wallerstedt, Behm and Ahlström2018), nor does the literature on implementation in primary care acknowledge that barriers may change (Lau et al., Reference Lau, Stevenson, Ong, Dziedzic, Treweek, Eldridge, Everitt, Kennedy, Qureshi and Rogers2015). ‘Timing’ was identified as a significant indicator for the success or not of implementation in this study. That is, the setting in which implementation is to take place maybe, or may become, non-conducive to change, which will have an impact upon the receptiveness of individuals’ to engage in practice development (Weiner, Reference Weiner2009). Implementation efforts during periods of ‘bad timing’ may therefore be destined to fail, as it is like ‘trying to ice a cake that hasn’t been baked’. Thus, it is necessary to assess the context, and possibly wait for it to change, or shift the focus of the intervention (May et al., Reference May, Johnson and Finch2016). The work of Diffin et al. (2018) supports this view, and highlights the importance of assessing organisational context when implementing evidence-based intervention and planning for practitioners’ disengagement. A companion paper also highlights the importance of the facilitator role in terms of ‘leverage’ within the team, communication skills and styles, and supporting peers (Diffin et al., Reference Diffin, Ewing, Harvey and Grande2018a). In the current study, staff required support; staff levels needed to improve and new staff had to ‘settle in’; to continue with the metaphor: ‘bake the cake and let it cool before icing’. This finding is consistent with those of Nilsen et al. (Reference Nilsen, Wallerstedt, Behm and Ahlström2018) who found that forward-thinking coordination of change is required to successfully implement change within nursing homes. To assist with this ‘forward-thinking’, heuristics for assessing organisational readiness have been developed (Scaccia et al., Reference Scaccia, Cook, Lamont, Wandersman, Castellow, Katz and Beidas2015; Sharpe et al., Reference Sharpe, Noble, Hiremagular and Grealish2018). Further to these recommendations, practitioners and researchers should consider ‘timing’; whether staff are focusing on other changes, or a high staff turnover, and the relevance of the intervention to potential adopters’ work, which may dictate how much time is given to its implementation.
The NPT constructs ‘Collective Action’ explained why some staff did not adopt the booklet or engage in work required to embed the new practice, as it accounts for the lack of resources invested in the management of the implementation (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015). The concept ‘change fatigue’, defined as a passive resignation towards organisational change and thus a sense of apathy amongst individuals (Nilsen et al., Reference Nilsen, Wallerstedt, Behm and Ahlström2018), may also explain why some nurses chose not to adopt the intervention. Care in the community appeared to be characterised by constant change, and consequently, staff may have had a negative attitude towards changes, including integration of the booklet. This idea is corroborated by Taylor et al. (Reference Taylor, Coates, Brewster, Mountain, Wessels and Hawley2015) who found that new telehealth technologies were perceived to be a ‘fad’ by nurses because of their constantly changing practice, and were not adopted. ‘Change fatigue’ in the current study was signalled by, although may not be synonymous with, the participants’ preoccupation with short-term rather than long-term goals. Therefore, rather than a sense of apathy, being ‘tired’ of constantly changing their practice may lead to practitioners’ resisting further changes.
It has been recognised for over 15 years that management support is particularly important to the success of change processes, as managers often dictate how resources in an organisation are used (Bryar and Bannigan, Reference Bryar, Bannigan, Bryar and Griffiths2003). Recent research has shown this continues to be a significant factor in the implementation of evidence-based practice in home care (Johnston et al., Reference Johnston, Coole, Narayanasamy, Feakes, Whitworth, Tyrell and Hardy2016), which was confirmed in this study. All staff should be involved in the change process from the outset. Specifically, HCAs are the main workforce and need to be harnessed and involved in the mainstreaming of interventions in this setting. To encourage HCAs’ participation in practice development, this staff group requires a ‘good leader’; practical know-how should be shared, and the contribution of individual staff members recognised. Moreover, as this study, and Nilsen’s et al. (2018) research has shown, leadership in the form of registered nurses as role models, can facilitate HCAs’ learning regarding the principles of palliative care and the development of knowledge and/or practice.
Competing workload was a frequently reported barrier in this study. One solution may be to offer staff dedicated time, away from clinical duties, to engage in practice development. This could reduce distractions (‘tasks that required immediate action’; ‘scheduled tasks’; and ‘maintenance tasks’) and encourage engagement. However, research suggests that setting time aside alone is not adequate (Mallion and Brooke, Reference Mallion and Brooke2016; Renolen et al., Reference Renolen, Høye, Hjälmhult, Danbolt and Kirkevold2018). Rather, our findings suggest staff actually require time to critically reflect upon their current practice. This could occur in groups (‘Communal Appraisal’), or individually (‘Individual Appraisal’) (May et al., Reference May, Rapley, Mair, Treweek, Murray, Ballini, Macfarlane, Girling and Finch2015), but may only be possible if staff levels improve.
Strengths and limitations of the study
Qualitative case study provided an ideal methodology, allowing the holistic exploration of interactions and contextual features of implementation. Nonetheless, our study’s conclusions were made from contact with a limited number of participants. The follow-up period (post-implementation) was also relatively limited (6–12 months). Furthermore, only 10 participants across the four sites took part in both stages: pre- and post-implementation interviews. A future study could explore the sustainability of the booklet intervention, and further test the facilitators identified in this study, to encourage the uptake of other evidence-based interventions in home care settings.
Notwithstanding the study’s limits, the findings make an important contribution to implementation literature, both within the area of home and end-of-life care as: (a) it is one of the first to use NPT to drive the implementation process, (b) provides an in-depth exploration of implementation, solely utilising qualitative methods, and (c) provides evidence that, despite the booklet being originally developed to be used as an adjunct to district nursing, it could be used within nursing home settings, both to support relatives and educate staff members. Furthermore, by exploring the delivery – or not – of the booklet, this study provided further justification for use of the intervention in palliative home care for cancer patients, and revealed with a ‘few tweaks’ the booklet would be suitable for any life-limiting conditions. Specifically, participants that attributed worth to the intervention acknowledged there was a gap in service provision and family carers require more support to fulfil patients’ preferences to be cared for and die at home. The booklet was considered a means to pass on some of the knowledge required to fulfil this; specifically, on ‘what to expect’ when the patient approaches the end of life. The intervention was received positively by family carers across all sites, which encouraged many members of staff to use it.
Conclusion
This study reveals unique challenges experienced by home care providers and researchers when attempting to change practice within this setting, including turbulent change and a focus on short-term rather than long-term goals. At the time of this study, care in the community appeared to be in crisis, as a result of underfunding and high staff turnover (Drennan, Reference Drennan2019). Participating sites were therefore not ‘ready’ for the change process and were widely under-resourced, highlighting the importance of timing when introducing change. It is likely that the challenges experienced by the researcher will be faced by others for the foreseeable future. Our findings suggest management leadership, staff involvement from the outset, and dedicated time to critically reflect upon existing and new practices may encourage future engagement with, and adoption of, evidence-based interventions in home care settings.
Acknowledgements
The authors would like to acknowledge the support of the Internal Facilitators and the four case study sites, and thank the staff involved in the interviews.
Financial support
This research was funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) Greater Manchester. The NIHR CLAHRC Greater Manchester is a partnership between providers and commissioners from the NHS, industry and the third sector, as well as clinical and research staff from the University of Manchester. The views expressed in this article are those of the author(s) and not necessarily those of the NHS, NIHR, or the Department of Health and Social Care.
Conflicts of interest
None.
Ethics
Ethical approval for this study was granted by Yorkshire & The Humber – South Yorkshire Research Ethics Committee (Ref: 16/YH/0202). Health Research Authority (HRA) approval was obtained from the participating NHS Trust, as well as from the individual case study sites. We received written informed consent for the interviews and for recording of the interviews.









