Clinician's Capsule
What is known about the topic?
The 5-meter gait speed test is an objective and efficient test to screen for frailty at the time of ED discharge.
What did this study ask?
Is slow gait speed or weak handgrip strength associated with repeat ED visits and functional decline?
What did this study find?
Two of five older adults leaving the ED were found to have slow 5-meter gait speed using a cutoff of 6 seconds or more, which was associated with higher risks of functional decline and subsequent ED visits.
Why does this study matter to clinicians?
Adverse events could potentially be mitigated by referring slow walkers for further geriatric assessment and interventions.
INTRODUCTION
Frailty is a geriatric syndrome characterized by impaired resilience to stressors and adverse health outcomes.Reference Clegg, Young, Iliffe, Rikkert and Rockwood1 The emergency department (ED) is the receiving ground for patients suffering acute stressors, and despite effective stabilization and discharge, frail patients often do not regain their baseline functional status and they return to the ED for new or unresolved issues. With older adults being the most rapidly growing group of patients encountered in the ED,Reference Pines, Mullins, Cooper, Feng and Roth2–Reference Lowthian, Curtis, Stoelwinder, McNeil and Cameron4 and the most likely to be frequent attenders,Reference Street, Berry and Considine5 there is an opportunity to screen for frailty and initiate interventions that may mitigate adverse outcomes. These interventions may include pathways for rapid follow-up by primary care providers, referral to outpatient geriatric assessment units, and community-based support services.
While frailty has been integrated in various medical and surgical specialties, adoption has been limited in emergency medicine.Reference Theou, Campbell, Malone and Rockwood6 A systematic mapping review on this topic found that there was a promising body of evidence on the treatment of frail patients in the ED, encompassing changes to ED staffing, physical infrastructure, care delivery, and holistic “geri-ED” models of care.Reference Preston, Chambers, Campbell, Cantrell, Turner and Goyder7 However, the review found that there was inconclusive evidence to endorse the use of any specific tool to identify frail patients in the ED, with most studies using rapid case finding questionnaires, checklists of accumulated deficits, or patient-reported assessments of the frailty phenotype. The latter is typically operationalized as a combination of slow gait speed, weak handgrip strength, low habitual physical activity, exhaustion, and weight loss.Reference Fried, Tangen and Walston8
Rather than asking patients to describe their walking and strength abilities as previously done, we sought to improve the identification of frailty by objectively measuring central components of the frailty phenotype,Reference Afilalo9 namely, gait speed and grip strength, at the time of ED discharge. Both of these tests have been extensively validated in older adults, and gait speed has been shown to be the screening test with the highest combined sensitivity and specificity to identify frailty in the community.Reference Clegg, Rogers and Young10 However, little is known about the use of gait speed to identify frailty in the ED. The current study was conducted to address this knowledge gap and test the hypothesis that simple objective physical performance tests would be associated with functional decline and repeat visits following ED discharge.
METHODS
Study design and population
This report is a prospective cohort study conducted between 2014 and 2016 at the Jewish General Hospital ED in Montreal, Quebec. Patients 75 years or older were approached by trained research professionals before ED discharge and invited to complete a questionnaire, grip strength test, and 5-meter gait speed testReference Afilalo, Alexander and Mack11 (Supplemental Table 1, which is available online) to assess their level of frailty and disability. Caregivers and family members were encouraged to be present to contribute their input about the patients’ baseline functional status and living situation. After ED discharge, patients were contacted to reassess their level of disability and re-visits to the ED. Electronic medical records were reviewed by to extract clinical covariates. Institutional ethics approval was obtained, and participants provided informed consent. Excluded were those with prohibitive language barriers, severe neuropsychiatric impairments (severe dementia, active delirium, unstable psychiatric condition), acute lower limb injuries that impeded walking, and arrival from full-care assisted living or rehabilitation facilities. Eligible patients were approached during daytime hours on weekdays, representing a convenience sample within the constraints of our research assistants’ availability. The treating physicians and patients were blinded to the frailty test results so as not to influence their decision to proceed with the planned discharge from the ED or alter the postdischarge plan.
Outcome measures
The outcomes of interest were unplanned repeat ED visit and postdischarge functional decline. Repeat ED visits were ascertained at 1 and 6 months using a combination of telephone contact with the patients and their family members and a review of the electronic medical records at the Jewish General Hospital. Unplanned visits excluded those that were scheduled or requested by the clinician for specific testing. Functional decline was ascertained using a 13-item disability questionnaire consisting of six basic activities of daily living (ADL; Katz Index)Reference Katz, Ford, Moskowitz, Jackson and Jaffe12 and seven instrumental activities of daily living (IADL; Older Americans Resources and Services scale)Reference Fillenbaum and Smyer13 administered at baseline and by telephone interview 1 month after ED discharge. The number of ADL and IADL items for which help was required (partial or total dependency) was summed to calculate the disability score, ranging from 0 to 13 points. Whereas different scoring schemes for disability have been proposed, this simplified scheme is commonly used and has acceptable psychometric properties.Reference Suijker, van Rijn, Riet Ter, Moll van Charante, de Rooij and Buurman14 An increase of one or more points from baseline to follow-up was defined ad hoc as a clinically meaningful functional decline.Reference Suijker, van Rijn, Riet Ter, Moll van Charante, de Rooij and Buurman14 The research assistants administering the follow-up questionnaire were blinded to the baseline frailty test results.
Statistical analysis
The distributions of gait speed and grip strength were examined using histograms and summary statistics. Unadjusted associations were evaluated using chi-squared and student t-tests. Adjusted associations were evaluated using logistic regression models. To avoid overfitting, parsimonious models were a priori adjusted for age, female sex, white race, Functional Comorbidity Index (FCI),Reference Groll, To, Bombardier and Wright15 ambulance arrival, final diagnosis, and either gait speed or grip strength. Final diagnosis was categorized as cardiovascular, gastrointestinal or genitourinary, infectious, musculoskeletal, or other. The FCI is a composite score encompassing the following 17 comorbidities: angina, myocardial infarction, heart failure, stroke, peripheral arterial disease, diabetes, asthma, chronic obstructive pulmonary disease, gastrointestinal bleed, back disease, arthritis, osteoporosis, depression, anxiety, visual impairment, hearing impairment. Obesity was not included because body mass index was not systematically collected. This study was powered with an alpha of 0.05 and beta of 0.80 to detect a twofold increase in repeat ED visits in frail patients, assuming a baseline rate of 20% and an even proportion of frail and nonfrail patients. Analyses were performed with the STATA 14 software package (College Station, TX).
RESULTS
Study cohort
During the study period, 157 patients were enrolled and 7 (4%) of these were lost to follow-up, leaving 150 patients for analysis in the final cohort (Figure 1). The characteristics of patients who were eligible but nonenrolled were similar to patients who were enrolled (Supplemental Table 2). The mean age was 81.1±4.9 years with 76 (51%) females. All patients were able to complete the gait speed and grip strength tests before ED discharge, and there were no testing-related adverse events. The mean grip strength was 28.8±8.9 kg (Supplemental Figure 1), with 34 (23%) being classified as weak. The mean gait speed was 0.93±0.29 meters/second (Supplemental Figure 2), with 61 (41%) being classified as slow (<0.83 meters/second). On aggregate, 71 (47%) had evidence of frailty based on either slow gait speed and/or weak grip strength (<30 kg for men and <20 kg for women).

Figure 1. Flow diagram.
Baseline characteristics
Patients that were frail according to either gait speed or grip strength were older (83.5 v. 79.1 years; p < 0.001), with a poorer self-reported health rating (2.4 v. 2.0 of 5; p = 0.002), a greater number of ADL/IADL disabilities (1.0 v. 0.2 of 13; p < 0.001), a greater number of FCI comorbidities (3.0 v. 1.9 of 17; p < 0.001) (Table 1). The individual comorbidities most frequently observed in frail patients were heart failure, hypertension, arrhythmia, and arthritis. The individual dependencies most frequently reported by frail patients were requiring help for transportation, shopping, housework, and incontinence (Supplemental Figure 3). Despite these differences, frail patients were not significantly more likely to receive home help services at baseline and had similar modes of ED arrival, triage acuity, length of stay, and final diagnoses.
Table 1. Baseline characteristics

ED = emergency department; GI = gastrointestinal; GU = genitourinary; MSK = musculoskeletal. Continuous variables expressed as mean ± standard deviation, categorical variables expressed as number of patients (proportion) for the “yes” response. Self-rated heath status scored from 1 (very good) to 5 (very poor). Functional Comorbidity Index scored from 0 (no comorbidities) to 17 (most comorbidities) based on a predefined list of comorbid conditions.
Unadjusted outcomes
A total of 29 (19%) and 45 (30%) patients had documented unplanned repeat ED visits at 1 and 6 months, respectively, and 36 (25%) had evidence of functional decline at 1 month (Table 2). Repeat ED visits were not significantly associated with gait speed or grip strength in unadjusted analyses, whereas functional decline was significantly associated with being frail (35% v. 14%; p = 0.002). Frail patients had a greater number of ADL/IADL disabilities at 1 month (1.4 v. 0.3; p < 0.001) and a trend toward a greater change in number of disabilities from baseline to 1 month (+0.5 v. +0.1; p = 0.07). In turn, there was a trend for functional decline at 1 month to be a risk factor for repeat ED visits at 6 months (43% v. 26%; p = 0.06).
Table 2. Unadjusted outcome measures

ED = emergency department. Continuous variables expressed as mean ± standard deviation, categorical variables expressed as number of patients (proportion) for the “yes” response. Disability scored from 0 (no disabilities) to 13 (most disabilities) based on the number of ADLs and IADLs that the patient reported being unable to perform without help.
Adjusted outcomes
After adjusting for age, sex, race, FCI, ambulance arrival, and final diagnosis, gait speed was independently associated with repeat ED visit at 6 months (odds ratio [OR] 1.20 per 0.1 meters/second decrement, 95% confidence interval [CI], 1.01 to 1.42) and functional decline at 1 month (OR 1.39 per 0.1 meters/second decrement, 95% CI, 1.12 to 1.72) but not with repeat ED visits at 1 month (OR 1.06 per 0.1 meters/second decrement, 95% CI, 0.88 to 1.27) (Table 3; Figure 2). The Hosmer-Lemeshow goodness-of-fit p-values for these models were 0.18, 0.18, and 0.21, respectively. When dichotomized according to the 6-second cutoff (0.83 meters/second), slow gait speed was independently associated with functional decline at 1 month (OR 3.52; 95% CI, 1.39 to 8.89). In a sensitivity analysis, functional decline at 1 month added to the multivariable model was associated with repeat ED visits at 6 months (OR 2.60; 95% CI, 1.01, 6.69). Grip strength was not significantly associated with any of these outcomes (Table 4).

Figure 2. Adjusted association between gait speed and incident functional decline. Slower gait speeds were associated with higher probabilities of functional decline. Functional decline was defined as one or more new disabilities for basic or instrumental activities of daily living 1-month after ED discharge.
Table 3. Gait speed adjusted models

CI = confidence interval; ED = emergency department; FCI = functional comorbidity index; GI = gastrointestinal; GU = genitourinary; MSK = musculoskeletal; m/s = meters/second; OR = odds ratio.
Table 4. Grip strength adjusted models
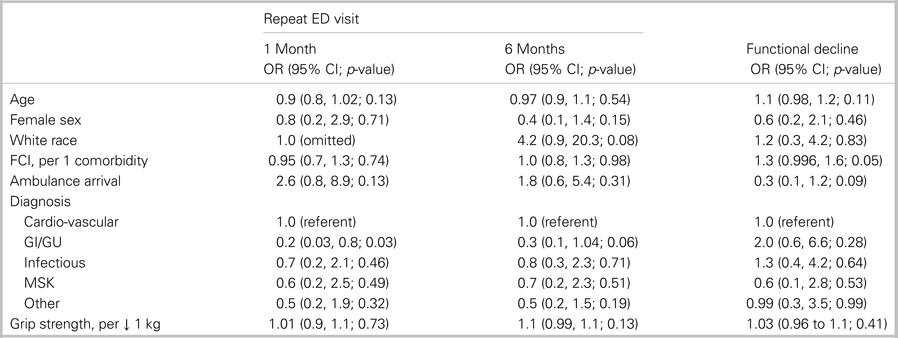
CI = confidence interval; ED = emergency department; FCI = functional comorbidity index; GI = gastrointestinal; GU = genitourinary; kg = kilograms; MSK = musculoskeletal; OR = odds ratio.
DISCUSSION
Our study has demonstrated that 5-meter gait speed can be feasibly measured at the time of ED discharge to identify frail older adults at risk for functional decline and return to the ED. Two of five older adults leaving the ED were found to be slow walkers, which, compounded on their greater burden of comorbidity and functional disability, increased by threefold their risk of short-term further functional decline. Functional decline was a harbinger for future ED usage over the ensuing 6 months. Gait speed was not predictive of short-term repeat ED visits within the first month after ED discharge. Finally, grip strength was not predictive of functional decline or repeat ED visits; therefore, gait speed should be favored as a screening test for frailty in this setting.
To date, most of the evidence on frailty in the ED has been based on rapid geriatric case finding questionnaires (Identification of Seniors At Risk [ISAR], Triage Risk Screening Tool [TRST], PRISMA-7, Silver Code) and global assessments of accumulated deficits (Frailty Index [FI], Clinical Frailty Scale [CFS], Brief Geriatric Assessment [BGA]).Reference Theou, Campbell, Malone and Rockwood6,Reference Preston, Chambers, Campbell, Cantrell, Turner and Goyder7,Reference Launay, de Decker, Kabeshova, Annweiler and Beauchet16,Reference Beauchet, Fung and Launay17 The case finding questionnaires are practical for front-line screening at the time of ED triage,Reference Bullard, Melady and Emond18 but their specificity to predict adverse outcomes is modest. The FI and CFS are validated predictors of hospital admission, length of stay, death, and functional decline,Reference Hastings, Purser, Johnson, Sloane and Whitson19–Reference Brousseau, Dent and Hubbard23 but their practical utility is contingent on being able to collect the required data elements in real-time.Reference Searle, Mitnitski, Gahbauer, Gill and Rockwood24 The busy ED clinician can “ballpark” a CFS rating, but this type of rating is poorly reproducibleReference Bouillon, Kivimäki and Hamer25 and no better than subjective judgment.Reference Sirois, Griffith and Perry26
Phenotypic assessments of frailty, particularly those based on physical tests, are objective and generalizable across clinicians and institutions.Reference Afilalo9 This is pertinent in the ED where clinicians have limited time for questionnaires, acutely ill patients may have limited ability for recall, and over time, a given patient may visit multiple different EDs and be seen by a variety of clinicians. However, acutely ill patients may have limited ability to complete physical tests and the resulting scores may not be indicative of their true capabilities. Fallon et al. cited this concern to justify why their prospective cohort study failed to observe an association between frailty and mortality in ED patients, with frailty having been measured by a questionnaire and grip strength test.Reference Fallon, Kilbane and Briggs27 Tucker et al. sought to pilot test the feasibility of the gait speed test by ED nurses, and although the nurses agreed that “gait speed screening should be implemented in the ED as a standard of care for older patients,” they managed to collect these data in only 21/35 patients.Reference Tucker, Evans, Clevenger, Ardisson and Hwang28
Sirois et al. attempted to circumvent the ED patients’ acute physical limitations by asking them to self-rate their lower-extremity strength, energy, and weight loss,Reference Sirois, Griffith and Perry26 finding this to be predictive of functional decline 3–6 months after an ED visit for a minor injury. Martin-Sanchez et al. similarly asked patients to self-rate their gait speed, upper-extremity strength, activity, energy, and weight loss, finding this to be predictive of 30-day mortality after an ED visit for decompensated heart failure.Reference Martín-Sánchez, Rodríguez-Adrada and Mueller29 Despite these two promising studies, Stiffler et al. reported the accuracy of self-rated gait speed and grip strength to be weak in ED patients and concluded that objective measurements should be favored.Reference Stiffler, Finley, Midha and Wilber30 A systematic review by Eagles et al. did not identify any high-quality studies using gait speed as a quantitative assessment in the ED; moreover, nonquantitative assessments of mobility (mainly the “Get Up & Go” test) were not predictive of hospital admissions or ED visits.Reference Eagles, Yadav, Perry, Sirois and Emond31 Thus, the current study was designed to objectively measure gait speed in the ED and demonstrate its feasibility and prognostic value.
Several limitations merit discussion. First, this was a single-center study that should be confirmed by a larger multi-center study before recommending gait speed for widespread use. It should be noted that gait speed has been validated in acute care settings outside of the ED, including medical wards and cardiovascular units.Reference Peel, Kuys and Klein32 While gait speed has been shown to outperform more elaborate frailty scales to predict adverse outcomes,Reference Purser, Kuchibhatla, Fillenbaum, Harding, Peterson and Alexander33,Reference Afilalo, Mottillo and Eisenberg34 it remains a screening test, and broader assessments are required to capture the multiple facets of frailty. Second, this study used research assistants to measure gait speed during working hours and did not test the implementation by clinical staff during all hours. Although this may affect the generalizability of our results, it is unlikely to have introduced a selection bias because enrolled and nonenrolled patients were generally similar and the reasons for not approaching patients were often logistical in nature. Third, ED visits were ascertained by reviewing medical records at the study center and interviewing patients by phone, such that a minority of ED visits occurring at other centers and not recalled by patients may have been missed leading to a nondifferential information bias. Fourth, the number of covariates analyzed in relation to the number of events for repeat ED visits (mainly at 1 month) may have led to residual confounding or overfitting.Reference Vittinghoff and McCulloch35 Lastly, the downstream effect of testing for frailty was not assessed and will require dedicated intervention studies. A systematic review identified 18 intervention studies focused on comprehensive geriatric assessment and delivery of care during the ED stay, although few studies addressed the optimization of care after the ED discharge.Reference Preston, Chambers, Campbell, Cantrell, Turner and Goyder7
CONCLUSIONS
Five-meter gait speed is an objective low-cost test to screen for frailty before ED discharge. Slow walkers have an increased risk of functional decline and subsequent ED visits within 6 months. These adverse events could potentially be mitigated by referring slow walkers for further geriatric assessment and interventions to improve their functional status and provide them with the necessary support services at home. While interventions for frail older adults have been successfully deployed in the fields of primary care and rehabilitation medicine,Reference Bibas, Levi, Bendayan, Mullie, Forman and Afilalo36 it remains to be determined how to best connect frail ED patients with the community-based resources that they require to reduce their risk of functional decline and frequent ED visits.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.431.
Presentations
This work was presented at Canadian Association of Emergency Physicians (CAEP) annual conference in 2015, Edmonton, Alberta.
Financial support
This work was supported in part by the Jewish General Hospital Foundation. Dr. Jonathan Afilalo is supported by grants from the Fonds de recherche du Québec en Santé and Canadian Institutes of Health Research.
Competing interests
The authors (J.A., S.M., XX., A.C., J.A.M., J.S.D., M.A.) declare that there is no conflict of interest.










