Cardiac cephalgia is a rare form of headache occurring as a manifestation of myocardial ischemia and aggravated by exercise. The International Classification of Headache Disorders (ICHD-3) classifies it as a secondary headache in the category attributed to disorders of homeostasis. 1 Mechanisms hypothesized for the pathophysiology of cardiac cephalgia include: (1) convergence of spinal cord nerve fibers with those nerves from the heart, (2) reduction of venous return from the brain to the heart resulting in increased intracranial pressure, or (3) increased inflammatory markers leading to vasodilation.Reference Torres-Yaghi, Salerian and Dougherty 2 Owing to the relationship with cardiac ischemia, correctly diagnosing this condition is imperative. Failure to recognize it can result in serious negative consequences. Misdiagnosis of cardiac cephalgia with a more common headache condition such as migraine can lead to treatment with abortive medications such as triptans. Triptans are contraindicated in patients with ischemic heart disease because of their vasoconstrictive properties which may exacerbate the underlying pathology of ischemia.Reference Nilsson, Longmore and Shaw 3 Rather, headache because of cardiac cephalgia is relieved by treatment with nitroglycerine and its derivatives. We present a case to expand on the classical description of cardiac cephalgia, highlight the importance of recognizing this condition, and detail its workup and management.
Mr. S, an 86-year-old man, presented to hospital with recurrent headaches and chest pain of 6 weeks. His past medical history is significant for polycythemia rubra vera managed with hydroxyurea, intermittent vertigo since the age of 10 managed with beta-histine, fusion of C4-6 vertebrae for degenerative disc disease, renal stones, benign prostatic hypertrophy, and a left total knee replacement for osteoarthritis for which he was using daily aspirin.
Mr. S was admitted to cardiology department. His headaches would occur 1-3 times daily lasting 30-90 minutes. They would start as a dull pain but quickly increase in intensity. The headaches would occur at rest; and were located bilaterally, posteriorly, and radiate anteriorly or holocranially. These headaches could be severe, often reducing the patient to tears. Associated with every headache, Mr. S would experience chest heaviness and dyspnea. He denied any prior headache history. The headaches had no provoking factors, no photophobia/phonophobia, no nausea, no autonomic features, no diurnal variation, and no associated changes with activity or posture. Mr. S had unremarkable cardiac and neurological examinations. His vital signs were stable and within normal limits. Initial laboratory investigations including complete blood count, electrolytes, and troponins were normal. ECG demonstrated normal sinus rhythm, chest X-ray showed no intrathoracic pathology, and CT head revealed no evidence of intracranial pathology.
As part of the cardiac workup, an exercise thallium test was performed, whereby the patient exercised for 4 minutes 10 seconds, and demonstrated 2 mm upsloping ST depression infero-laterally with exertional angina. Myocardial perfusion imaging revealed a moderate volume of ischemia in the right coronary artery (RCA) territory. Coronary angiography (Figure 1) revealed a 90% distal posterior circulation stenosis that was felt to be too small for stenting, and non-flow limiting disease elsewhere (60% proximal left circumflex, 50% diagonal, and 80% diagonal branch). Mr. S had an MRI brain and C-spine which demonstrated diffuse smooth dural thickening with enhancement in the brain (Figure 2) prompting a lumbar puncture. This was unremarkable (no opening pressure was performed by interventional radiology under fluoroscopy). CT chest/abdomen/pelvis was negative for sarcoid or a primary neoplasm, but revealed a partially occlusive thrombus of the inferior mesenteric vein. The dural enhancement shown on MRI was felt to be due to extramedullary hematopoiesis, which has been reported to occur in polycythemia.Reference Ito, Fujita and Hosogane 4 Detailed investigations including immunoglobulin G (IgG) subclasses and clinical follow-up have not shown evidence of other causes for the MRI findings. Per hematology, Mr. S was started on lifelong anticoagulation (Warfarin) in hospital given the inferior mesenteric vein thrombus.
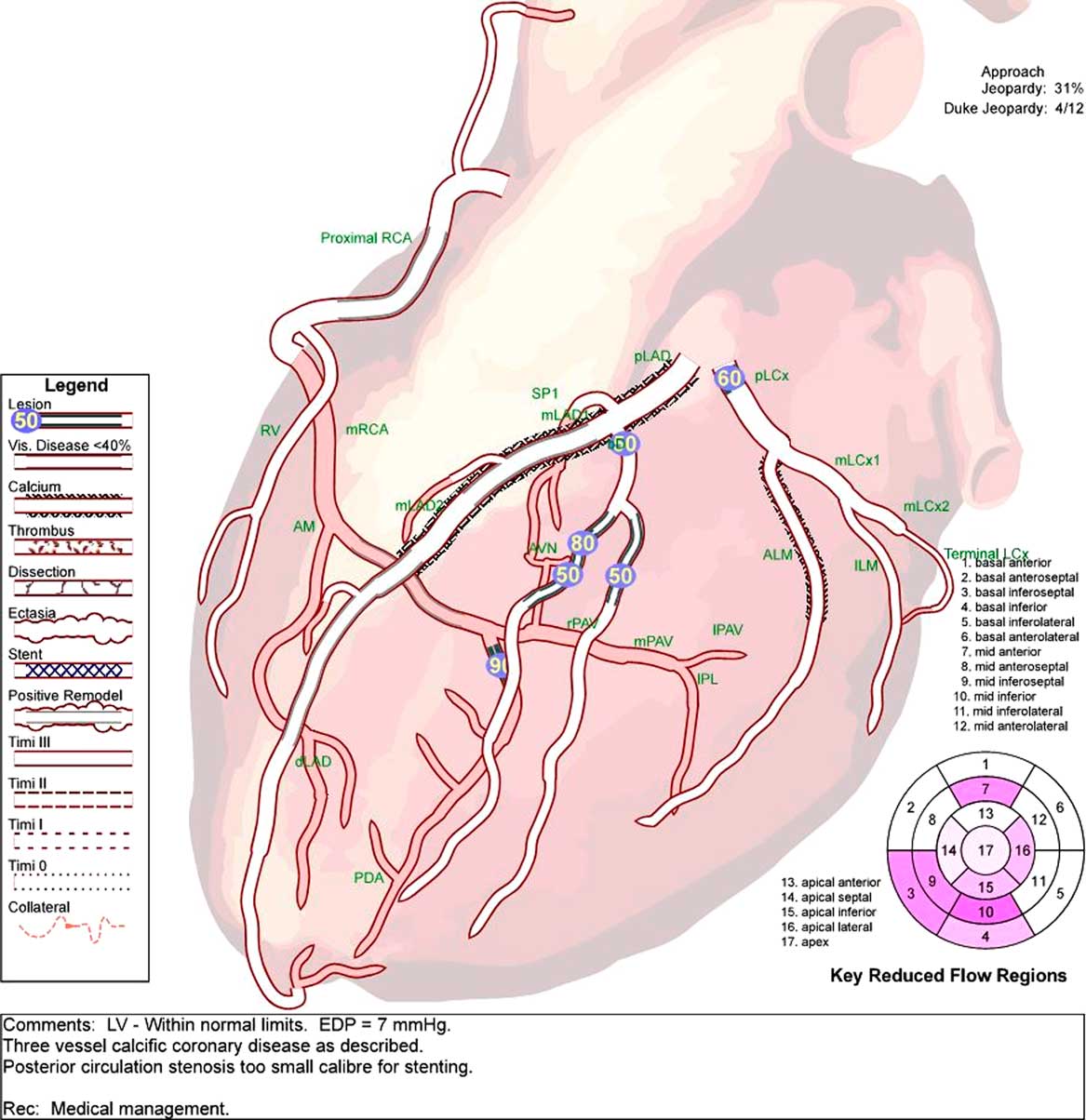
Figure 1 Cardiac angiogram demonstrating multivessel calcific coronary disease, most prominently 90% stenosis in the posterior circulation that was too small for stenting. Medical management advised.
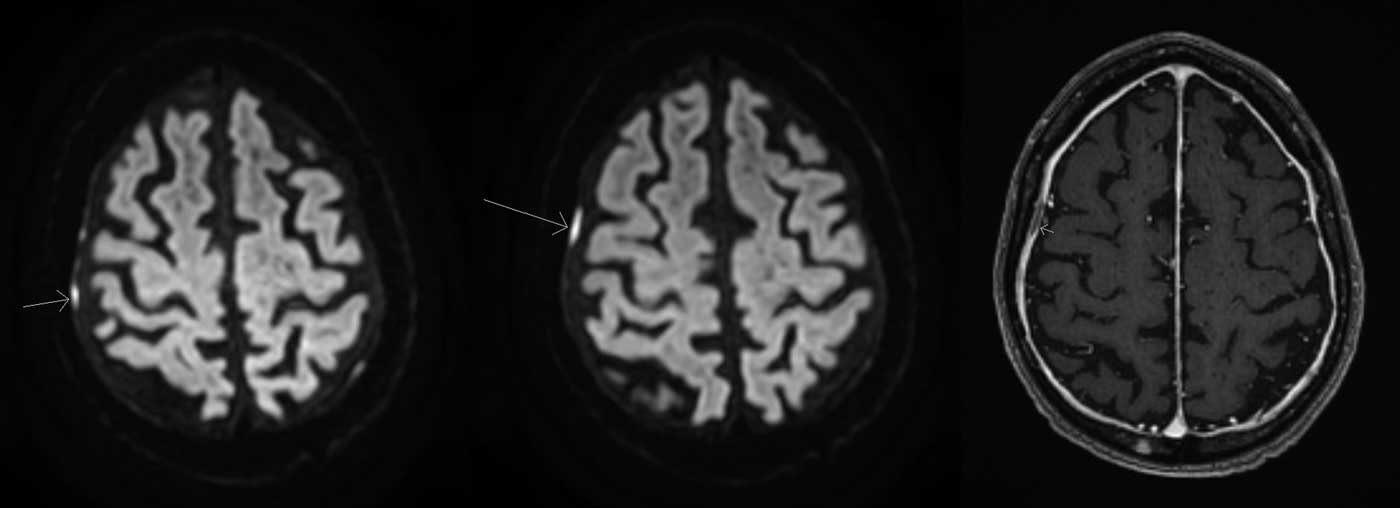
Figure 2 MRI brain sequences demonstrating smooth dural thickening with enhancement. Left and middle: Diffusion weighted imaging sequences demonstrating tiny foci of dura-based diffusion restriction overlying the right convexity. Right: T1-weighted sequence with gadolinium demonstrating smooth diffuse dural-based enhancement.
This presentation of headaches and associated chest pain seems most consistent with cardiac cephalgia. As the patient had headache with concurrent symptoms of known cardiac ischemia, the overall recommendation was for optimization of anti-ischemic therapy. He was initiated on amlodipine, bisoprolol, a nitroglycerin (NTG) patch (gradually titrated up in hospital with good effect), and NTG spray as required. Mr. S continued to have episodes (1-2 episodes/24 hours) of dull chest discomfort with associated headache, relieved with NTG spray. He continued to use NTG spray for breakthrough episodes of chest pain and headache upon discharge. Upon follow-up by neurology 1 month post-discharge, he was found to have significantly decreased headache frequency, approximately 1 per week.
We present a case of cardiac cephalgia in a patient who presented with simultaneous symptoms of headache, chest heaviness, and dyspnea. Similar cases of myocardial ischemia associated with headache have been previously reported, and the label “cardiac cephalgia” was first described in 1997.Reference Lipton, Lowenkopf and Bajwa 5 Our patient had concurrent cardiac symptoms and headache in the context of ischemic heart disease. Consequently, these headaches improved with medical management of ischemia. The temporal relation of headache, myocardial ischemia and its management, as well as the characteristics of the headache are in keeping with the ICHD-3 diagnostic criteria for cardiac cephalgia. 1
The difficulty in diagnosing cardiac cephalgia is demonstrated in our case. There were many challenging factors, such as a previous diagnosis of polycythemia, missing cerebral spinal fluid (CSF) opening pressure, symptoms occurring outside of activity, and consideration of primary headache disorders. Polycythemia can cause headache, 1 but this was a longstanding diagnosis that was well managed in our patient. Unfortunately, a CSF opening pressure was not obtained; however, there was no orthostatic component to our patient’s headache nor associated features to suggest a low-pressure headache. As in ischemic heart disease, it is not implausible that cardiac cephalgia could occur without exertion. Finally, primary headache disorders could be considered in this case; however, our patient had several red flags, which were described in the history, to deter us from these disorders. Most notably, our patient was an 86-year-old with new onset headache without prior headache history.
Given the severity of associated coronary pathology, diagnosis of cardiac cephalgia is critical. With good follow-up, headache journaling, and patient compliance to treatment goals, preservation of cardiac myocytes and prevention of ischemia can be achieved.
ACKNOWLEDGEMENT
Patient consent was obtained for publication of the manuscript. We thank the patient for graciously allowing us to present his case for this journal so that we can educate our neurologists of the future.
DISCLOSURES
Ryan MacIsaac, Scott Jarvis, and Kevin Busche have nothing to disclose.
STATEMENT OF AUTHORSHIP
Ryan MacIsaac contributed to drafting the manuscript and clinical information on the case. Kevin Busche and Scott Jarvis contributed to critical revision of the manuscript and clinical information on the case.




