1. Introduction
The major public health problem and personal tragedy of suicide is accompanied by a lack of empirical evidence regarding the short-term prediction of suicidal ideation (SI) and suicidal behavior (SB) [Reference Glenn and Nock1], i.e. the processes leading to SI and SB in time frames of hours or days (proximal risk factors) [Reference O’Connor and Nock2, Reference Franklin, Ribeiro, Fox, Bentley, Kleiman and Huang3]. Variables such as depressiveness, hopelessness, rage, anger, anxiety, and sleeping problems were identified as variables elevating suicide risk and increasing SI in the short-term while findings seem to be most robust for depressiveness and hopelessness [Reference Hawton, Casañas, Comabella, Haw and Saunders4–Reference Rudd, Berman, Joiner, Nock, Silverman and Mandrusiak9].
Yet, a recent meta-analysis has concluded that the prediction of imminent suicide risk has not substantially improved over the past 50 years and pointed out the need of assessing suicidal phenomena repeatedly [Reference Franklin, Ribeiro, Fox, Bentley, Kleiman and Huang3], e.g. because SI has been shown to fluctuate considerably [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10, Reference Hallensleben, Spangenberg, Forkmann, Rath, Hegerl and Kersting11]. Although it has not been established yet in detail, which factors determine the individuals’ transition from suicidal thoughts to suicidal actions, the presence of SI is a major risk factor for the emergence of actual SB. Consequently, understanding the development of SI, the role of proximal risk factors and monitoring its course over time is an important part of suicide prevention. Studies applying ecological momentary assessments (EMA) allow examining variables of interest in real time, and in participants’ natural environment [Reference Verhagen, Hasmi, Drukker, van Os and Delespaul12, Reference Santangelo, Ebner-Priemer, Trull, Comer and Kendall13] and are a very promising approach in suicide research [Reference Glenn and Nock1, Reference de Beurs, Kirtley, Kerkhof, Portzky and O’Connor14].
1.1. The interpersonal theory of suicide
The Interpersonal Theory of Suicide (IPTS) posits two interpersonal factors that lead to suicidal desire: thwarted belongingness (TB) and perceived burdensomeness (PB) [Reference Joiner15]. TB describes the unmet need of being socially integrated, and PB reflects the perception of being a burden on others. The sole presence of one of these factors causes passive SI (i.e., having death wishes such as “I wish I was dead.”), whereas the simultaneous presence of PB and TB (i.e., a two-way interaction) in connection with hopelessness regarding their decrease is assumed to lead to active SI (i.e., experiencing a desire to engage in suicidal behaviors such as “I want to kill myself.”) [Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16]. TB and PB are assumed to be dynamic and, thus, modifiable cognitive-affective states [Reference Joiner15, Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16]. According available empirical evidence, the strongest support has been found for the effect of PB and for the interaction of PB and TB on SI, while the association between TB and SI showed to be less consistent [Reference Ma, Batterham, Calear and Han17, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]. However, only very few studies have tested the main as well as the interaction effects of PB and TB proposed by the IPTS, have applied prospective designs, or have specifically focused on individuals at elevated risk for suicide [Reference Ma, Batterham, Calear and Han17, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18].
1.2. EMA studies on SI
Very few studies have examined SI and its risk factors employing EMA so far [Reference Spangenberg, Forkmann and Glaesmer19, Reference Kleiman and Nock20] revealing a predictive effect for negative affective states on SI [Reference Ben-Zeev, Young and Depp6, Reference Palmier-Claus, Taylor, Gooding, Dunn and Lewis21, Reference Links, Eynan, Heisel, Barr, Korzekwa and McMain22]. Regarding the short-term variability of SI, Kleiman et al. (2017) have reported substantial variability in SI within a time frame of four to eight hours demonstrating that a considerable amount of variation (33%–47%) in SI is attributable to within-person variance [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10]. A preliminary analysis (N = 20) of the present study has also demonstrated considerable fluctuations in SI within an even shorter time frame of 30 min up to two hours [Reference Hallensleben, Spangenberg, Forkmann, Rath, Hegerl and Kersting11]. Variables discussed at proximal risk factors (hopelessness, PB, and TB) were as well subject to considerable within-person fluctuation and co-occurred with SI in cross-sectional multi-level analyses. However, in prospective multi-level analyses, neither hopelessness nor PB, or TB predicted short-term changes in SI when controlling for SI at the previous measurement occasion [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10]. A recent daily diary study also demonstrated concurrent associations between SI and interpersonal variables and hopelessness and provided initial support for prospective associations between the interaction of interpersonal variables and SI [Reference Czyz, Horwitz, Arango and King23].
1.3. Aims
Our study aims to further investigate the short-term variability of SI. In addition, we examined cross-sectional as well as prospective associations between SI and variables suggested as proximal risk factors by the IPTS (i.e. PB and TB, [Reference Joiner15]) accounting for well-established risk factors of SI such as depressiveness (i.e. sad mood) and hopelessness [Reference Hawton, Casañas, Comabella, Haw and Saunders4, Reference Ben-Zeev, Young and Depp6, Reference Rudd, Berman, Joiner, Nock, Silverman and Mandrusiak9]. We conducted an EMA study in a sample of psychiatric inpatients with unipolar depression, where we expected SI to occur frequently [Reference Sokero, Melartin, Rytsala, Leskela, Lestela-Mielonen and Isometsa24].
In order to extend current evidence and examine the assumptions of the ITPS more stringently [Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16, Reference Kleiman and Nock20], we 1) applied a high-frequency sampling scheme (10 signals per day within a time frame of 12 hours), 2) assessed all variables of interest with two items (ensuring reliable assessment) [Reference Forkmann, Spangenberg, Rath, Hallensleben, Hegerl and Kersting25], 3) distinguished between passive and active SI, and 4) included the interaction between PB and TB in our analyses.
2. Method
2.1. Procedure
Eligible patients in three German psychiatric hospitals were approached and informed about the study by a research assistant (N = 196). Informed consent was provided by those who were willing to participate (N = 92). Of those, 17 (18%) were excluded because they did not meet the inclusion criteria (i.e. primary diagnosis of unipolar depression, current or life-time SI, age ≥18 years, fluent in German). Patients were further excluded if they had a bipolar affective disorder, psychotic symptoms, substance addiction in the past year, or an IQ below 85 according to a language based intelligence test [Reference Lehrl26]. Four participants from the pilot phase were additionally included in the study resulting in N = 79 patients.
Every participant received 10€ for compensation and additional 40€ if having completed at least 80% of the EMA prompts. All study procedures were approved by the Ethical Review Board of the Medical Faculty of University of Leipzig (No: 388-13-16122013).
2.2. Participants
Five of the included participants (6%) did not finish the EMA assessment due to high strain (n = 3) or unexpectedly early discharge from hospital (n = 2). Thus, data of 74 participants (collected 8/2015 to 7/2017) were analyzed (N = 69 with major depression, N = 5 with dysthymia). Age was between 18 and 85 years (M = 37.6, SD = 14.3), N = 53 (71.6%) of the participants were female and N = 24 (33.8%) reported one or more prior suicide attempts.
2.3. Assessments
2.3.1. Baseline
Participants underwent a structured clinical interview (SCID-I) [Reference Wittchen, Zaudig and Fydrich27] to ensure diagnosis of depression.
2.3.2. EMA
EMA data collection was conducted via movisensXS [28] on Android smartphones that were lent to the participants. Participants were signaled 10 times per day on six consecutive days; signals occurred randomly between 8:00 a.m. and 7:50 p.m. with a minimum interval of 30 minutes between prompts (i.e. signal-contingent). At every prompt, participants were asked to rate their momentary level of passive (Life is not worth living for me.; There are more reasons to die than to live for me.) and active SI (I think about taking my life., I want to die.), depression (I feel sad., …downhearted.), hopelessness (My future seems dark to me., I might as well give up because there is nothing I can do about making things better for myself.), PB (I feel useless., …like a burden for others.), TB (I feel lonely., …like I do not belong.). Each construct was measured with two items using a 5-point Likert scale (1 – not at all to 5 – extremely) resulting in sum scores (ranging from 2 to 10) with higher values indicating a higher level of the respective construct.
EMA items were taken from existing EMA instruments (e.g., German PANAS-X [Reference Gruehn, Kotter-Gruehn and Roecke29]), selected from relevant self-report instruments considering item-total correlation, item content and wording (e.g., the Interpersonal Needs Questionnaire (INQ) [Reference Glaesmer, Spangenberg, Scherer and Forkmann30, Reference Hallensleben, Spangenberg, Kapusta, Forkmann and Glaesmer31], the German Beck Hopelessness Scale (BHS) [Reference Kliem and Brähler32], the Paykel Suicide Scale (PSI) [Reference Paykel, Myers, Lindenthal and Tanner33], the Modified Scale for Suicidal Ideation (MSSI) [Reference Miller, Norman, Bishop and Dow34], the German Beck Scale for Suicide Ideation (BSS) [Reference Kliem and Brähler35]), or were newly developed. In a second step, item wording was adjusted to be as brief as possible and to refer to the actual moment. Confirmatory factor analysis on the within-person covariance matrix supported the factorial validity of the item set with depression, hopelessness, PB, TB, passive and active SI reflecting different latent constructs. Reliabilities were excellent on the person-level (ω ≥.90) and good at the prompt-level (ω ≥.70) for all constructs considered in the analysis. Convergent validity was indicated by positive correlations (all r ≥.55) between mean EMA scores and sum scores of self-report questionnaires filled in after the EMA assessment measuring the same construct (i.e., INQ, BHS, BSS and the Rasch-based Depression Screening (DESC) [Reference Forkmann, Boecker, Wirtz, Eberle, Westhofen and Schauerte36]) [Reference Forkmann, Spangenberg, Rath, Hallensleben, Hegerl and Kersting25].
2.4. Data analysis
The dataset consisted of 60 (assessments on level 1) * 74 (persons on level 2) = 4,440 observations. Participants completed 89.7% of the EMA assessments on average (Min = 75%, Max = 100%), resulting in 4,295 valid observations. Due to the nested structure of the data, we conducted multilevel analyses using the statistical software HLM [Reference Raudenbusch, Bryk and Congdon37]. Figures were created by using R, ggplot2 package [Reference Wickham38, Reference R Core Team39].
In a first step, we calculated the intercept-only model for both outcomes (passive and active SI) and intra-class correlations (ICC) as an indicator of the proportion of variance explained by the different levels [Reference Hox40]. To further describe variability across time, we calculated Mean Squared Successive Differences (MSSD). The MSSD is a sum score of the squared differences between two measurement occasions in time series and thus represents point-to-point variability with higher values indicating higher fluctuation [Reference Woyshville, Lackamp, Eisengart and Gilliland41].
Secondly, we computed a baseline model for both outcome variables. The baseline models contained the time lagged SI (passive or active) at level 1 to account for autocorrelation of SI in all further models. These models were used as reference models to evaluate the incremental value of the level 1 predictors using a Quasi R2 measure indicating the change of the outcome’s residual variance when adding the model’s level 1 predictors [Reference Hox40, Reference Hayes42]. We used the R2 (S&B) formula [Reference Snijders and Bosker43], as this can be applied to models containing random slopes [Reference LaHuis, Hartman, Hakoyama and Clark44].
Thirdly, two models were fitted for passive SI (model 1 with cross-sectional predictors at level 1, model 2 with time-lagged predictors at level 1) and four for active SI (model 3a and 3b with cross-sectional predictors at level 1, model 4a and 4b with time-lagged predictors at level 1, the latter including the interaction term PBxTB). Besides the recommendation to generally allow random slopes in the model where applicable [45], we conducted deviance tests for all models revealing better fit for the random slopes models in comparison to the more restrictive random intercept model. Yet, because we were primarily interested in the fixed effects, random effects are not reported in the paper besides the estimated percentage of slope coefficients that are positive [Reference Hox40].
All models were estimated by means of restricted maximum likelihood estimation (REML), as our number of level 2 units is relatively small [Reference Hayes42] and the predictor variables were person-mean centered in all analyses, as we were particularly interested in within-person relationships [Reference Enders and Tofighi46]. In models 2 and 4, predictors were time lagged to the previous measurement occasion (t-1). In doing so, the last value per day was not lagged to avoid obtaining “between-days” lags. Our analyses were sufficiently powered to detect moderate to large effects on the observational level (level 1) [Reference Kleiman47].
3. Results
3.1. Short-term variability
Across all assessments, the proportion of SI nonzero ratings was 64.3% for passive SI and 38.9% for active SI. Two participants (3%) did not report any SI and 13 participants (18%) did not report any active SI. ICCs indicate that in hopelessness and passive SI around 25% of the variance is accounted for by within-person variability. For active SI, TB, PB, and depressiveness, between 36% and 47% of variance is due to within-person variability according ICCs (see Table 1). Mean MSSD values illustrate that there was on average considerable moment-to-moment variability in all constructs. Yet, MSSDs showed a wide range, indicating that this variability differed substantially between individuals (see Table 1). In Fig. 1, heat maps visually illustrate individual moment-to-moment variability for SI and the risk factors.
3.2. Multilevel analyses
3.2.1. Outcome passive SI
Depressiveness, hopelessness, PB, and TB are significantly positively associated with passive SI, beyond the effects of time lagged passive SI (model 1). For the majority of participants (71–97%), the associations between predictors in model 1 and passive SI were positive (see ratio of slopes > 0 in Table 2).
In model 2, the levels of hopelessness, PB, and passive SI at t-1 significantly positively predicted passive SI at time t. Contrary to our expectations, time lagged TB and depressiveness did not predict passive SI at time t, which was accompanied by lower ratios of positive slopes (60% for depressiveness and 50% for TB).
3.2.2. Outcome active SI
When considering the main and interaction effects of the interpersonal variables cross-sectionally (model 3a and 3b), depressiveness, hopelessness, TB, and PB were positively significantly associated with active SI (co-occurred). For TB and PB, between 64 and 70% of participants showed positive associations with active SI (see Table 3).
Table 1 Descriptive statistics and variability indices of the EMA scales.

Note: SD = standard deviation, Min = minimum, Max, = maximum, MSSD = mean squared successive difference, ICC = intraclass correlation; all constructs were measured with two items resulting in a sum score from 2 to 10;
Data in this table was presented in Forkmann et al. (in press)25, as part of a large psychometric analysis of the EMA item set used in this study.
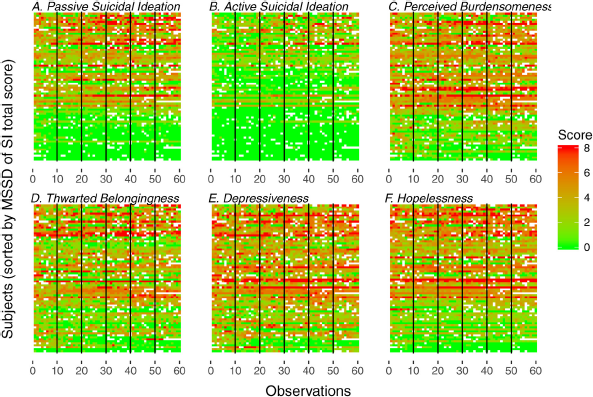
Fig. 1. Heat maps of momentary ratings of suicidal ideation and risk factors across observations and participants.
Note: The ratings of momentary SI and the considered risk factors are coded by color. Green (light gray) indicates low and red (dark gray) indicates high momentary levels of the respective construct. Missing observations are not colored.
In each heat map, one row represents one participant and each square represents one momentary rating (interval between ratings ranged from 30 minutes to few hours). On the x-axis, vertical lines separate the days (day 1 to 6) of the assessment. On the y-axis, participants are sorted by their MSSD in overall suicidal ideation (including passive and active suicidal ideation) with higher MSSD values in the upper part of the heat maps and lower MSSD values in the lower part. In Fig. 1A and 1B (passive and active suicidal ideation), the lower part of the figures is dominated by green (light gray), indicating the absences or very low levels of suicidal ideation. For active suicidal ideation, yellow (middle gray) and red shades (dark gray) are rare in comparison with the other variables. With this exception, the momentary ratings of all depicted variables varied within participants and across time as indicated by color changes within rows.
In the prospective models 4a and 4b, TB did not predict active SI, while hopelessness, PB, and the interaction of PB and TB at t-1 significantly predicted active SI (see Table 3).
4. Discussion
4.1. Short-term variability of SI
The results further demonstrated that SI as well as the risk factors under study (i.e., PB, TB, hopelessness, and depressiveness) are subject to considerable within-person variability over short time periods [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10, Reference Hallensleben, Spangenberg, Forkmann, Rath, Hegerl and Kersting11]. It is noteworthy that these fluctuations appeared in very short time frames (i.e., intervals of 30 minutes up to few hours) in our study. This finding clearly supports the necessity of assessing SI repeatedly and in real-time to obtain ecologically valid insights in the onset and course of SI [Reference Glenn and Nock1, Reference de Beurs, Kirtley, Kerkhof, Portzky and O’Connor14].
4.2. Real-time associations between SI and interpersonal variables
As expected, according to the IPTS [Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16] and previous evidence from other, mostly cross-sectional, studies [Reference Ma, Batterham, Calear and Han17, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18], PB and TB showed positive concurrent associations with passive SI beyond the effect of hopelessness and depressiveness, generally supporting the pathway to passive SI specified in the IPTS. Yet in the prospective analyses, we found an association between PB and passive SI only. For active SI, a different picture emerged: PB, TB, depressiveness, and hopelessness co-occurred with active SI, while the interaction term of PB and TB was not significant in the cross-sectional model. Interestingly, hopelessness and PB as well as the interaction term significantly predicted active SI prospectively (models 4a and 4b). The effect of the interaction appeared to be small, which is in line with meta-analytic evidence from cross-sectional studies showing that the effect of the two-way interaction between PB and TB is relatively weak in comparison to the mostly moderately sized main effects of PB and TB [Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]. Additional support for the concurrent and prospective value of the interaction between PB and TB was provided by a recent daily diary study [Reference Czyz, Horwitz, Arango and King23]. Hence, the divergence between cross-sectional and prospective analysis in our study might be a result of the limited power to detect small effects and the lower base rate of active SI (compared to passive SI) in the investigated sample.
The finding that PB seems to be a more valid predictor for SI than TB is well-known from a number of previous studies with cross-sectional designs [Reference Hill and Pettit48–Reference Bryan, Morrow, Anestis and Joiner52] and is also in line with meta-analytic evidence showing that PB is a more robust prospective predictor of suicidal thoughts [Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]. Using an EMA approach, Kleiman et al. [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10] have found concurrent associations between the interpersonal variables, hopelessness, and SI, but could not demonstrate any prospective associations when accounting for the autocorrelation of SI., Our study further supports initial evidence for the prospective value of the interpersonal variables [Reference Czyz, Horwitz, Arango and King23] and provides partial evidence for the assumptions of the IPTS employing prospective analysis (especially regarding the link between PB and SI). The rather small effects found in our study, however, cast doubt on the clinical utility of the results as has been previously discussed [Reference Franklin, Ribeiro, Fox, Bentley, Kleiman and Huang3, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18] and point out that the postulates of the IPTS might not fully capture the variety of individual influences and trajectories of SI.
Table 2 Parameter estimates for multilevel models with passive suicidal ideation as outcome variable (models 1 and 2).

Notes: N (Level 2) = 74. N (Level 1) = 4295. All level-1 predictors were person-mean centered. Est. = Estimate (unstandardized regression coefficient). 95% CI (Est.) = 95% confidence interval for Est. SE = standard error.
1 Based on the assumptions of normally distributed slope coefficients, this value indicates the estimated percentage of slope coefficients that are positive36.
2Quasi R2 indicates the change of the residual variance in passive suicidal ideation when adding the models’ level 1 predictors compared to the baseline models40.
4.3. Real-time associations between hopelessness, depression, and SI
Notably, hopelessness had the most robust and largest effect on SI across all cross-sectional and prospective models. The importance of hopelessness as a risk factor for suicidality (especially for SI) has previously been demonstrated in a multitude of studies assessing hopelessness via questionnaires [Reference Nock and Kazdin7, Reference Wang, Jiang, Cheung, Sun and Chan8, Reference Beevers and Miller53, Reference Brezo, Paris and Turecki54]. For state hopelessness assessed in real-time, findings are inconclusive: While Kleiman et al. [Reference Hallensleben, Spangenberg, Forkmann, Rath, Hegerl and Kersting11] found hopelessness being associated with concurrent and subsequent SI (which did not hold when controlling for preceding SI, however), others [Reference Ben-Zeev, Young and Depp6] could not detect a relation between hopelessness and subsequent SI (when accounting for preceding SI). Despite the specific role of hopelessness about PB and TB in the IPTS [Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16], this aspect has been fairly neglected by the majority of studies examining the IPTS including our own [Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]. In light of the relevance of general hopelessness in our results we would strongly recommend to include hopelessness regarding the changeability of PB and TB in future investigations. The effect of depressiveness on SI was less robust in our study: While depressiveness was associated with SI in all our cross-sectional analyses, it had no predictive effect in the prospective analyses contradicting previous studies [Reference Ben-Zeev, Young and Depp6, Reference Husky, Swendsen, Ionita, Jaussent, Genty and Courtet55]. However, these studies slightly differed from ours in terms of methodology (items, EMA assessment).
4.4. Strengths and limitations
To the best of our knowledge, this is the first EMA-study that distinguishes between passive and active SI, allowing for empirically testing specific IPTS assumptions [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10, Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner16, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]. Besides other notable strengths (excellent compliance, assessing all variables with two reliable and valid EMA items [Reference Forkmann, Spangenberg, Rath, Hallensleben, Hegerl and Kersting25]), our findings should be considered in the context of several limitations. We examined a rather homogeneous sample of depressed inpatients, and active SI was reported by 61 of 74 participants (82%). Moreover, only 46.7% of eligible inpatients consented to participate in the study further limiting the generalizability of our findings. While our findings can be integrated in the available empirical evidence on short-term variability of SI and its risk factors [Reference Spangenberg, Forkmann and Glaesmer19, Reference Kleiman and Nock20, Reference Czyz, Horwitz, Arango and King23] and the IPTS [Reference Kleiman, Turner, Fedor, Beale, Huffman and Nock10, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18, Reference Czyz, Horwitz, Arango and King23], further research in other clinical and non-clinical populations is needed to underpin the generaliziability of the findings. Although suicide research needs new and objective ways of measuring suicide risk (e.g., indirect measures of suicide-related variables as well as behavioral proxies [Reference Glenn and Nock1, Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18]), we only used self-reports. Because data on the temporal course of SI and its risk factors is still scarce [Reference Spangenberg, Forkmann and Glaesmer19, Reference Kleiman and Nock20], it is also unclear if our sampling strategy fits the dynamics of its natural course [Reference Verhagen, Hasmi, Drukker, van Os and Delespaul12, Reference Ebner-Priemer, Trull, Mehl and Conner56]. Moreover, it remains unclear whether a satisfactory operationalization of the IPTS constructs has already been attained by the available instruments and items such as the INQ [Reference Hallensleben, Spangenberg, Kapusta, Forkmann and Glaesmer31]. While, overall, our EMA items showed good reliability and convergent validity with the commonly used INQ [Reference Forkmann, Spangenberg, Rath, Hallensleben, Hegerl and Kersting25], psychometric limitations of this operationalization apply to our study as well potentially limiting the ability to draw conclusions on the validity of the IPTS [Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker and Hagan18].
4.5. Conclusion
One of the strongest clinical implications of this study is the need to assess SI and its risk factors repeatedly in short time frames of hours and days (as has been recommended before) [Reference Glenn and Nock1, Reference de Beurs, Kirtley, Kerkhof, Portzky and O’Connor14]). Future studies might extend observations to longer periods of several weeks to gain more insight in the individual occurrence, course, and decline of SI [Reference Forkmann, Spangenberg, Rath, Hallensleben, Hegerl and Kersting25, Reference Ebner-Priemer, Trull, Mehl and Conner56]. Although we could identify variables that predicted changes in SI prospectively, the effects generally appear to be small and only partially in line with theoretical assumptions warranting further investigation. It might be useful to focus specifically on person-level or cross-level effects or to conduct subgroup analyses (i.e., differentiate between persons experiencing passive and active SI or persons with and without suicide attempt history). Because of the low base rate of persons experiencing active SI and with a history of suicide attempt(s), such analyses were not possible in our study for reasons of power. More complex models such as the Integrated Motivational-Volitional model of suicidal behavior [Reference O’Connor57] that include more variables that serve as moderator or mediator in the development of SB might also lead to larger effects because of the combination of several predictors.
Table 3 Parameter estimates for multilevel models with active suicidal ideation as outcome variable (models 3 and 4).
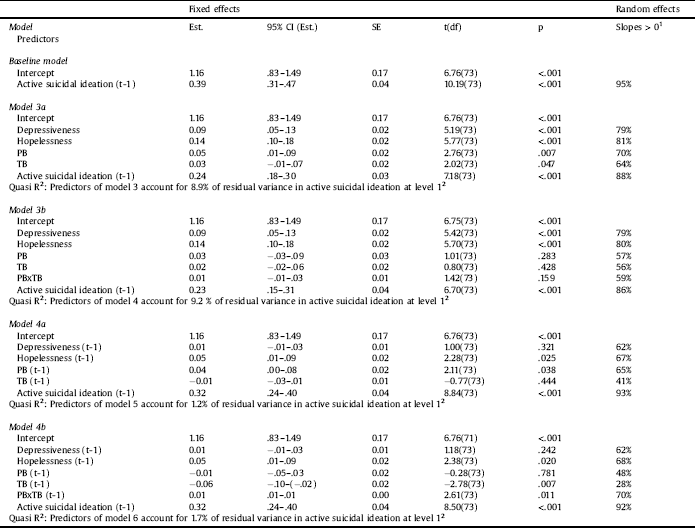
Notes: N (Level 2) = 74. N (Level 1) = 4295. All level-1 predictors were person-mean centered. Est. = Estimate (unstandardized regression coefficient). 95% CI (Est.) = 95% confidence interval for Est. SE = standard error.
1Based on the assumptions of normally distributed slope coefficients, this value indicates the estimated percentage of slope coefficients that are positive.36
2Quasi R2 indicates the change of the residual variance in active suicidal ideation when adding the models’ level 1 predictors compared to the baseline models.40
Potential conflicts of interest
None.
Funding
This research was supported by research grants no. SP 1556/1-1, GL 818/1-1 and FO 784/1-1 from the German Research Foundation.
Role of the sponsor
The supporters had no role in the design, analysis, interpretation, or publication of this study.
Previous presentation
Poster presented at the IASR/AFSP International Summit on Suicide Research, Henderson, Nevada, November 5–8, 2017. Poster presented at the 5th Biennial Conference of the Society for Ambulatory Assessment, Luxembourg, June 15–17, 2017. Presentation at the IASR/AFSP International Summit on Suicide Research, Henderson, Nevada, November 7th, 2017. Presentation at the 16th European Symposium for Suicide and Suicidal Behavior, Oviedo, Spain, September, 9th, 2016, Presentation at the German Congress for Psychosomatic Medicine and Psychotherapy (DKPM), Berlin, Germany, March, 8th, 2018.







Comments
No Comments have been published for this article.