CLINICIAN'S CAPSULE
What is known about the topic?
While the short-term (30-day) prognosis for emergency department (ED) syncope is well studied, long-term outcomes (beyond 30 days) are not well studied.
What did this study ask?
What is the long-term (1 year or later) prognosis, particularly mortality and cardiac morbidity, among ED patients with syncope?
What did this study find?
There was a notable mortality (7%), a sizeable cohort (16%) with recurrent syncope requiring hospitalization, and 6% required device insertion.
Why does this study matter to clinicians?
Emergency physicians should be aware of the long-term outcomes and develop follow-up plans to reduce morbidity and mortality.
INTRODUCTION
Syncope is defined as a “transient loss of consciousness due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery.”Reference Brignole, Moya and de Lange1 Syncope accounts for 1%–3% of all emergency department (ED) visits, and among 50% of these patients, the cause of syncope is still unknown at the end of the ED evaluation.Reference Brignole, Menozzi and Bartoletti2,Reference Feraco, Grandinetti, Lauro and Cosentino3 Short-term outcomes between 0 and 30 days are well studied among ED patients with syncope. Overall, approximately 10% of patients experience serious outcomes within 30 days, including 1%–5% of patients with myocardial infarction; 4%–7% with arrhythmias; and <1% with each of the following serious outcomes: death, serious structural heart disease, significant hemorrhage, subarachnoid hemorrhage, or pulmonary embolism.Reference Quinn, McDermott, Stiell, Kohn and Wells4–Reference Mukarram, Taljaard and Sivilotti13 However, long-term outcomes are not well studied. Long-term outcomes are equally important to guide management decisions in the ED to help reduce long-term morbidity and mortality for patients. With a better understanding and appreciation of long-term risks, ED physicians can set-up appropriate follow-up for these patients with family physicians, as well as cardiologists. Therefore, this review will focus on long-term outcomes, particularly cardiac morbidity and mortality that occurred up to one-year after the initial episode of syncope.
METHODS
This was a systematic review of literature for long-term outcomes at one year or later of patients with syncope who presented to the ED. We decided a priori to perform a meta-analysis for each outcome at one-year if our review identified data to perform such an analysis. We searched the following databases: Cochrane Central Register of Controlled Trials (CENTRAL) using OVID, Medline and Medline in Process (using OVID), PubMed, Embase (using OVID), and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). A search strategy was developed to identify keywords and medical subject headings (MeSH) in Medline that were then adapted for all other databases. The search was conducted by a librarian with considerable expertise in systematic review search strategy (LS), from the inception of each database to June 23, 2017. An updated literature search was later performed to include articles published up until December 2018. A search strategy was developed to identify keywords and MeSH in Medline that were then adapted for all other databases (Supplemental Appendix 1). We used EndNote software to organize our articles obtained from the above search strategy. We included articles that enrolled adult patients (aged ≥16 years old) who presented to the ED with syncope and had at least a 12-month follow-up after the initial episode. Articles that reported pertinent long-term outcomes of mortality, arrhythmia, pacemaker or implantable cardioverter-defibrillator (ICD) insertion, and hospitalization because of recurrent syncope were included. We excluded articles that enrolled pediatric patients; patients with pre-syncope; those patients with non-syncope-related transient loss of consciousness such as hypoglycemia, transient ischemic attack, stroke, or seizure; those studies conducted in non-ED settings, case reports, and letters to editor; and those studies for which full-text articles could not be obtained. We excluded non-English articles, as there was no evidence that this exclusion would affect the generalizability of measured outcomes.Reference Morrison, Polisena and Husereau14,Reference Jüni, Holenstein, Sterne, Bartlett and Egger15 Our review included articles with large population sizes from North America and Europe published in English that would likely be representative of the wider population once meta-analyzed. If required, we contacted the authors for clarification of outcomes and their timing at least twice before excluding them from further analysis.
Two reviewers (CL and PH) screened the articles first based on the title and abstract, and, then, full articles were reviewed for inclusion. Disagreements during the article selection were resolved by consensus and, if required, adjudicated, by a third investigator (MM).
Outcomes measures
The outcome measures selected for this systematic review were all-cause mortality, recurrence of syncope requiring hospitalization, detection of new arrhythmia, and device implantation for treatment of arrhythmia at 12 months or later from the index syncope.
Quality assessment
Two authors (CL and PH) independently evaluated the included studies for quality assessment and risk of bias using the SIGN 50 tool.16 This tool evaluates 14 domains: study question, study population, recruitment, dealing with patients with obvious outcomes, lost to follow-up, comparison of those with and without follow-up, clear definition of outcomes, blinding to outcome assessment, dealing with unblinded exposure, reliability of data collection, valid and reliable outcome assessment, inter-rater reliability of data collection, confounding, and reporting of results with confidence intervals. Articles were given a “yes” if they met the domain criteria, “no” if they did not meet the domain criteria, and “can't say” if they partially met the domain criteria or it could not be determined. CL and PH independently determined if the article was of unacceptable, acceptable, or highly acceptable quality. Unacceptable quality was defined as high risk of bias with conclusions likely to change in future research. Acceptable was defined as moderate risk of bias with possibility of conclusions changing with future research. Highly acceptable was defined as low risk of bias, conclusions unlikely to change results with further research. Disagreements were solved by discussions between CL and PH, and, herein, we report the consensus results.
Data analysis
Inter-rater agreement was made using a kappa analysis at each step of the article selection process and quality assessment. We performed a meta-analysis for outcomes at 12 months from the index syncope. Additionally, we report outcomes beyond 12 months by conducting a descriptive analysis and, if possible, report outcomes between days 31 and 365 by conducting a sensitivity analysis.
The proportions of patients experiencing an outcome in the included studies were pooled using a random effects generic inverse variance meta-analysis (RevMan v.5.3; Cochrane Collaboration). The I 2 statistic was used to assess heterogeneity: I 2 values of more than 75% were considered to represent high heterogeneity. The pooled proportion of patients experiencing an outcome was calculated using the generic inverse variance method. Point estimates and 95% confidence intervals (CI) were calculated. We performed a sensitivity analysis to see the effects on heterogeneity by removing the studies that reported disproportionate results in comparison with others and limiting to only prospective studies.
RESULTS
Literature search
Our initial literature search found 2,094 articles after removal of duplicates (Figure 1). CL and PH screened the articles. After title and abstract screening, 50 articles were selected for a full-text review (κ = 0.85, 95% CI 0.77–0.93). After a full-text assessment, 16 articles were selected for inclusion in the systematic review (κ = 0.86, 95% CI 0.71–1.00). We excluded two articles at this stage. Nume et al. reported only deaths because of motor vehicle accidents related to syncope and, hence, were excluded.Reference Numé, Gislason, Christiansen, Zahir, Hlatky and Torp-Pedersen17 We excluded an article by Ungar et al 2010, as this study used the same cohort of patients as the study done by Del Rosso et al.Reference Ungar, Del Rosso and Giada18 An updated literature search was performed to include articles up until December 2018. Of the 692 articles found in the updated literature search, three additional articles by Sandhu et al., Baron-Esquivias et al., and Du Fay De Lavallaz et al. were found and included in our systematic review.Reference Sandhu, Tran, Sheldon and Kaul19–Reference du Fay de Lavallaz, Badertscher and Nestelberger21 The articles by Du Fay De Lavallaz et al. and Baron-Esquivias et al. reported outcomes beyond one year and did not explicitly report one-year outcomes. The authors did not respond to our attempts to clarify the data. Therefore, these two studies were included in the systematic review, and we were unable to include them in the meta-analysis. We reviewed the bibliography of all included studies to identify potential articles that were missed. Of the 424 references, no new articles were included in the systematic review.

Figure 1. Article collection and data extraction, PRISMA diagram
We found a total of 19 articles with long-term outcomes in ED patients with syncope and were included in this review. Of the 19 articles, we were able to extract or obtain data for one-year outcomes for 12 studies and were included in the meta-analysis; 10 studies reported outcomes between 31 and 365 days and were included in the sensitivity analysis. A description of eight articles that report outcomes beyond 12 months is included in this review.
Table 1 shows the characteristics of the 19 studies included in the systematic review. There were 14 prospective and 5 retrospective studies. Most of the included articles were single-centre studies with a sample size ranging from 75 to 51,831 patients.
Table 1. Summary of accepted articles included

NR = not recorded.
*Indicates articles for which outcomes were available but only for >12 months after the index syncopal episode. These articles were not included in the meta-analysis.
†Indicates articles that included a follow-up of >12 months; however, day 0 to day 365 data could be extracted.
Main results
There were 12 articles that reported one-year outcomes (Table 2). All 12 studies reported one-year mortality rates. A pooled analysis showed that the proportion of ED patients with syncope who will die within one year of their index syncope was 7.0% (95% CI 6.0%–9.0%, I2 = 83%). Figure 2a shows the forest plot for one-year mortality. Because of high heterogeneity, we performed a subgroup analysis based on study design comparing retrospective and prospective studies. This showed that the proportion of patient who die within one year of the index syncope in the retrospective studies was 6.0% (95% CI 4.0%–9.0%, I2 = 74%) compared with 7.0% (95% CI 6.0%–9.0%, I2 = 37%) mortality in the prospective studies. There was no significant difference in the mortality rates between the two types of studies, retrospective versus prospective (p = 0.60).

Figure 2a. Forest plot for morality from day 0 to day 365.

Figure 2b. Forest plot for device insertion for day 0 to day 365.

Figure 2c. Forest plot for recurrence of syncope requiring admission for day 0 to day 365.
Table 2. Summary of outcomes day 0 to day 365

NR = not recorded.
*Other outcomes included pacemaker insertion, ICD, new arrhythmia, and recurrence of syncope requiring admission.
†Study had follow-up of >12 months; however, 12-month data could be extracted.
Three studies reported one-year device insertion for treatment of arrhythmias related to syncope. Pooled analysis showed that 6.0% (95% CI 2.0%–11.0%, I2 = 95%) of the patients would have a pacemaker or an ICD inserted within one year of the index syncopal episode. Device insertion rates ranged from 2.59% as reported by Reed et al. in 2011 to 14.8% as reported by Gomes et al. The heterogeneity seen in the pooled analysis was largely driven by a study by Gomes et al; however, we cannot conclude as to why there was such a large variation. Figure 2b shows the forest plot for device insertion at one year.
Two studies, Ungar et al. and Baranchuck et al., reported recurrence of syncope within one year requiring admission. A pooled analysis showed that 16.0% (95% CI 12.0%–20.0%, I2 = 0.0%) of patients would have a recurrent episode of syncope that requires hospitalization for further workup (Figure 2c). We were unable to extract data for the one-year meta-analysis for this outcome from the article by Sandhu et al., and the authors were unable to provide these data. Hence, this study was excluded from the meta-analysis for this outcome.
Two studies by Silva et al. and Reed et al. in 2011 reported new arrhythmias at 26.4% and 1.06%, respectively. However, there was significant variation in the reported proportions; therefore, we did not perform a meta-analysis. This large variation is most likely because of significantly different definitions of significant arrhythmia as reported by the two working groups.
Sensitivity analysis for outcomes from day 31 to day 365
To perform this sensitivity analysis, only studies for which day 0 to day 30 outcomes could be removed were used. Two studies, Gomes et al. and Reed et al. (2011), did not report 30-day outcomes in their original article. However, we were able to contact both authors and obtain the 30-day outcomes to include them in the sensitivity analysis. A total of 10 studies were included in this sensitivity analysis (Supplemental Appendix Table 1).
All 10 studies reported mortality from day 31 to day 365. A pooled analysis showed that the proportion of ED patients with syncope who die after 30 days but up to 1 year was 5.0% (95% CI 4.0%–6.0%, I2 = 79.0%). Because of high heterogeneity, we performed a subgroup analysis based on study design. This subgroup analysis showed that mortality among ED patients with syncope was 5.0% (95% CI 2.0%–7.0%, I2 = 75.0%) in the retrospective studies and 5.0% (95% CI 4.0%–7.0%, I2 = 78.0%) among patients in the prospective studies. There was no significant difference in mortality after 30 days until 1 year between the prospective and retrospective studies (p = 0.71). Appendix Figure 1a shows the forest plot for mortality from day 31 to day 365.
Two studies reported device insertion from day 31 to day 365. A pooled analysis showed that the proportion of ED patients with syncope who would have a pacemaker inserted between day 31 and day 365 was 1.0% (95% CI 1.0%–2.0%, I2 = 0.0%). Neither study reported insertion of an ICD beyond day 30. Appendix Figure 1b shows the forest plot for device insertion between day 31 and day 365. Only Ungar et al. provided data for recurrence of syncope requiring hospitalization from day 31 to day 365 that was reported at 11.6%.
Outcomes beyond day 365
Supplemental Appendix Table 2 shows a summary of outcomes for studies with follow-up of more than 12 months including the duration of follow-up. Mortality for studies with follow-up months ranged from 4.9% to 21.0%. Shen et al. and Baron-Esquivias et al. reported recurrence of syncope requiring hospitalization as 6.8% and 18.6%, respectively. Only Shen et al. reported device insertion in 11.7%. Shen et al. and Martin et al. reported arrhythmia in 6.8% and 11.5%, respectively.
A quality assessment and risk of bias SIGN-50 tool was used to complete the quality assessment and risk of bias for all articles. All articles were found to be of acceptable quality, meeting most criteria with some weaknesses in the included studies that may be associated with bias (κ for quality assessment 0.90, 95% CI 0.85–0.95). Results of the quality assessment are shown in Table 3.
Table 3. Quality assessment using SIGN-50 tool
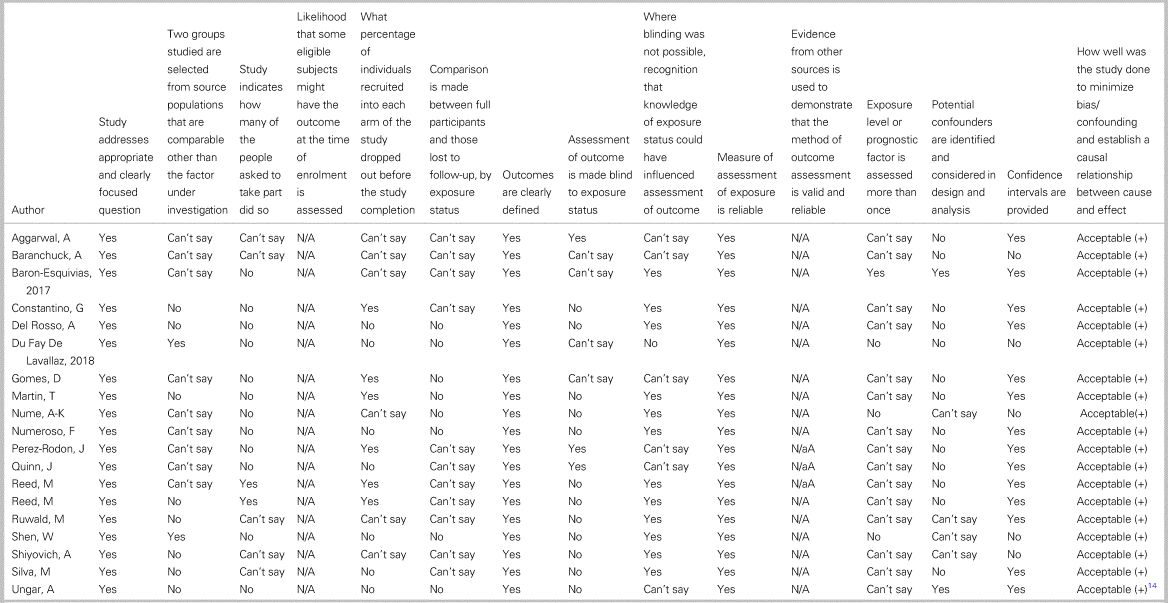
Acceptable (+) = Meets most criteria. Some flaw in the study with an associated risk of bias. Conclusion may change in light of further studies; Can't say = cannot say if the article meets criteria; N/A = not applicable; No = the article does not meet criteria; Yes = yes the article meets criteria.
DISCUSSION
Our systematic review for long-term outcomes among ED patients with syncope included 19 studies. We were able to conduct a meta-analysis for one year using a subset of articles and found that an important portion of patients, 7.0%, would experience death; approximately one in six patients would experience recurrence of syncope requiring hospitalization; and 6.0% of patients would have a device inserted for treatment of an arrhythmia related to syncope. A sensitivity analysis for outcomes between 31 and 365 days showed that still an important proportion, 1 in 20, would experience mortality. The proportion of patients who had device insertions for arrhythmias was lower (1%) beyond 30 days of the index syncope.
Short-term 0–30 day outcomes for ED patients with syncope are well reported. The results of our review showed that overall long-term all-cause mortality for patients with syncope was 7.0%. Mortality after 30 days was still high at 5.0%. Solbiati et al. previously reported an 8.4% one-year mortality in their systematic review.Reference Solbiati, Casazza and Dipaola38 However, this review includes both patients with syncope and syncope mimics such as seizures. It is evident that ED patients with syncope have a risk of mortality even after surviving the short-term period subsequent to their syncopal episode. Moreover, several studies with follow-up exceeding one year report a large rate of mortality of up to 21.0% within four years of the index episode. It is pertinent that ED physicians, as well as other syncope specialists and general practitioners, are aware of this when deciding investigations, management, and follow-up for these patients. No previous studies have compared the mortality rates among matched patients with and without syncope. Among those presenting to the ED with syncope, 16.0% would have at least one other episode of syncope that requires hospitalization within one year. Such recurrences and hospitalizations have a profound impact on the quality of life of these patients. Patients with recurrent syncope have a poor quality of life, and the negative effect on life quality is proportional to the number of episodes of syncope.Reference Brignole, Moya and de Lange39 Appropriate identification of these patients, education, and further management by syncope specialists can improve their quality of life.Reference Brignole, Moya and de Lange1
We found that the probability of pacemaker insertion within one year would be 6.0% among patients presenting to the ED with syncope. Our sensitivity analysis showed that most of these devices are inserted within the first 30 days, and none of the studies reported ICD insertion in the long term. A recent study reported that a large proportion of arrhythmias was identified within the first hours immediately after syncope, and 91.7% were identified within two weeks of syncope among those at risk.Reference Thiruganasambandamoorthy, Rowe and Sivilotti40 However, 5.0% of ED patients with syncope would experience mortality beyond 30 days that could be because of an occult life-threatening arrhythmia.
In our literature search, the two studies that did report arrhythmias had varying definitions for this outcome. Moreover, some studies published data on device insertion; however, they did not publish data on specific arrhythmias or the number of arrhythmias that were different from the number of devices inserted. It is likely that if an arrhythmia resulted in a device being inserted, then this was counted as a device insertion outcome rather than an arrhythmia. In general, studies were unclear reporting the arrhythmias and device insertions for treatment of arrhythmias. Future large-scale studies are needed to evaluate the incidence of arrhythmias in the longer term and risk factors for such arrhythmias.
Given that 1 in 14 patients will die and one in six will require hospitalization for recurrent syncope in the following year, significant morbidity and mortality exists for these patients. Currently, there are no studies that reliably risk-stratify patients with syncope for long-term outcomes. Future studies are needed to guide physicians for better long-term management of patients presenting with syncope.
LIMITATIONS
There was a large degree of heterogeneity among the studies included in this review. There were significant differences in study design and follow-up method; the age of patients included in the studies were widely varied with mean age range from 56.5 years to 71 years; and patient comorbidities and causes of syncope were also variable among studies. Moreover, while all studies examined mortality, assessment of other long-term outcomes was highly variable, and very few studies reported all potential long-term outcomes. Although 19 articles were included in the final systematic review, fewer studies were included in the meta-analysis.
We limited our meta-analysis to one-year outcomes, as this was the most feasible based on the included studies and would be clinically pertinent. Hence, we had to exclude articles with the highest mortality rates: 21.0% reported by Ruwald et al. at a 30-month follow-up and 16.7% reported by Aggarwal et al. at a 4.2-year follow-up. Such high mortality rates underline the clinical importance of syncope.
It was difficult to find studies that capture significant arrhythmia as an outcome. Moreover, those did have significantly different definitions of arrhythmia. For this reason, we could not do any pooled analysis for arrhythmia outcomes.
To our knowledge, the SIGN 50 tool was the most appropriate tool to use for quality assessment of single-arm retrospective and prospective studies. We did not use two questions in the second half of the tool, as these were used to assess quality of guidelines.
CONCLUSION
ED patients with syncope remain at risk for mortality and morbidity in the long term. Approximately one in six patients with syncope will be re-admitted to the hospital for investigations within one year of syncope, and one in fourteen will die. Further research should focus on how to identify patients at risk for long-term adverse outcomes and management to improve their outcomes including quality of life.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.393.
Competing interests
None declared.
Funding
None.











