CLINICIAN'S CAPSULE
What is known about the topic?
A small number of randomized controlled trials (RCTs) have been conducted involving emergency department (ED)-based violence intervention programs, but multiple methodological issues have been identified.
What did this study ask?
Is it feasible to complete an RCT on an ED-based violence intervention program, and what is the efficacy of this program?
What did this study find?
This study demonstrated the feasibility and safety of an RCT and a large magnitude of benefit for the EDVIP program.
Why does this study matter to clinicians?
ED-based interventions addressing the issues associated with violence may result in reduced repeat violent injury among youth.
INTRODUCTION
Violence perpetrated by another person in a non-familial, non-intimate relationship is the most common injury type for youth (aged 12–24) to visit an emergency department (ED) and the leading cause of hospitalization among males aged 15 to 24 years.Reference Macpherson, Schull, Manuel, Cernat, Redelmeier and Injuries1,2 Between 2012 and 2016 in Canada, 21% of homicide victims and 37% of those accused were youth.3 For every youth homicide, there are 16 admissions to the hospital for violence-related injuries and 116 ED visits.4 Violence-related injury is costly; in 2010, Canada spent $1.14 billion on violence-related injury ($541 million direct, $602 million indirect).5 Beyond the millions of dollars spent, huge emotional cost to individuals, their family, communities, and society occur. Injury is described as a chronic, recurring disease.Reference Sims, Bivins and Obeid6 In Winnipeg, MB, 20% of youth with a violence-related injury returned to the same ED within 12 months with a repeat violence-related injury.Reference Parveen and Snider7 The current standard of care is to treat the physical injury and discharge them from the ED without counselling.
The ED is an ideal setting to link an injured youth to a mentor as they are in a reflective and receptive state of mind.Reference Johnson, Bradshaw and Wright8 Hospital-based violence intervention programs are considered best practice; however, given their cost and insufficient evidence from large controlled trials, uncertainty exists. If this model is not efficacious, then public money should be spent elsewhere to decrease the burden of violence. The primary objective of this study was to determine the feasibility and safety of performing a large randomized control trial (RCT) to test the effectiveness of an ED violence intervention program (EDVIP) that connects an injured youth at the time of injury with a support worker to reduce repeat violence-related injury. The secondary objectives were to determine the efficacy and effectiveness of EDVIP on repeat violence-related injury, justice, and education systems interactions and the impact on ED length of stay (LOS) to optimize the intervention.
METHODS
Study design and timeline
The study was a pilot RCT with recruitment from November 2013 to November 2014. Participants were identified using an automated email based on criteria entered into the ED Information System (EDIS) at triage and then screened and recruited by a research assistant from 08:00 to 24:00 or the overnight support worker. The RA then logged onto a central randomization website (randomize.net), and randomization with block sizes of four and six occurred. Participants randomized to the control group were offered the intervention one year after enrolment. While allocation was unblinded to those delivering the intervention, all research personnel later involved in collecting outcomes were blinded to allocation. Collection of outcomes occurred in 2016, with justice data becoming available in 2018. This study was approved by the University of Manitoba Health Research Ethics Board.
Study setting
The study setting was an inner-city academic ED in Winnipeg, MB.
Population
Inclusion criteria are youth (aged 14–24) presenting to the ED with a violence-related injury. Exclusions include if the youth was unable to consent because of language or pre-existing severe cognitive deficits; transfer >1 hour from hospital; and presentation due to intimate partner violence, sexual assault, child maltreatment, or self-harm.
Intervention
The EDVIP intervention is a wraparound care program that uses the Circle of Courage strengths-based Indigenous framework.Reference Brendtro, Vanbockern and Brokenleg9 The program, delivered by support workers who have lived experience with violence, was founded on an integrated knowledge translation approach with diverse community members, youth previously affected by violence, clinicians, and researchers. The development, protocol, and intervention are described in previous manuscripts.Reference Snider, Woodward and Mordoch10,Reference Snider, Jiang, Logsetty, Strome and Klassen11
Support workers are notified about a potential participant when they are registered in the ED. As soon as the youth is able to participate, the support worker supports the youth and, if present, their family while the patient is still in the ED or hospital. Youth are asked to identify factors that put them at risk for violence (e.g., unsafe housing, addictions, and mental health). Discussions of protective factors such as education, employment, and cultural programs occur. Within the first 72 hours after discharge, the youth visits the EDVIP office to meet with the support worker and social worker to complete formal assessments assessing future violence risk and to set goals. Support workers are available to youth 24/7 for the following year by phone, text, and in person. Initially, they met with the youth several times weekly and, then, slowly taper down to a few times monthly by the end of the year. Support workers worked closely with community partners linking youth with organizations that could help them reach their goals.
Primary outcome measures
Feasibility was determined by measuring recruitment, fidelity, adherence, and safety. An objective for recruitment was set to determine the duration required for a large effectiveness trial. Data on numbers screened, eligible, and consenting were gathered. To assess fidelity, initially, a common number of goal contacts was developed a priori to start the intervention; however, it became clear that the youth required different care levels based on their risk that fluctuates, and the fidelity plan was adapted during the study. Eventually, the Violence Risk Scale was used to determine low, medium, or high risk for violence and an associated goal for number of contacts determined with a fidelity measure being achievement of 85% of these contacts.Reference Stockdale, Olver and Wong12 Participant adherence refers to both the receipt of the intervention and enacting on the intervention (e.g., accessing resources). The initially planned inventory, designed to measure the strength of the bond between the support worker and participant and the agreement on tasks and goals set, was poorly understood by the youth.Reference Horvath and Greenberg13 Adherence outcome was revised to collect data on youth actions related to their goals. Gang-involved youth are at high risk of retaliatory violence. It was essential to ensure participants not experience increased harm as part of the intervention. A mid-study review and all serious adverse events were reviewed with the Data and Safety Monitoring Board (DSMB).
Secondary outcome measures
Repeat violence-related injury, visits for substance use, and mental health were measured using a combination of administrative data and chart review. A list of all visits by each participant to any of the seven Winnipeg EDs in one year post-enrolment into the study was provided by the Winnipeg Health Region based on provincial health information numbers (PHIN). Subsequently, a chart review using a standard chart abstraction form was performed by trained nurse (RN) chart abstractors to determine the nature of the visit. Data from the EDIS were used to determine the LOS of the initial visit. Given the concerning wait times and focus on improving patient flow in Canadian EDs, it was important to understand this program's impact. Mean times are reported.
Changes in interactions with the justice system were determined by linking the participant's PHIN to the Prosecutions Information and Scheduling System at the Manitoba Centre for Health Policy (MCHP). The umber of charges laid in the year prior to the index injury and in the year post-index injury was collected for each group and, then, compared and reported as an odds ratio (OR). Individual PHINs were linked to the Enrollment, Marks, and Assessments database at MCHP. A binary measurement of “actively enrolled in school” or “already completed grade 12” was determined for the year prior to injury and the year after injury. Positive engagement was defined as new enrolment in the year post-injury. Absolute differences are reported.
Given the importance of understanding whether the program helped the participants, an efficacy analysis occurred. Participants were considered to have participated in EDVIP if they met with their support worker at any time beyond the initial meeting. Effectiveness analysis occurred according to randomization.
Data analyses
The analyses were carried out using SAS 9.4 (SAS Institute, Cary, NC). All p values were two tailed, and a p value of <0.05 was regarded as significant. For most continuous variables, mean and standard deviation were summarized by group (intervention and waitlist). Canadian Triage and Acuity Scale (CTAS) were not normally distributed and, therefore, summarized in the descriptive analyses using the median and range. Categorical variables and ordinal variables were summarized using number (percent) in various categories. For continuous variables with a normal distribution (e.g., age), mean and standard deviation are presented, and an independent t-test was used to compare two groups; if not normally distributed, variables are summarized using median and range, and the Mann-Whitney U test used. Categorical variables are summarized using the number (percent) in various categories, a chi-square or Fisher's exact test was used, as appropriate. For count outcomes, a generalized linear model with Poisson distribution was used to examine the group differences. A generalized linear mixed model with binomial distribution was conducted to examine the group difference in changes from one year before admission to one year after.
Sample size
The sample size was based on how many youths could be recruited to the study within one year.
RESULTS
In one year, 3,067 email alerts were received, and 92% were screened for eligibility. Of those, 451 (16%) were deemed eligible; 162 (36%) consented to a cohort study, but only 133 (82%) of those consented to future randomization into studies. Sixty-eight participants were randomized into EDVIP, and 65 were randomized to the waitlist control. Three of those randomized to EDVIP withdrew their consent while in the ED; therefore, only 65 youth are compared in the analysis. (Figure 1) There were no differences in baseline demographics between the two groups (Table 1).

Figure 1. Study flow.
Table 1. Baseline demographics and index visit characteristics

CI = confidence interval; CTAS = Canadian Triage and Acuity Scale; EDVIP = emergency department violence intervention program; EMS = emergency medical services; HSC = Health Sciences Centre; IQR = interquartile range; SD = standard deviation.
*If rows do not equal 100%, this is because of missing data.
Fifty-seven youth (88%) enrolled in the intervention attended their first follow-up appointment. There was one formal withdrawal after this initial meeting, and 5 (9%) youth did not participate after their initial meeting despite three or more attempts to contact them within the first month.
Further, 74% of participating youth were actively engaged (weekly contact) at six months and 57% at one year. All adverse events were reviewed with the DSMB. No deaths occurred during the study. The stopping rule of a significant (p < 0.05) increase in repeat violence-related injury was not met mid-study.
For the efficacy analysis, 51 youth were assumed to be participants, and 82 youth were assumed to be in the waitlist control group. While not powered to show a difference, an efficacy analysis of pilot RCT data demonstrated a large magnitude of benefit with EDVIP on: any repeat violence-related injury, number of repeat violence-related injury, education involvement, and justice involvement (Table 2). There was an absolute decrease of 10.4% in violence-related injury (relative decrease of 43.2%, p = 0.15). There was a decrease in the number of repeat violence-related injury between the group (EDVIP 1.14 ± 0.38 v. control 1.95 ± 1.99, p = 0.11). Of those who did have a repeat violence-related injury, injuries to those involved in EDVIP occurred sooner 194.9 ± 106.3 days vs. Control 309.4 ± 103.9 days (p-value = 0.02). Of those with a repeat violence-related injury, those in EDVIP were less likely to be injured by a weapon (28.6% v. 47.4%, respectively; p = 0.39). There was no difference in post-enrolment visits for substance use (p = 0.76) and mental health (p = 0.84). Further, 11.8% of EDVIP youth v. 7.6% of control (difference of 4.2%, p = 0.42) demonstrated positive education enrolment or graduation in the efficacy analysis. Youth enrolled in EDVIP stayed, on average, 59.5 minutes (15%) less (p = 0.21) than those not enrolled in EDVIP. If controlled for previous justice involvement, the efficacy analysis demonstrated an OR of 0.36 (0.07–1.77) for those enrolled in the EDVIP program (Table 3). There was no direction of benefit or harm for EDVIP if analyzed by randomization group.
Table 2. Efficacy analysis

CI = confidence interval; CTAS = Canadian Triage and Acuity Scale; EDVIP = emergency department violence intervention program; ED = emergency department; IQR = interquartile range; LOS = length of stay; SD = standard deviation.
*Only among those with repeat violence-related injury.
Table 3. Comparison for justice data (efficacy): Changes from one year before to one year after the index date
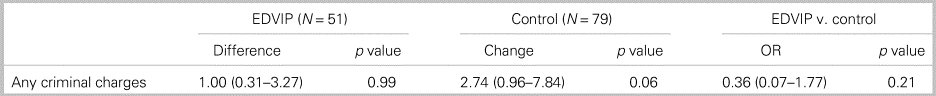
EDVIP = emergency department violence intervention program.
DISCUSSION
Interpretation of findings
This pilot study demonstrated the feasibility of implementing the EDVIP, a future effectiveness study, and potential efficacy. No safety concerns were demonstrated by the data or highlighted. Efficacy demonstrated a non-statistically significant but strong magnitude of benefit on any repeat violence-related injury, number of repeat violence-related injury, education, and justice involvement. There was no direction of benefit or harm when using an effectiveness analysis. Those enrolled in the EDVIP program had a trend toward earlier visits for repeat violence-related injury. This may indicate increased risk early in the program or increased comfort presenting to the ED. These data indicate that the protocol likely works and highlight future consideration of the difference between youth who drop out and those who stay and how the EDVIP intervention could better engage youth in the initial days post-injury. The lack of difference in post-enrolment visits associated with substance misuse and mental health are likely related to systemic issues that provide opportunity for direct entry through the ED to a detoxification program. This changed part way through the study, and the support workers regularly used this route to access addictions care. A new mental health centre associated with the ED opened during the study, and EDVIP youth commonly used this centre. With pressure on EDs to reduce wait times, it is positive to see that implementing a support worker model did not extend the LOS. A decrease in average LOS of 59.5 minutes (p = 0.21) demonstrated the potential benefit of using laypersons in a busy ED. EDVIP support workers ensure youth would have safe shelter on discharge, appropriate clothing, and food and likely helped to expedite discharge from the ED.
Comparison with previous studies
This study is one of a small number of RCTs examining the effect of hospital-based violence intervention programs. Previous studies showed variable benefit but were limited by sample size, recollection bias for self-reported follow-up, selection bias for high risk repeat injuries, and high loss of follow-up.Reference Aboutanos, Jordan and Cohen14–Reference Zun, Downey and Rosen17 The previous studies and this study determined the effect of a hospital-based violence intervention program on youth injured by violence on repeat violence-related injury; however, the ages, intervention design, duration of program, and outcome measures differed in all cases.
Strengths and limitations
Given the high loss of follow-up in self-reported outcomes in previous studies, our study demonstrates the benefit of administrative data to follow patients allowing for near 100% follow-up within a wide geographic location. It is a limitation that the pilot study allowed for slight variations in protocol as the EDVIP team learned how to implement and evaluate the intervention. However, this would allow for improved measurements in a large effectiveness trial. Given only 36% of the eligible youth consented to a cohort study and only 82% of those consented to randomization, selection bias might exist. By its nature, the intervention required participants to be ready for making changes in their lives. While randomization results in this selection bias being decreased, any conclusions should be limited to those who are motivated to change. Attrition bias is evident in any efficacy analysis. Given the lack of benefit in the intention-to-treat analysis, it is important to optimize the intervention to ensure decreased attrition in future trials. Participants were recruited from an inner-city trauma centre in a mid-sized Canadian city and may not be generalizable to all locations; however, demographics and repeat violence-related injury rates in the control group are consistent with international estimates.
Clinical implications
This study demonstrates feasibility and safety and is one among only a few RCTs to report the efficacy of a hospital-based violence intervention program for youth on reducing injury recidivism. While not powered to demonstrate a difference, the study demonstrated that those who stayed in the program and participated >1 month had a decrease in incidence and number of repeat violence-related injury. This efficacy result has been of great interest to many policy makers locally, nationally, and, indeed, internationally. In fact, the positive directional benefit resulted in a loss of equipoise here in Winnipeg and resulted in the program being fully funded by the government (albeit currently on hold because of funding cuts).
Research implications
Behavioural RCTS in EDs are rare. This study demonstrated the feasibility and safety of conducting an RCT in a typically hard to reach population. The authors feel that a full RCT would, of course, be appropriate methodologically; however, this has become difficult in an environment in which equipoise was lost in both the community and, frankly, the front-line workers based on efficacy results.
CONCLUSIONS
The study demonstrated great promise for EDVIP programs. Future studies will better determine its effectiveness for this population.
Acknowledgements
We would like to thank Karen Cook, Justin Rivera, Rob Robinson, Linda Rost, Nathan Thomas, Leslie Spillett, Trevor Strome, and the late Floyd Wiebe for their involvement in developing the intervention and their support throughout the study.
Competing interests
Funding received from the Canadian Institutes of Health Research (FRN 130476), Children's Hospital Research Institute of Manitoba and Research Manitoba. No conflict of interests.








