Introduction
There are around 7000 different rare diseases worldwide (prevalence <1:2000). The majority of these conditions have a genetic origin and a chronic and often progressive course. Valid information about rare diseases is scarce, diagnostic processes are difficult, and treatment options limited (Kole & Faurisson, Reference Kole and Faurisson2009). On an individual level, the conditions cause constraints, psychological and interpersonal problems, and decreased quality of life (Cohen & Biesecker, Reference Cohen and Biesecker2010; von der Lippe, Diesen, & Feragen, Reference von der Lippe, Diesen and Feragen2017). In a cross-sectional online study we conducted including patients with different rare diseases, high percentages of patients showed increased depression and anxiety levels, assessed with standardized questionnaires (Uhlenbusch et al., Reference Uhlenbusch, Löwe, Härter, Schramm, Weiler-Normann and Depping2019). Comorbid mental diseases in addition to a chronic condition can worsen the course of the disease (Lichtman et al., Reference Lichtman, Froelicher, Blumenthal, Carney, Doering, Frasure-Smith and Sheps2014; Watkins et al., Reference Watkins, Koch, Sherwood, Blumenthal, Davidson, O'Connor and Sketch2013) and add to reduced quality of life (Cruz, de Almeida Fleck, & Polanczyk, Reference Cruz, de Almeida Fleck and Polanczyk2010; Müller-Tasch et al., Reference Müller-Tasch, Peters-Klimm, Schellberg, Holzapfel, Barth, Jünger and Herzog2007). Since the majority of rare diseases are not curable, maintaining and enhancing quality of life is crucial.
The prevalence of affective and anxiety disorders in patients with rare diseases is unclear. Studies on psychopathology in specific rare diseases such as amyotrophic lateral sclerosis (ALS) (Chen et al., Reference Chen, Guo, Zheng, Wei, Song, Cao and Shang2015) or systemic sclerosis (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011) exist but no study has systematically synthesized this evidence across rare diseases. Systematically summarizing evidence can help to better understand the burden of living with a rare disease and enables deriving implications for comprehensive patient care. This may be particularly relevant in the field of rare diseases, where the high number of different rare diseases and the rarity of each condition challenges research and healthcare (Eidt et al., Reference Eidt, Frank, Reimann, Wagner, Mittendorf and Graf von der Schulenburg2009). The objective of this systematic review was to examine the prevalence of clinically relevant affective and anxiety disorders in patients with different rare chronic diseases. Moreover, we aimed at identifying aspects associated with increased psychopathology.
Method
We performed a systematic review and meta-analysis following the PRISMA guidelines. We published a review protocol on PROSPERO (http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018106614).
Eligibility criteria
We included studies published in English or German with the primary aim of investigating the prevalence of affective and/or anxiety disorders, assessed with structured clinical interviews or clinical diagnoses. We included observational studies (cross-sectional studies, case-control studies, cohort studies) and excluded case studies, case series, randomized controlled trials, and grey literature. Included patients were adults with any rare chronic disease. If a study addressed children and adolescents, it was included if data for age-based subgroups were available. Rarity was defined as affecting less than one in 2000 individuals. We included diseases with a primarily genetic origin since we aimed at investigating chronic rather than acute conditions. Therefore, we excluded rare cancers, injuries, infections, complications after medical interventions and somatoform diseases. We further excluded studies assessing rare sub-forms of non-rare diseases (e.g. early-onset Parkinson disease) and gen-carriers without the clinical picture of the disease.
Search strategy
We discussed the search strategy with an independent librarian of the University of Hamburg beforehand. We systematically searched three electronic databases between May and June 2018: MEDLINE, PSYNDEX, PsycINFO. The search term included all rare diseases listed in the orpha.net registry of rare diseases [(RARE DISEASE) AND (DEPRESSION OR ANXIETY OR PSYCHOSOCIAL OR MENTAL HEALTH OR QUALITY OF LIFE OR PATIENT EXPERIENCES OR PSYCHOPATHOLOGY OR WELL-BEING)]. An excerpt of the search term is in the online Supplementary material. In addition, we hand-searched references and used the cited-by function for all articles meeting inclusion criteria. Last date of hand-search was 25 January 2020. We used Ovid for the database search and Endnote X7.3.1 to manage references during the screening process.
Study selection
We imported all studies detected during the database search into Endnote X7.3.1, where we screened for eligibility. During the initial screening process, one researcher assessed eligibility based on the titles, abstracts, and study types. Studies meeting any exclusion criteria were removed during the initial screening process. Potentially relevant studies or studies where eligibility remained unclear were further evaluated in the secondary screening. During the secondary screening process, two researches independently checked abstracts and full-texts. If full-texts were not available, we contacted corresponding authors. We documented all reasons for exclusion during the secondary screening. We discussed unclear cases and in case of disagreement, other co-authors were consulted.
Data extraction
We prepared a data extraction form based on the objectives of this review, which we piloted with a sample of studies and revised it until found adequate. We extracted the following data items: disease, sample size, study design, measures to assess psychopathology, comparison group (if applicable), frequency of current and lifetime major depressive disorder, current and lifetime affective disorders, current and lifetime anxiety disorders (assessed with clinical interview or clinical diagnoses), all reported correlates of depression and anxiety symptoms (assessed with clinical interviews as well as standardized questionnaires, if these were used additionally). Two researchers (NU, JS) independently read all studies meeting inclusion criteria, extracted relevant data, and compared the extracted information.
Data analysis
Quality and risk assessment
We assessed the quality of individual studies using the STROBE checklist for reporting observational studies (https://www.strobe-statement.org/index.php?id=available-checklists). Based on the number of items in the checklist, a maximum of 34 points (sub items included) could be reached. If information was not reported, we rated it as not fulfilled. Some items are only applicable for certain study designs. We calculated the percentage of fulfilled items in relation to the number of applicable items for the study design with a possible range from 0% to 100%. Two researchers independently rated the studies and discussed disparities until reaching agreement. In vague cases, a third researcher was consulted. We calculated interrater reliability using κ.
Meta-analysis
Based on the outcomes assessed in each study, the prevalence rate of clinically diagnosed affective and anxiety disorders was calculated as the reported number of subjects with a clinical diagnosis divided by the total number of subjects of the study (one-arm study) and the considered study arm (two-arm study), respectively. The prevalence rates were transformed with a logit transformation and pooled using a random intercept logistic regression model. Ninety-five percent confidence intervals for the individual study results were calculated using Clopper-Pearson intervals. The results of the meta-analysis are presented using forest plots. Overall heterogeneity among studies was assessed using the I 2 and τ 2 statistics and heterogeneity tests. The reported p values are one-sided; p values less than 0.025 are considered statistically significant. Funnel plots were created to evaluate reporting bias. In a sensitivity analysis, the pooled estimates were stratified by the quality of the included studies distinguishing between low (<40%) and high quality (⩾40%). All analyses and graphs were generated with the statistical software R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria). The meta-analysis was performed using the command metaprop of the R-package meta (version 4.11–0).
Results
Search results and characteristics of included studies
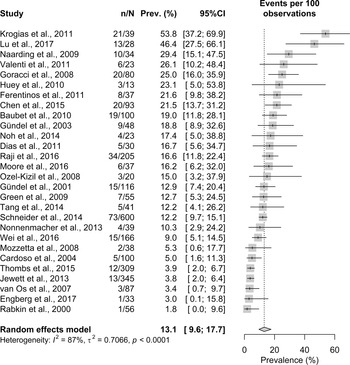
We identified 41 146 records by database search and 671 studies by hand-search. After removing duplicates, we screened 34 402 titles/abstracts in the initial screening and full texts of 531 studies during the secondary screening. Due to the high number of potentially relevant studies, we excluded studies published before the year 2000 during the secondary screening. Finally, we included 39 studies in the qualitative analysis and 37 in the quantitative analysis (flowchart in Fig. 1). Sample sizes ranged between N = 13 and N = 1752. In total, N = 5951 patients with 24 different rare diseases were included (a list of all diseases and their prevalence rates is in online Supplementary Table S1). The largest group were patients with ALS (7 studies, N = 2156 patients). Thirty-four studies had a cross-sectional design, two studies were cohort studies, and one study was a combined case-control study and cohort study. Two studies had a longitudinal design with baseline and follow-up assessments. In these cases, we used the baseline data. Twenty-two studies assessed both affective disorders (or only MDD) and anxiety disorders, 17 studies only affective disorders (or only MDD), and no study examined only anxiety disorders. The quality of included studies ranged between 29.41% and 91.18% with a mean value of 57.91% (s.d. = 14.74%). Interrater reliability was good with κ = 0.74. Online Supplementary Table S2 provides an overview of the characteristics and main results of all included studies. The final quality rating for each study is in online Supplementary Table S3.
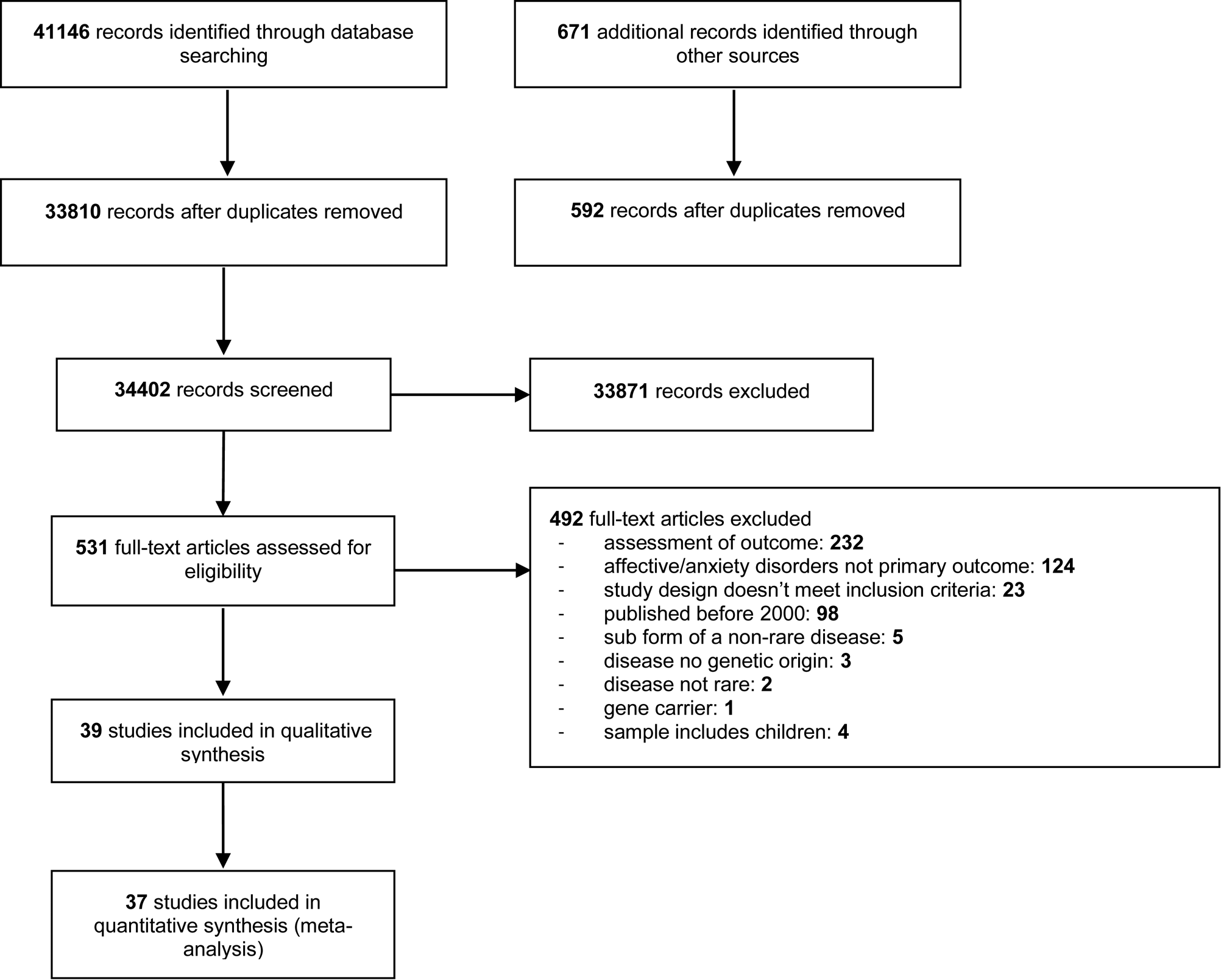
Fig. 1. Flowchart representing search results and selection process. Notes. Inclusion criteria were applied in the following order: (1) primary outcome, (2) assessment of outcome, (3) study design, (4) sample characteristics.
Frequency of affective disorders
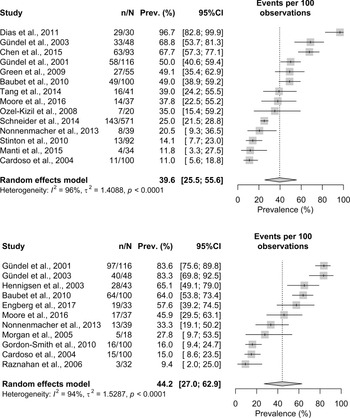
Of the 39 studies included in the qualitative analysis, all studies assessed affective disorders (or only MDD), with widely ranging frequency rates. The prevalence of current MDD ranged between 2.0% (Rabkin, Wagner, & Del Bene, Reference Rabkin, Wagner and Del Bene2000) and 53.8% (Krogias et al., Reference Krogias, Strassburger, Eyding, Gold, Norra, Juckel and Ninphius2011). The pooled prevalence estimate was 13.1% (95%CI 9.6–17.7%) across 28 studies with significant heterogeneity (I 2 = 87%, p < 0.0001). Visual inspection of the funnel plot showed no indications of reporting bias across studies. A sensitivity analysis excluding three studies with a quality of <40% revealed a pooled prevalence of 13.3% (95% CI 9.5–18.2%). The prevalence for lifetime MDD ranged between 11.1% (Morgan, Murphy, Lacey, & Conway, Reference Morgan, Murphy, Lacey and Conway2005) and 73.9% (Valenti et al., Reference Valenti, Pescini, Antonini, Castellini, Poggesi, Bianchi and Pantoni2011). The pooled prevalence estimate was 39.3% (95% CI 31.7–47.4%) across 15 studies. Heterogeneity was significant with I 2 = 84% (p < 0.0001) and the funnel plot showed no asymmetry. After excluding two studies with a quality of <40%, the pooled prevalence was 40.2% (95% CI 32.7–48.3%). The forest plots for current and lifetime MDD are in Figs 2 and 3. All forest plots showing the sensitivity analyses and all funnel plots are in the online Supplementary material.
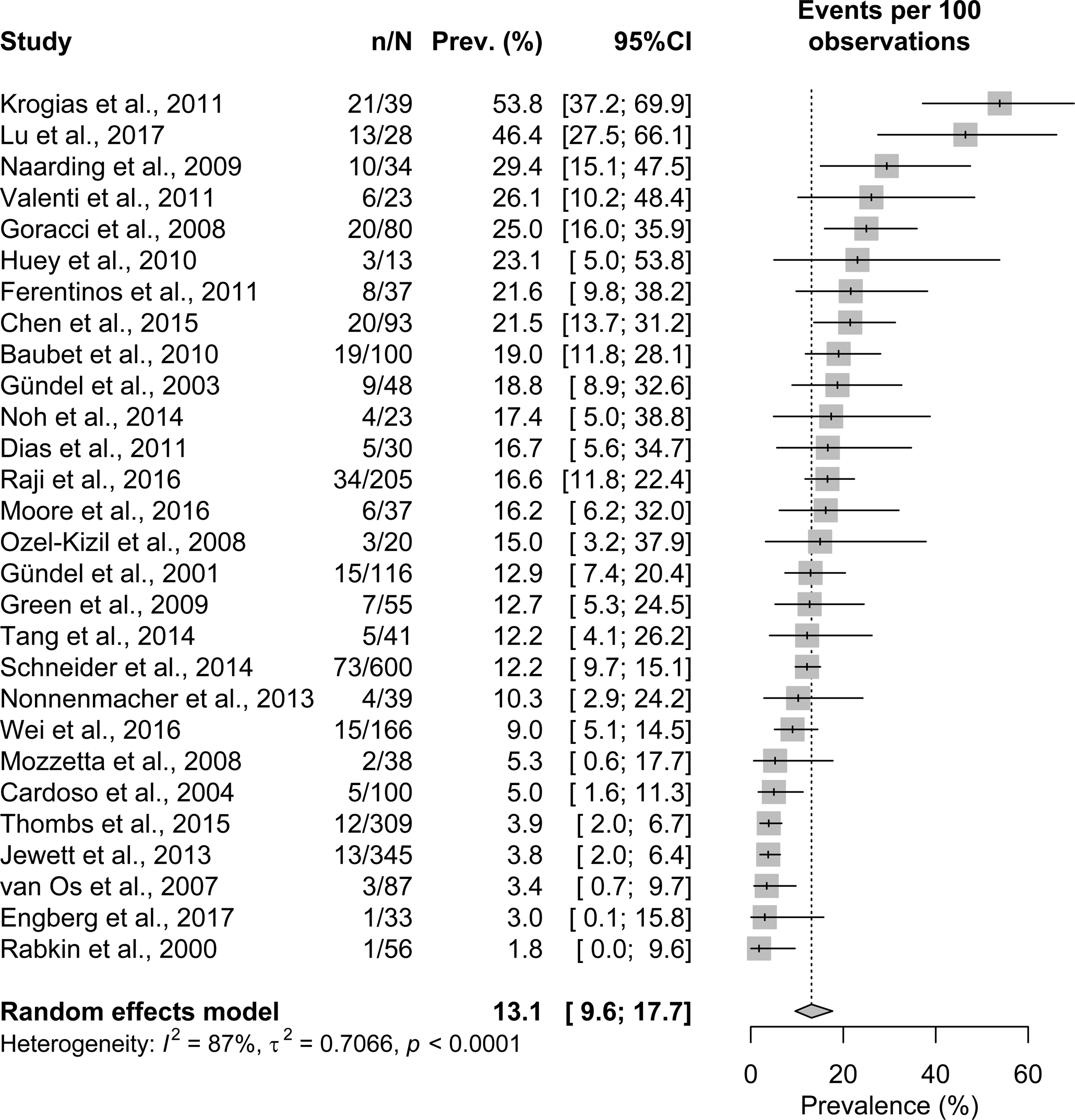
Fig. 2. Forest plots with prevalence rates of original studies and pooled prevalence estimates (with 95% CI) for current major depressive disorder. Notes. n = affected cases, N = sample size; Prev. = prevalence.
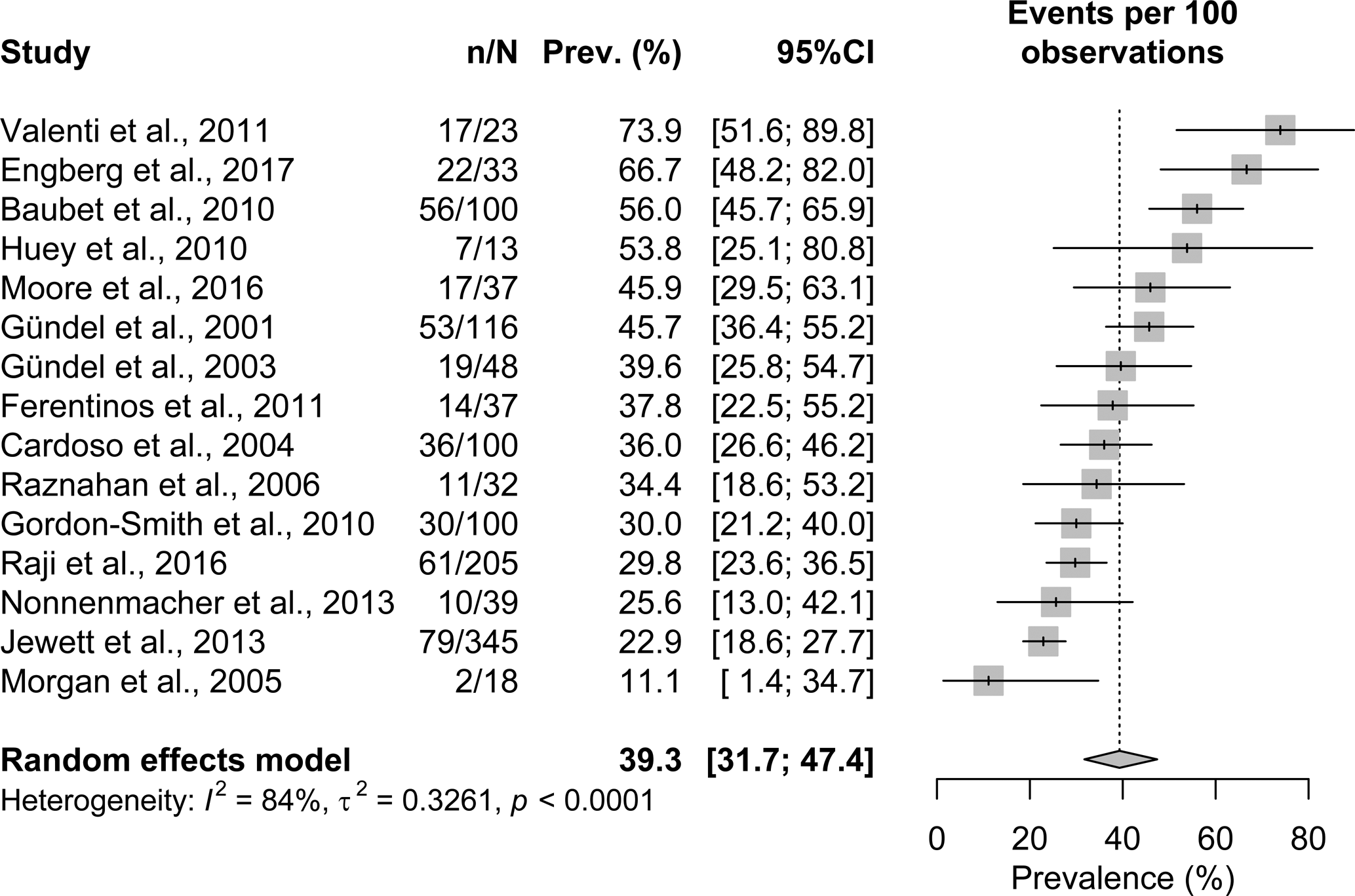
Fig. 3. Forest plots with prevalence rates of original studies and pooled prevalence estimates (with 95% CI) for lifetime major depressive disorder. Notes. n = affected cases, N = sample size; Prev. = prevalence.
The frequency of any affective disorder ranged between 5.6% (Stinton, Elison, & Howlin, Reference Stinton, Elison and Howlin2010) and 57.0% (Chen et al., Reference Chen, Guo, Zheng, Wei, Song, Cao and Shang2015) for current diagnoses. The pooled prevalence estimate for any current affective disorder was 21.2% (95% CI 15.4–28.6) across 17 studies with significant heterogeneity (I 2 = 90%, p < 0.0001). The funnel plot indicated no reporting bias across studies. A sensitivity analysis excluding two studies with a quality of <40% revealed a pooled prevalence of 18.8% (95% CI 13.8–25.2%). The prevalence of any lifetime affective disorder ranged between 11.6% (Henningsen & Meinck, Reference Henningsen and Meinck2003) and 72.7% (Engberg et al., Reference Engberg, Strandqvist, Nordenstrom, Butwicka, Nordenskjold, Hirschberg and Frisen2017) with a pooled prevalence of 46.1% (95% CI 35.8–56.8%) across 10 studies. The model showed significant heterogeneity (I 2 = 90%, p < 0.0001). Visual inspection of the funnel plot showed no evidence of reporting bias. No sensitivity analysis was performed since all studies had a quality of >40%. Figure 4 shows forest plots for current and lifetime affective disorders.
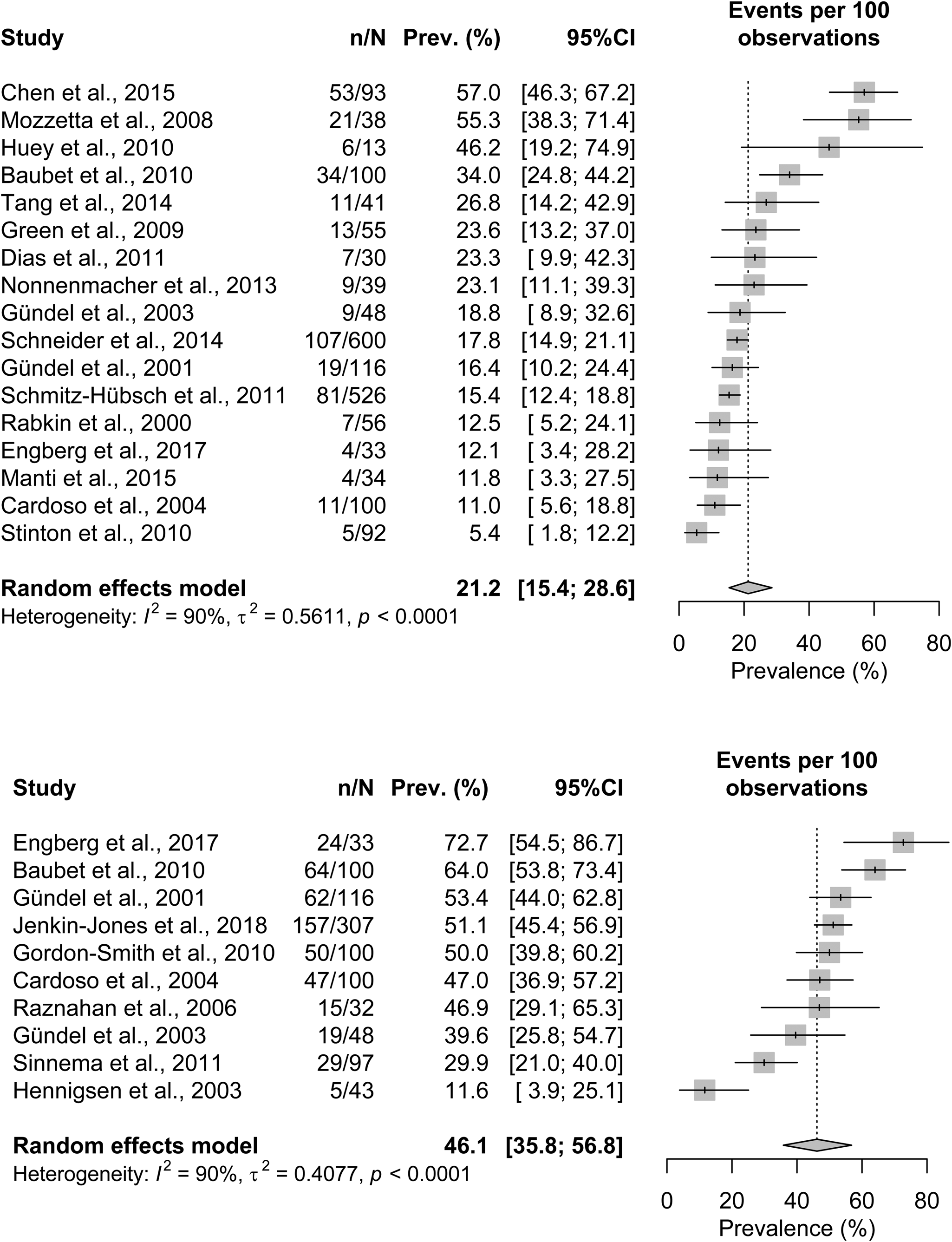
Fig. 4. Forest plots with prevalence rates of original studies and pooled prevalence estimates (with 95% CI) for current and lifetime affective disorder. Notes. n = affected cases, N = sample size; Prev. = prevalence.
Frequency of anxiety disorders
Of the 39 studies included in the qualitative analysis, 22 studies assessed anxiety disorders. The frequency for any current anxiety disorder ranged between 11.0% (Cardoso et al., Reference Cardoso, Daly, Haq, Hanton, Rubinow, Bondy and Schmidt2004) and 96.7% (Dias et al., Reference Dias, Kummer, Doyle, Harsanyi, Cardoso, Fontenelle and Teixeira2011) with a pooled prevalence estimate of 39.6% (95% CI 25.5–55.6%) across 14 studies. Heterogeneity was significant with I 2 = 96% (p < 0.0001) and the funnel plot showed no asymmetry. A sensitivity analysis excluding one study with a quality of <40% revealed a pooled prevalence of 40.0% (95% CI 24.9–57.3%). The prevalence range for lifetime anxiety disorders was 9.4% (Raznahan, Joinson, O'Callaghan, Osborne, & Bolton, Reference Raznahan, Joinson, O'Callaghan, Osborne and Bolton2006) to 83.6% (Gündel, Wolf, Xidara, Busch, & Ceballos-Baumann, Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001). One study (Mozzetta et al., Reference Mozzetta, Antinone, Alfani, Neri, Foglio Bonda, Pasquini and Picardi2008) assessed only generalized anxiety disorders and reported that 25.0% had a current diagnosis. Another study (Huey, Koppel, Armstrong, Grafman, & Floeter, Reference Huey, Koppel, Armstrong, Grafman and Floeter2010) investigated only phobia and reported a prevalence of 15.4% both for current and lifetime phobic disorder. These studies were not included in the meta-analysis. The pooled prevalence rate for the remaining studies was 44.2% (95% CI 27.0–62.9%) across 11 studies with significant heterogeneity (I 2 = 94%, p < 0.0001). Visual inspection of the funnel plot indicated no significant reporting bias. One study with a quality of <40% was excluded for the sensitivity analysis, which revealed a pooled prevalence of 45.9% (95% CI 27.3–65.8%). Figure 5 shows forest plots of the included studies and the overall effect estimates for current and lifetime anxiety disorders.
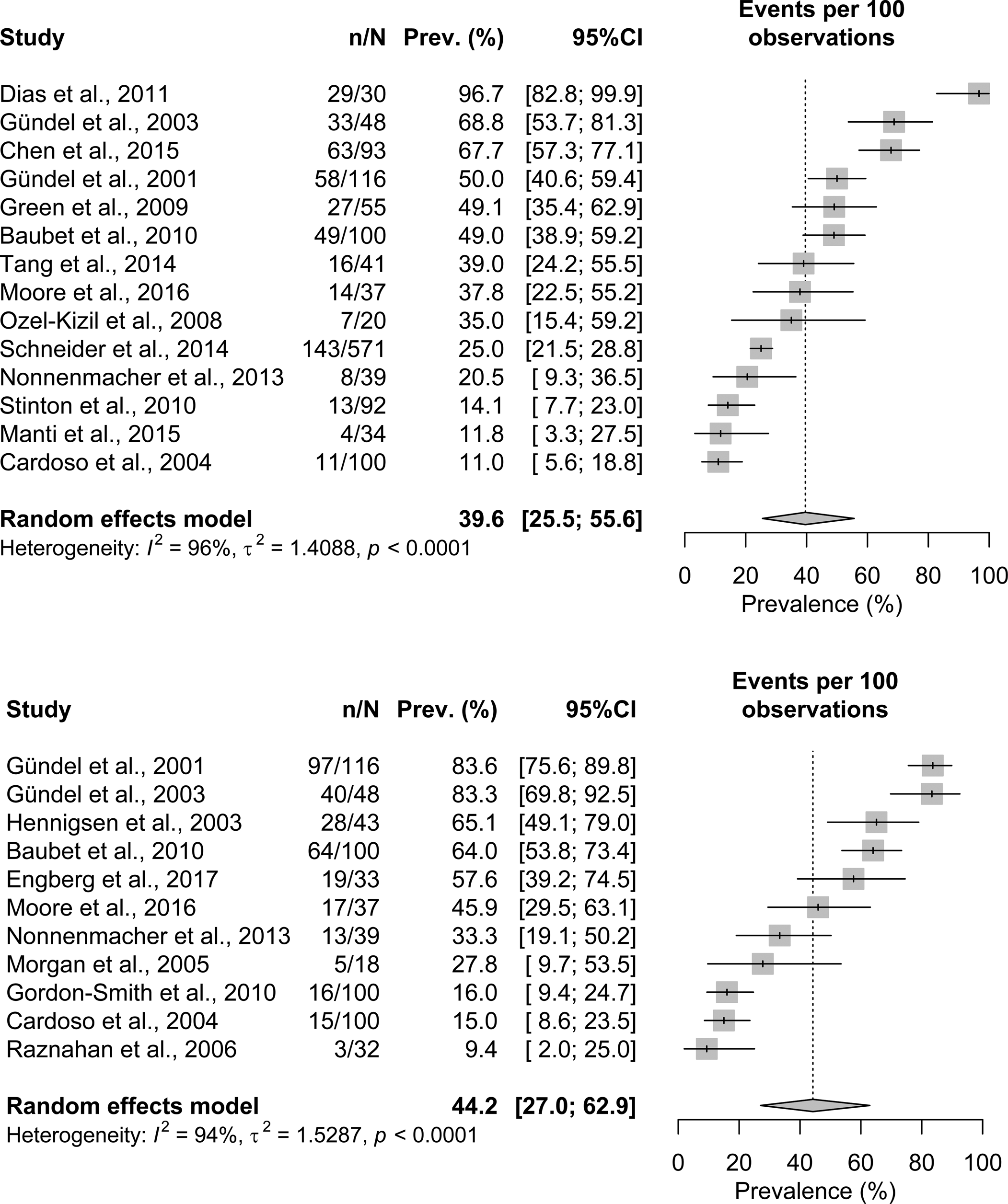
Fig. 5. Forest plots with prevalence rates of original studies and pooled prevalence estimates (with 95% CI) for current and lifetime anxiety disorder. Notes. n = affected cases, N = sample size; Prev. = prevalence.
Comparisons with control groups
In 15 studies, the frequency of affective and anxiety disorders was compared with a control group (online Supplementary Table S2). All eight studies reporting comparisons with population-based samples found significant differences in terms of a higher psychopathological burden of patients with rare diseases (Engberg et al., Reference Engberg, Strandqvist, Nordenstrom, Butwicka, Nordenskjold, Hirschberg and Frisen2017; Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001, Reference Gündel, Wolf, Xidara, Busch, Ladwig, Jacobi and Ceballos-Baumann2003; Hedgeman et al., Reference Hedgeman, Ulrichsen, Carter, Kreher, Malobisky, Braun and Olsen2017; Lu et al., Reference Lu, Duan, Zuo, Xu, Zhang, Li and Zhang2017; Manti et al., Reference Manti, Nardecchia, Chiarotti, Carducci, Carducci and Leuzzi2016; Moore et al., Reference Moore, Methley, Pollard, Mutch, Hamid, Elsone and Jacob2016; Roos et al., Reference Roos, Mariosa, Ingre, Lundholm, Wirdefeldt, Roos and Fang2016). In two studies (Chen et al., Reference Chen, Guo, Zheng, Wei, Song, Cao and Shang2015; Rabkin et al., Reference Rabkin, Wagner and Del Bene2000), authors compared patients with their caregivers and one reported higher frequencies of both depressive and anxiety disorders in patients (Chen et al., Reference Chen, Guo, Zheng, Wei, Song, Cao and Shang2015). In four out of eight comparisons with patients with non-rare diseases, patients with rare diseases showed higher rates than controls (Gündel et al., Reference Gündel, Wolf, Xidara, Busch, Ladwig, Jacobi and Ceballos-Baumann2003; Huey et al., Reference Huey, Koppel, Armstrong, Grafman and Floeter2010; Jenkins-Jones et al., Reference Jenkins-Jones, Parviainen, Porter, Withe, Whitaker, Holden and Ross2018; Mozzetta et al., Reference Mozzetta, Antinone, Alfani, Neri, Foglio Bonda, Pasquini and Picardi2008), two studies found no differences (Engberg et al., Reference Engberg, Strandqvist, Nordenstrom, Butwicka, Nordenskjold, Hirschberg and Frisen2017; Ozel-Kizil, Akbostanci, Ozguven, & Atbasoglu, Reference Ozel-Kizil, Akbostanci, Ozguven and Atbasoglu2008), and in two studies, the authors reported higher frequencies in the comparison group (Dias et al., Reference Dias, Kummer, Doyle, Harsanyi, Cardoso, Fontenelle and Teixeira2011; Moore et al., Reference Moore, Methley, Pollard, Mutch, Hamid, Elsone and Jacob2016).
Correlates of psychopathology
Fifteen studies additionally investigated correlates of psychopathology. In one study, psychopathology was not related to any individual (e.g. age, IQ) or external (life events) variable (Stinton et al., Reference Stinton, Elison and Howlin2010). In all other studies, authors found different associations with various patient-related, disease-related, or psychological features, partly with contradictory results. A detailed presentation of the observed correlates for all studies is in online Supplementary Table S4. In the following, we describe only major trends.
Patient-related features
Where sex differences were detected, most studies reported an association between female sex and both depression (Nonnenmacher, Hammer, Lule, Hautzinger, & Kuebler, Reference Nonnenmacher, Hammer, Lule, Hautzinger and Kuebler2013; Schmitz-Hübsch et al., Reference Schmitz-Hübsch, Coudert, Tezenas du Montcel, Giunti, Labrum, Durr and Klockgether2011; Schneider et al., Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014) and anxiety (Green et al., Reference Green, Gothelf, Glaser, Debbane, Frisch, Kotler and Eliez2009; Schneider et al., Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014; Tang et al., Reference Tang, Yi, Calkins, Whinna, Kohler, Souders and Gur2014). In studies that found age-related differences, depression was mostly associated with older age (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011; Manti et al., Reference Manti, Nardecchia, Chiarotti, Carducci, Carducci and Leuzzi2016; Roos et al., Reference Roos, Mariosa, Ingre, Lundholm, Wirdefeldt, Roos and Fang2016; Schneider et al., Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014), while anxiety disorders occurred more frequently in younger individuals (Hedgeman et al., Reference Hedgeman, Ulrichsen, Carter, Kreher, Malobisky, Braun and Olsen2017; Manti et al., Reference Manti, Nardecchia, Chiarotti, Carducci, Carducci and Leuzzi2016; Ozel-Kizil et al., Reference Ozel-Kizil, Akbostanci, Ozguven and Atbasoglu2008; Schneider et al., Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014). Most studies found no association with other demographic variables or education (Jewett, Razykov, Hudson, Baron, & Thombs, Reference Jewett, Razykov, Hudson, Baron and Thombs2013; Manti et al., Reference Manti, Nardecchia, Chiarotti, Carducci, Carducci and Leuzzi2016; Roos et al., Reference Roos, Mariosa, Ingre, Lundholm, Wirdefeldt, Roos and Fang2016; Wei et al., Reference Wei, Zheng, Guo, Ou, Chen, Huang and Shang2016). Contrarily, two studies (Nonnenmacher et al., Reference Nonnenmacher, Hammer, Lule, Hautzinger and Kuebler2013; Raji, Lawani, & James, Reference Raji, Lawani and James2016) found that depression was associated with lower education, unemployment, and low income.
Disease-related and clinical features
The majority of studies examining the relation between clinical symptoms of the rare diseases and psychopathology found no associations (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011; Cardoso et al., Reference Cardoso, Daly, Haq, Hanton, Rubinow, Bondy and Schmidt2004; Chen et al., Reference Chen, Guo, Zheng, Wei, Song, Cao and Shang2015; Gordon-Smith et al., Reference Gordon-Smith, Jones, Burge, Munro, Tavadia and Craddock2010; Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001; Naarding, Janzing, Eling, van der Werf, & Kremer, Reference Naarding, Janzing, Eling, van der Werf and Kremer2009; van Os et al., Reference van Os, van den Broek, Mulder, ter Borg, Bruijn and van Buuren2007; Wei et al., Reference Wei, Zheng, Guo, Ou, Chen, Huang and Shang2016) or only with single symptoms (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011; Jewett et al., Reference Jewett, Razykov, Hudson, Baron and Thombs2013; Raznahan et al., Reference Raznahan, Joinson, O'Callaghan, Osborne and Bolton2006). Three studies reported an association between pain and depression or anxiety (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011; Rabkin et al., Reference Rabkin, Wagner and Del Bene2000; Raji et al., Reference Raji, Lawani and James2016). Illness duration showed no association with depression or anxiety in six studies (Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001; Henningsen & Meinck, Reference Henningsen and Meinck2003; Krogias et al., Reference Krogias, Strassburger, Eyding, Gold, Norra, Juckel and Ninphius2011; Lu et al., Reference Lu, Duan, Zuo, Xu, Zhang, Li and Zhang2017; Nonnenmacher et al., Reference Nonnenmacher, Hammer, Lule, Hautzinger and Kuebler2013; Wei et al., Reference Wei, Zheng, Guo, Ou, Chen, Huang and Shang2016), two studies found higher psychopathology early in the disease course or early after diagnosis for anxiety (Moore et al., Reference Moore, Methley, Pollard, Mutch, Hamid, Elsone and Jacob2016) and affective disorders (Roos et al., Reference Roos, Mariosa, Ingre, Lundholm, Wirdefeldt, Roos and Fang2016). One study found a relation between longer disease duration and younger age of onset and depression (Schmitz-Hübsch et al., Reference Schmitz-Hübsch, Coudert, Tezenas du Montcel, Giunti, Labrum, Durr and Klockgether2011). Another study found no association with age of onset (Wei et al., Reference Wei, Zheng, Guo, Ou, Chen, Huang and Shang2016). A variety of studies found associations between depression and different neurological features and/or cognitive abilities (Krogias et al., Reference Krogias, Strassburger, Eyding, Gold, Norra, Juckel and Ninphius2011; Lu et al., Reference Lu, Duan, Zuo, Xu, Zhang, Li and Zhang2017; Moore et al., Reference Moore, Methley, Pollard, Mutch, Hamid, Elsone and Jacob2016; Noh et al., Reference Noh, Chung, Kim, Kang, Lim, Kwon and Kim2014; Schmitz-Hübsch et al., Reference Schmitz-Hübsch, Coudert, Tezenas du Montcel, Giunti, Labrum, Durr and Klockgether2011; Valenti et al., Reference Valenti, Pescini, Antonini, Castellini, Poggesi, Bianchi and Pantoni2011; van Os et al., Reference van Os, van den Broek, Mulder, ter Borg, Bruijn and van Buuren2007). Depression was further associated with decreased physical functioning in two studies (Rabkin et al., Reference Rabkin, Wagner and Del Bene2000; Wei et al., Reference Wei, Zheng, Guo, Ou, Chen, Huang and Shang2016), while three studies found no association (Lu et al., Reference Lu, Duan, Zuo, Xu, Zhang, Li and Zhang2017; Naarding et al., Reference Naarding, Janzing, Eling, van der Werf and Kremer2009; Nonnenmacher et al., Reference Nonnenmacher, Hammer, Lule, Hautzinger and Kuebler2013).
Psychosocial features
Few studies examined psychological features such as illness perceptions. Gündel et al. (Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001) observed that psychological variables explained depression and anxiety better than clinical features. Depressive coping (instead of, for instance, problem-focused coping) was identified as a strong predictor of depression and anxiety (Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001, Reference Gündel, Wolf, Xidara, Busch, Ladwig, Jacobi and Ceballos-Baumann2003). Depression and/or anxiety were further associated with reduced quality of life and poorer social functioning (Baubet et al., Reference Baubet, Ranque, Taieb, Berezne, Bricou, Mehallel and Mouthon2011), less enjoyment and satisfaction in different life areas (Goracci et al., Reference Goracci, Fagiolini, Martinucci, Calossi, Rossi, Santomauro and Castrogiovanni2008; Rabkin et al., Reference Rabkin, Wagner and Del Bene2000), and more psychological and physical distress (Rabkin et al., Reference Rabkin, Wagner and Del Bene2000). In patients with spasmodic torticollis, the extent of body image dissatisfaction was a strong predictor for the diagnosis of social phobia (Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001). One study found no association between depression and meaning of health but a negative correlation between depression and the number of perceived positive amplifiers in the patient's life (Nonnenmacher et al., Reference Nonnenmacher, Hammer, Lule, Hautzinger and Kuebler2013).
Discussion
This is the first systematic review and meta-analysis on affective and anxiety disorders in patients with different rare chronic diseases. Prevalence rates ranged widely between studies, with pooled prevalence estimates of up to 46.1%, for instance for lifetime affective disorders. Heterogeneity between studies was high, which is reflected in large confidence intervals of the pooled prevalence rates. The large variation between diseases may reflect the clinical heterogeneity of different rare diseases. However, even among studies investigating the same disease, results varied widely (e.g. current anxiety disorder in ALS 20.5–67.7%). Other methodological sources of heterogeneity could be different sampling strategies, study designs, or assessments of psychopathology although we tried to limit the latter by only including studies using clinical diagnoses. The pooled prevalence rates should be interpreted in a way considering the lower and upper bounds of the confidence interval as compatible with the overall estimate. However, even if conservatively referring to the lower bound, the pooled prevalence estimates we found are higher than in the general population (Jacobi et al., Reference Jacobi, Höfler, Strehle, Mack, Gerschler, Scholl and Wittchen2014). This is in line with studies on depressive and anxiety disorders in patients with more common chronic conditions. Mental diseases in addition to a somatic disorder can negatively affect the course of the somatic disease and reduce quality of life (Cruz et al., Reference Cruz, de Almeida Fleck and Polanczyk2010; Lichtman et al., Reference Lichtman, Froelicher, Blumenthal, Carney, Doering, Frasure-Smith and Sheps2014; Müller-Tasch et al., Reference Müller-Tasch, Peters-Klimm, Schellberg, Holzapfel, Barth, Jünger and Herzog2007; Watkins et al., Reference Watkins, Koch, Sherwood, Blumenthal, Davidson, O'Connor and Sketch2013). Therefore, detecting and treating mental disorders in patients with rare chronic diseases is crucial to improve overall health and well-being.
To better understand which aspects may lead to increased psychopathology rates, we further investigated correlates of depression and anxiety. Different and partly contradictory patient-related, clinical, and psychosocial features were associated with increased psychopathology. Regarding some of the clinical correlates such as cognitive impairments or fatigue, it is unclear whether these are symptoms of the somatic disease that are associated with depression or rather symptoms of a depressive disorder itself. Due to the cross-sectional design of most studies, the direction of these relationships remains unclear. Moreover, some of the conditions included in this review may have a pathophysiological predisposition for affective or anxiety disorders. For instance, Huntington's disease causes degenerative cerebral changes, which can contribute to the development of depressive disorder (Naarding et al., Reference Naarding, Janzing, Eling, van der Werf and Kremer2009) and in spasmodic torticollis, a functional disturbance of the basal ganglia affects the limbic loop, likely resulting in mood disorders (Gündel et al., Reference Gündel, Wolf, Xidara, Busch, Ladwig, Jacobi and Ceballos-Baumann2003). In these cases, it can be difficult to differentiate whether the somatic predisposition or problems in adjusting to the disease cause psychopathological symptoms. Moreover, medication for the somatic disease can cause psychiatric symptoms as a side effect, e.g. steroids in sarcoidosis (Goracci et al., Reference Goracci, Fagiolini, Martinucci, Calossi, Rossi, Santomauro and Castrogiovanni2008). Overall, in some cases, it can be difficult to distinguish between somatic symptoms, side effects of medications and symptoms, or consequences of comorbid mental diseases. For healthcare providers, these distinctions may be difficult as well. Symptoms of mental disorders may be mistaken for physical symptoms, which could lead to an underestimation of psychological burden. To detect mental disorders in somatically ill patients, interdisciplinary cooperation, for example, through consultative services, or a systematic use of standardized screening instruments could be helpful. In three studies, the prevalence of affective or anxiety disorders was particularly high in early stages of the disease. This is in line with a qualitative study from our team, where patients described receiving the diagnosis as a life changing experience (Uhlenbusch, Löwe, & Depping, Reference Uhlenbusch, Löwe and Depping2019) and indicates, that the time right after diagnosis may be a particularly critical phase in which patients need particular support in adjusting to their disease.
In many studies, clinical symptoms were not associated with depression or anxiety. Besides clinical features, psychological processes can play a role in the development of mental disorders. One study showed that psychological features such as illness perceptions were better predictors of psychopathology than clinical features (Gündel et al., Reference Gündel, Wolf, Xidara, Busch and Ceballos-Baumann2001). This is in line with a cross-sectional study we conducted on depression and anxiety symptoms in patients with rare diseases, where disease-related aspects did not contribute to explained variation of depression and anxiety, while psychological features played a substantial role (Uhlenbusch et al., Reference Uhlenbusch, Löwe, Härter, Schramm, Weiler-Normann and Depping2019). This indicates that when addressing psychopathology, it may be adequate to provide healthcare, which is not tailored to the specific disease. This information is particularly useful in the field of rare diseases, where disease-specific support offers are hardly feasible due to the high number of different conditions.
Despite the rarity of the conditions, some authors succeeded at reaching large sample sizes. Most of these studies were cohort studies retrieving data from patient registries (Hedgeman et al., Reference Hedgeman, Ulrichsen, Carter, Kreher, Malobisky, Braun and Olsen2017; Jenkins-Jones et al., Reference Jenkins-Jones, Parviainen, Porter, Withe, Whitaker, Holden and Ross2018; Roos et al., Reference Roos, Mariosa, Ingre, Lundholm, Wirdefeldt, Roos and Fang2016), where medical information is organized and stored systematically. For instance, Denmark, Sweden, and other Nordic countries have nationwide registries with similar structures and personal identification numbers, which enable researchers to perform large cohort studies. This may be particularly useful in the field of rare diseases, where conducting adequately powered studies is challenging (Pai et al., Reference Pai, Yeung, Akl, Darzi, Hillis, Legault and Iorio2019). In two other studies (Schmitz-Hübsch et al., Reference Schmitz-Hübsch, Coudert, Tezenas du Montcel, Giunti, Labrum, Durr and Klockgether2011; Schneider et al., Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014), the authors attained large sample sizes by cooperating globally. Schneider et al. (Reference Schneider, Debbane, Bassett, Chow, Fung and van den Bree2014) recruited patients across 15 different centers, all part of the International Consortium on Brain and Behavior in 22q11.2 Deletion Syndrome (http://www.22q11-ibbc.org). Although collaborations of this form increase heterogeneity due to cultural variation or sampling differences, they could be a promising approach to strengthen evidence in the field of rare diseases.
A major strength of this study is the broad search considering all rare diseases listed in the orpha.net registry of rare diseases. A total of 34 402 studies were screened. However, due to the high number of records, many studies were excluded during the initial screening based on the information given in the title and abstract. This procedure enabled us to screen the high number of studies but we may have excluded potentially relevant studies for which the information in the abstract is inaccurate or incomplete. For the same reason, we did not update the database search, which is recommended in order to detect studies published during the time of data analysis (Eden, Levit, Berg, & Morton, Reference Eden, Levit, Berg and Morton2011). The resulting time gap between the end of the search and the publication must be noted as a limitation. The quality of assessed studies ranged widely and some studies fulfilled less than half of the criteria in the STROBE checklist. This is a potential source of bias and may affect the reliability of individual study results. However, a sensitivity analysis excluding studies with a quality of <40% scarcely changed the pooled prevalence estimates. Moreover, the STROBE checklist is a guideline for reporting observational studies and it is not always clear whether an aspect was not reported or not performed. Some items further addressed specific analyses (e.g. sub-group or sensitivity analyses), which may have been beyond the scope of some studies. We rated ‘not fulfilled’ in all of these cases, which may result in a stricter assessment and an underestimation of the studies' quality. The current study aimed at complementing survey-based research on symptom burden in patients with rare diseases. Hence, we only included studies that used clinical diagnoses or structured clinical interviews. This allowed us to investigate clinically relevant affective and anxiety disorders and aimed to reduce heterogeneity. However, as we excluded studies solely based on questionnaires, the results do not provide a comprehensive representation of all research on psychopathology in rare diseases. Considering studies using self-report questionnaires may have resulted in a broader range of different rare diseases. Large studies on depression and anxiety used standardized questionnaires, for instance the International Depression Epidemiological Study by Quittner et al. (Reference Quittner, Goldbeck, Abbott, Duff, Lambrecht, Solé and Barker2014), who included more than 6000 patients with the rare disease cystic fibrosis across nine countries. More recent surveys investigated depression and anxiety in samples of patients with differing rare diseases in Germany (Uhlenbusch et al., Reference Uhlenbusch, Löwe, Härter, Schramm, Weiler-Normann and Depping2019) and the USA (Bogart & Dermody, Reference Bogart and Dermody2020). A further limitation lies in the fact that most of the included studies had a non-experimental, cross-sectional design and no conclusions can be drawn about causal relationships. Finally, the heterogeneity between but also within diseases is high and should be considered when interpreting the results.
In conclusion, this is the first systematic review on clinically diagnosed affective and anxiety disorders in patients with different rare diseases. We synthesized data on prevalence and correlates of psychopathology and found widely ranging prevalence rates and different, partly contradictory features to be associated with depression and anxiety. Disregarding the heterogeneity of different studies, pooled prevalence estimates showed that high percentages of patients across different rare diseases are affected by affective and anxiety disorders. Considering that the majority of rare diseases are not curable, early detecting and treating mental disorders can be critical in order to maintain and improve general health and well-being in patients with rare diseases.
Despite our broad search strategy considering all rare diseases listed in the orpha.net registry of rare diseases, only 24 different conditions were included, representing only a fraction of the estimated 7000 different rare diseases worldwide. This indicates that evidence on this topic still lacks a vast majority of rare diseases. Conducting studies in this area could be facilitated by building networks and research collaborations across sites.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721003792.
Acknowledgements
There was no funding source for this study.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.