Introduction
For healthcare professionals, palliative care is an interdisciplinary approach to provide the best available care and support (Vanderhaeghen et al., Reference Vanderhaeghen, Bossuyt and Opdebeeck2018). The approach enables patients and next-of-kin to be involved in the care process and decision-making, with communication and interpersonal relationships being cornerstones in this. A number of areas for improvement in palliative end-of-life (EOL) care have been identified in Sweden. These areas relate to the assessment of oral health and pain, and the prescription of anti-anxiety drugs and opioids for pain, pressure ulcer management and EOL discussions (The Swedish National Board of Health and Welfare [SNBHW], 2017).
Early integration of palliative care is highlighted (van der Steen et al., Reference van der Steen, Radbruch and Hertogh2013) and may contribute to successful EOL discussions with patients and next-of-kin. During such discussions, important issues related to symptoms, emotions, and existential issues should be discussed continuously and in a timely manner (Udo et al., Reference Udo, Lövgren and Lundquist2017; Hagan Thomas et al., Reference Hagan Thomas, Jackson and Carlson2019). Guidelines emphasize that all patients are entitled to information and opportunities for discussion during the care process, e.g., about transitioning from curative treatment to increased focus on palliative care and on a late palliative phase when imminent death is expected (Palliative Care Competence Framework Steering Group, 2014). These discussions with a patient and next-of-kin are similar to advanced care planning and include information, care planning and discussions about prognosis, goals of care, consent to treatment, and EOL decision-making (Sekse et al., Reference Sekse, Hunskår and Ellingsen2018).
The majority of patients with progressive cancer think that it is the physician's responsibility to initiate EOL discussions (Bergenholtz et al., Reference Bergenholtz, Timm and Missel2019). Discussions should be interdisciplinary, with a registered nurse present to provide person-centered care supporting the patient and minimize concerns and misunderstandings (Anderson et al., Reference Anderson, Bloch and Armstrong2019).
Barriers to EOL discussions include lack of time and privacy, lack of training, poor timing and readiness, prognostic uncertainty, and the fear of initiating EOL discussions (Udo et al., Reference Udo, Lövgren and Lundquist2017; Doubal et al., Reference Doubal, Cowey and Bailey2018; Sekse et al., Reference Sekse, Hunskår and Ellingsen2018). In a retrospective record review in nursing homes, it was found that EOL discussions with patients were not documented in any of the 100 patient records included. However, next-of-kin were informed about deterioration and what to expect in the near future (Høgsnes et al., Reference Høgsnes, Danielson and Norbergh2016).
In recent years, the trend has been that EOL discussions have increased in frequency, but this differs between diagnoses and age groups (Martinsson et al., Reference Martinsson, Fürst and Lundström2012). Old age may be a risk of not having EOL discussions (Lindskog et al., Reference Lindskog, Tavelin and Lundstrom2015). Which people are considered “old” is a complex and multidimensional judgment, but may be related to when a person is entitled to state pensions (United Nations, 2012). There are also geographical differences, despite EOL discussions being considered important and recommended in national guidelines (SNBHW, 2016).
The goal of having a national register like the SRPC is to enable scrutinization of palliative care. The register contains rich nationwide data from various care and geographical settings. The SRPC comprises information about several aspects of palliative care, including EOL discussions, that facilitate evaluations and enable healthcare institutions’ follow-up of quality of care as well as research based on the register data (Lindskog et al., Reference Lindskog, Tavelin and Lundstrom2015; Elmstedt et al., Reference Elmstedt, Mogensen and Hallmans2019; Lövgren et al., Reference Lövgren, Melin-Johansson and Udo2019).
To ensure equal and high-quality palliative care where information is communicated with the patients and next-of-kin, it is important to continue the efforts to systemize EOL discussions. Therefore, the aim of this study was to explore the proportion of adult patients and next-of-kin who, according to the SRPC, had or did not have EOL discussions, and associated factors.
Methods
Design and study population
This nationwide register study was based on data from the SRPC database. It included all deaths in Sweden that were reported to the register during 2015–2017 (n = 177,921). The SRPC covered 55–66% of all deaths in Sweden during these 3 years (2015: 66%; 2016: 64%, 2017: 55%). This study is a part of a larger project about communication in palliative care in collaboration between Ersta Sköndal Bräcke University College, Dalarna University, and Mid Sweden University.
Measurement
The SRPC comprises information about various aspects of palliative care and a questionnaire with 29 items that has been created specifically for the register based on the register was used in this study (Lundström et al., Reference Lundström, Axelsson and Heedman2012). Data are reported to the register by healthcare staff and are voluntary. The findings should be applicable in clinical praxis. In this paper, the following data were used: patient age, sex, diagnosis, place of death, if there was a documented decision by the physician that care be shifted to EOL care (yes/no), how long before death the person lost the ability to express his or her will and participate in decisions about the content of medical care, if the person had an individually adapted and documented EOL discussion that he/she was in the final stages of life and that the care was focused on the quality of life and symptom relief (yes/no), and if the person's next-of-kin had an individually adapted and documented EOL discussion that the person was in the final stages of life and that the care was focused on the quality of life and symptom relief (yes/no).
Data analysis
Descriptive statistics using IBM SPSS statistics version 25 with mean, median, max–min, and standard deviation (SD) values for continuous variables, such as age (years), sex (male/female), diagnosis (cancer, heart disease, multiple diseases, dementia, lung disease, and stroke), place of death (hospital, nursing home, home, specialized inpatient palliative care unit, or other place), and percentages for categories were compiled for this study, as well as the proportion of patients and next-of-kin having had an EOL discussion. The outcomes were analyzed with two logistic regressions (enter method) with patients having had an EOL discussion and next-of-kin having had an EOL discussion, respectively, as the dependent variable. Predictors, including age, sex, diagnosis, place of death, if a physician had assessed that care be shifted to EOL care (yes/no), and how long before death the patient lost the ability to make decisions about the content of medical care (maintained, hours, days, weeks, and months), were documented. The relative risks were estimated using odds ratios with 95% confidence intervals.
Ethical considerations
The study followed the ethical principles of the Helsinki Declaration (Helsinki Declaration, 1964) and was approved by the Ethics Review Board in Stockholm, Sweden (Dnr: 2019–02617).
Results
Sociodemographic characteristics
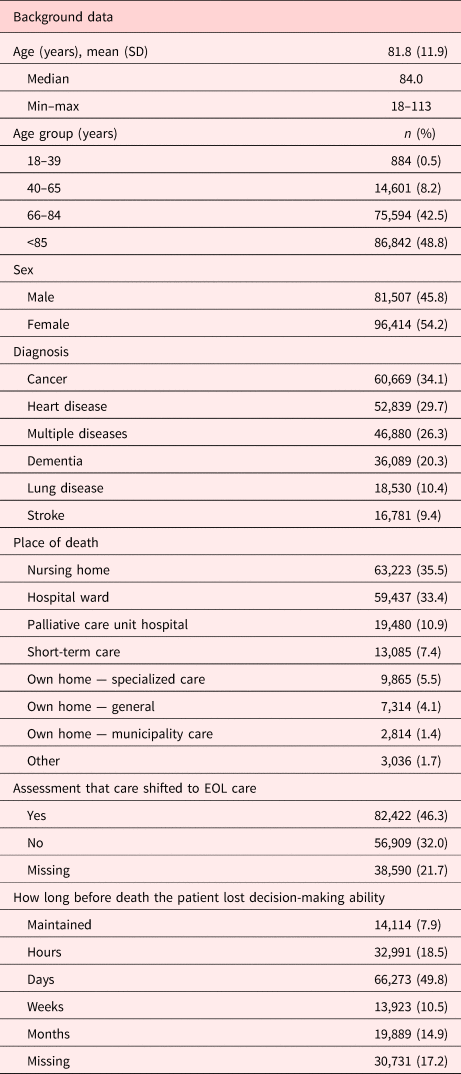
The mean age in the sample was 81.8 years (median age 84); the youngest person was 18 years and the oldest 113 years. A majority were over 85 years of age and female. The most common diagnoses were cancer, heart disease, lung disease, multiple diseases, dementia, and stroke. Most patients died in a nursing home or hospital, with only a small proportion of the patients having died at home. A majority of the patients were still able to make decisions about the medical care content days before death and were informed about the transition to EOL care (Table 1).
Table 1. Patients’ sociodemographic characteristics (N = 177,921)
EOL discussion and associated factors
Less than half (34%) of the patients had not had a documented EOL discussion with a physician in the last days of life (Figure 1). The corresponding figure for next-of kin was 14% (Figure 2).
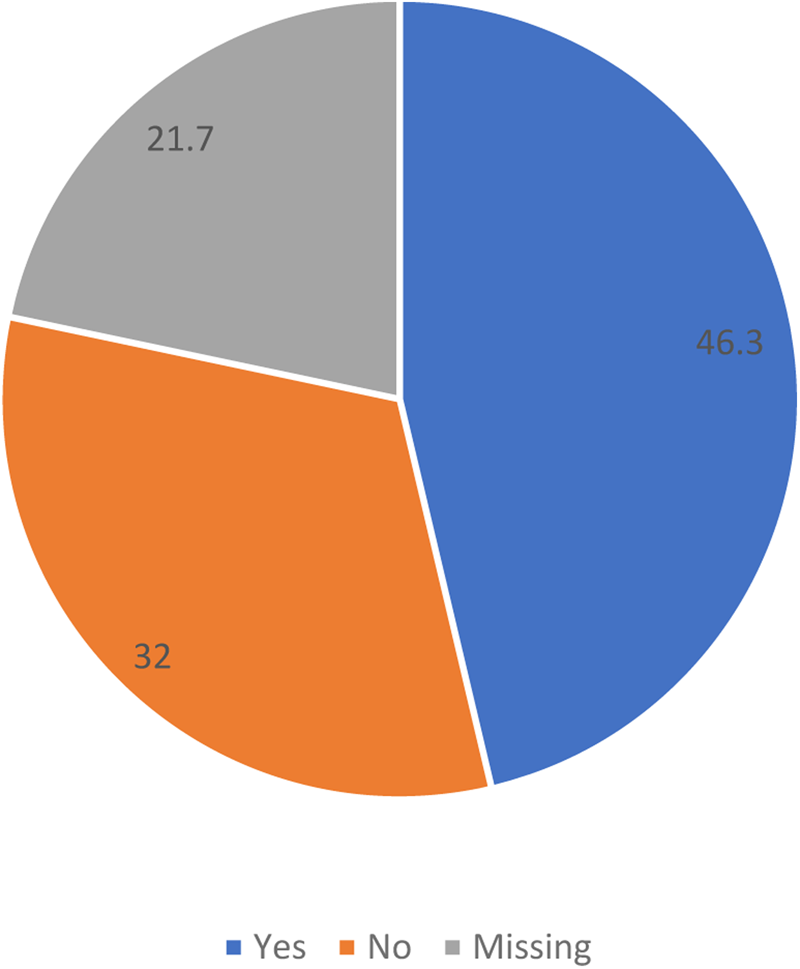
Fig. 1. Proportion of patients with EOL discussions in the years 2015–2017.
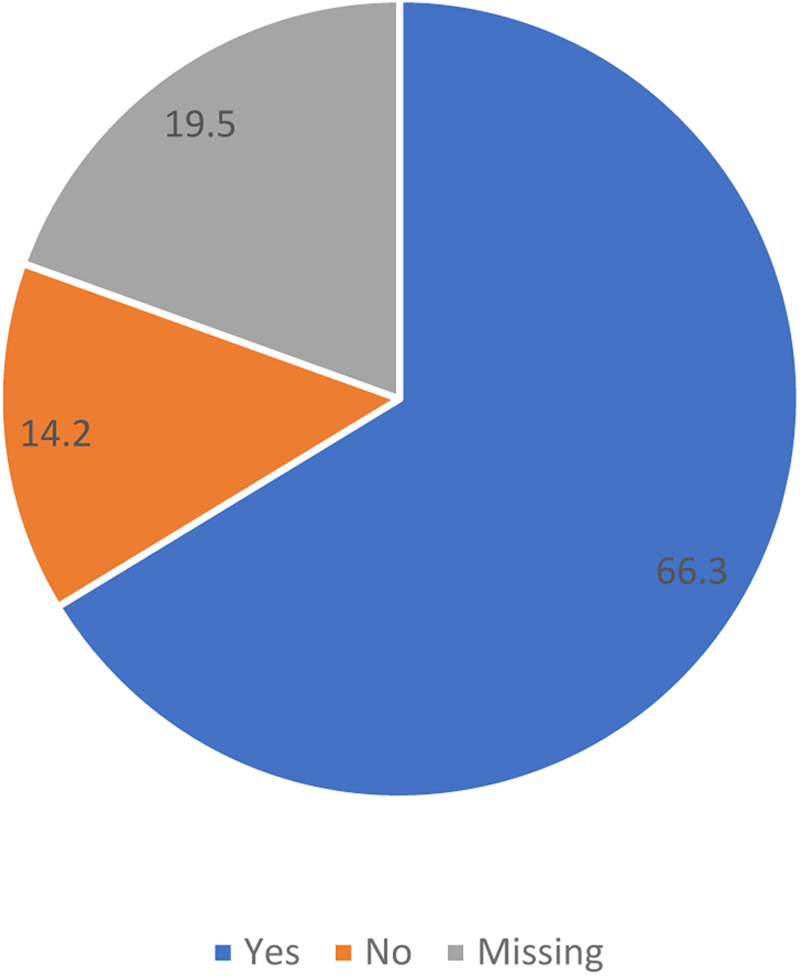
Fig. 2. Proportion of next-of-kin with EOL discussions in the years 2015–2017.
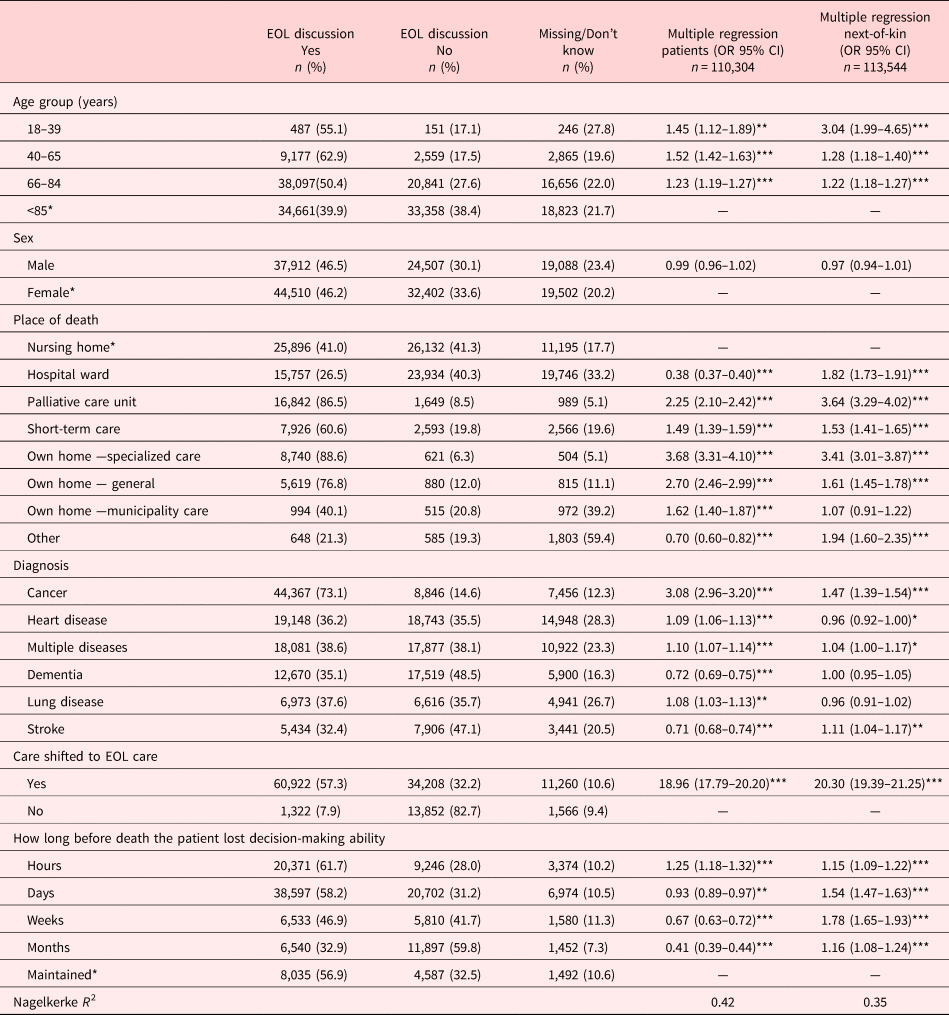
Almost half of the patients and a majority of the next-of-kin had an EOL discussion with a physician (46% vs. 66%). According to the logistic regression analysis (Table 2), patients who had not had an EOL discussion were predicted by older age, diagnosis (dementia or stroke), and place of death (dying in the hospital).
Table 2. Patients with/without EOL discussions and multivariate associations between patient-/care-related factors and EOL discussions with patients and next-of-kin, respectively
* p < 0.05.
** p < 0.01.
*** p < 0.001.
Those who lost their ability to make decisions months before death were more likely not to have had an EOL discussion, as were those who did not have a documented decision that care be shifted to EOL care. Compared with dying at a nursing home, there were several places of death that were significant predictors of having had an EOL discussion. The strongest predictors of having had an EOL discussion were dying at home with support from specialized palliative home care or dying at a palliative care unit, if it was documented in the patient's record that care had shifted to EOL care, and if the patient had cancer. Next-of-kin who had not had an EOL discussion were predicted by older age of the patient, diagnosis (heart disease or lung disease), no documented decision that care be shifted to EOL care, and place of death (own home with municipality care or short-term care). The strongest predictor of the next-of-kin having had an EOL discussion was that care had shifted to EOL care. Of the diagnoses, cancer was the strongest predictor of next-of-kin having had an EOL discussion.
Discussion
The proportions of adult patients and next-of-kin who do not have an EOL discussion and associated factors are relatively unknown. Our study included 177,921 registrations in the SRPC of patients who died during the period 2015–2017. Based on this extensive data, fewer of the patients who had EOL discussions were older and female, diagnosed with dementia or stroke, and cared for in a nursing home or hospital. A larger proportion of the patients and next-of-kin who had EOL discussions had cancer or had a decision made by their physician that care be shifted to EOL care documented in their patient record.
Our study confirmed previous findings that EOL discussions are not implemented in all care contexts and are not provided to patients on equal terms. Adequate and consistent documentation related to EOL care goals and decision-making has an impact on the quality of care, including EOL discussions (Bloomer et al., Reference Bloomer, Botti and Runacres2018). This was particularly apparent in the present study among older patients diagnosed with stroke or dementia, who died in a nursing home or hospital, or if the shift to EOL care was undocumented. Previous register-based studies show that patients with lung disease in specialist palliative care had EOL discussions more often than those in nursing homes (Henoch et al., Reference Henoch, Strang and Löfdahl2019). It has also been reported that a documented EOL discussion is a factor that relieves symptoms for persons cared for in nursing homes and their next-of-kin (Andersson et al., Reference Andersson, Årestedt and Lindqvist2018). On the other hand, having EOL discussions is not more common in regions with fully developed palliative care compared with regions with less developed palliative care (Schelin et al., Reference Schelin, Sallerfors and Rasmussen2018). This support the importance of improving palliative care including EOL discussions in, for example, nursing home settings (Smedbäck et al., Reference Smedbäck, Öhlén and Årestedt2017). Significantly fewer EOL discussions were held with patients with an incurable illness in their last week of life during the COVID-19 pandemic in 2020 compared with 2019 (Strang et al., Reference Strang, Bergström and Martinsson2020), which further increased inequality.
Old age is a predictor for not having EOL discussions, and for patients and next-of-kin not getting information about imminent death (Lindskog et al., Reference Lindskog, Tavelin and Lundstrom2015). This is particularly common if the older person has dementia, is dying in hospital (Martinsson et al., Reference Martinsson, Lundström and Sundelöf2020), and has difficulties understanding the prognosis or limitations of life support care (Ethier et al., Reference Ethier, Paramsothy and You2018). Although evidence is limited, studies have shown that persons with dementia are a neglected group when it comes to palliative care, including EOL discussions (Ngo and Holroyd-Leduc, Reference Ngo and Holroyd-Leduc2015; Erel et al., Reference Erel, Marcus and Dekeyser-Ganz2017; Piers et al., Reference Piers, Albers and Gilissen2018); there is increased recognition of their need and eligibility for such care (Erel et al., Reference Erel, Marcus and Dekeyser-Ganz2017). This makes the presence of next-of-kin, and their role in the communication process, even more important (Ngo and Holroyd-Leduc, Reference Ngo and Holroyd-Leduc2015). The lack of EOL discussions for dying persons with dementia suggests that the EOL discussion process and advanced care planning should be initiated at an earlier stage with persons with dementia and next-of-kin, to better prepare them for EOL care. If information is given early on, these persons would most likely be able to receive the information about EOL issues and participate in the communication process, despite illness progression.
EOL discussions are of most importance to patients when receiving appropriate symptom management and to avoid unnecessary hospitalization or treatment against the person's preferences and wishes (Jethwa and Onalaja, Reference Jethwa and Onalaja2015). Considering that persons with dementia may not have the cognitive ability to discuss EOL plans (Brooke and Kirk, Reference Brooke and Kirk2014), emphasis should be on how to support staff to achieve successful EOL discussions where next-of-kin are included — not on if it should be done (Høgsnes et al., Reference Høgsnes, Melin-Johansson and Norbergh2014). Information and communication to next-of-kin is crucial both for their own well-being and for making informed decisions in the best interests of their loved ones (Dening et al., Reference Dening, King and Jones2017; Bosisio et al., Reference Bosisio, Jox and Jones2018). Applying a palliative care philosophy in nursing homes may support a next-of-kin's existential life situation, which often becomes more difficult after their loved one has been relocated to a nursing home (Brooke and Kirk, Reference Brooke and Kirk2014; Høgsnes et al., Reference Høgsnes, Melin-Johansson and Norbergh2014). Person-centered care may not be enough for older persons, especially when diagnosed with dementia, making the family's role vital (Feinberg, Reference Feinberg2014). Family-centered care including a wider family network has been suggested as beneficial in palliative care for persons with dementia (Broady et al., Reference Broady, Saich and Hinton2018; Hao and Ruggiano, Reference Hao and Ruggiano2020). This approach is widely used in pediatric care, and there is now a growing interest in implementing family-centered care also in adult care for the most vulnerable (Feinberg, Reference Feinberg2014; Hao and Ruggiano, Reference Hao and Ruggiano2020).
Limitations of the study
This retrospective nationwide registry study contributes knowledge about factors influencing EOL discussions. The strengths are that it included all deaths in Sweden reported to the SPCR during 2015–2017, and specifies the proportion of EOL discussions provided to patients and next of kin. However, underlying factors as geographical locations are not examined, and that the palliative care knowledge and competence among professionals is unknown might have an impact on factors associated with EOL discussions. Furthermore, staff who register data in the SRPC have varying knowledge about the patients’ last days of life, and data should therefore be interpreted with caution.
Conclusion and clinical implications
Despite the benefits of timely communication about EOL care, dying patients do not have equal access to communication about EOL issues. Though not all patients and next-of-kin may wish to participate in EOL discussions, they must still be invited and given the opportunity to choose, as part of high-quality palliative care. Our extensive nationwide data supported previous findings that EOL discussions seem to be a challenge, as they are not equally and systematically implemented in all care settings and to all patients, regardless of diagnosis or age. Based on the results in this study, further efforts must be made, so that neglected patients and next of-kin can receive the EOL discussions they are entitled to, on equal terms.
Funding statement
Mid Sweden University and Ersta Sköndal Bräcke University College provided financial support for publication of this article.
Conflicts of interest
None declared.









